Playlist
Show Playlist
Hide Playlist
Post-inflammatory Hyperpigmentation (PIH) in Darker Skin
-
Slides Post-inflammatory Hyperpigmentation PIH in Darker Skin.pdf
-
Download Lecture Overview
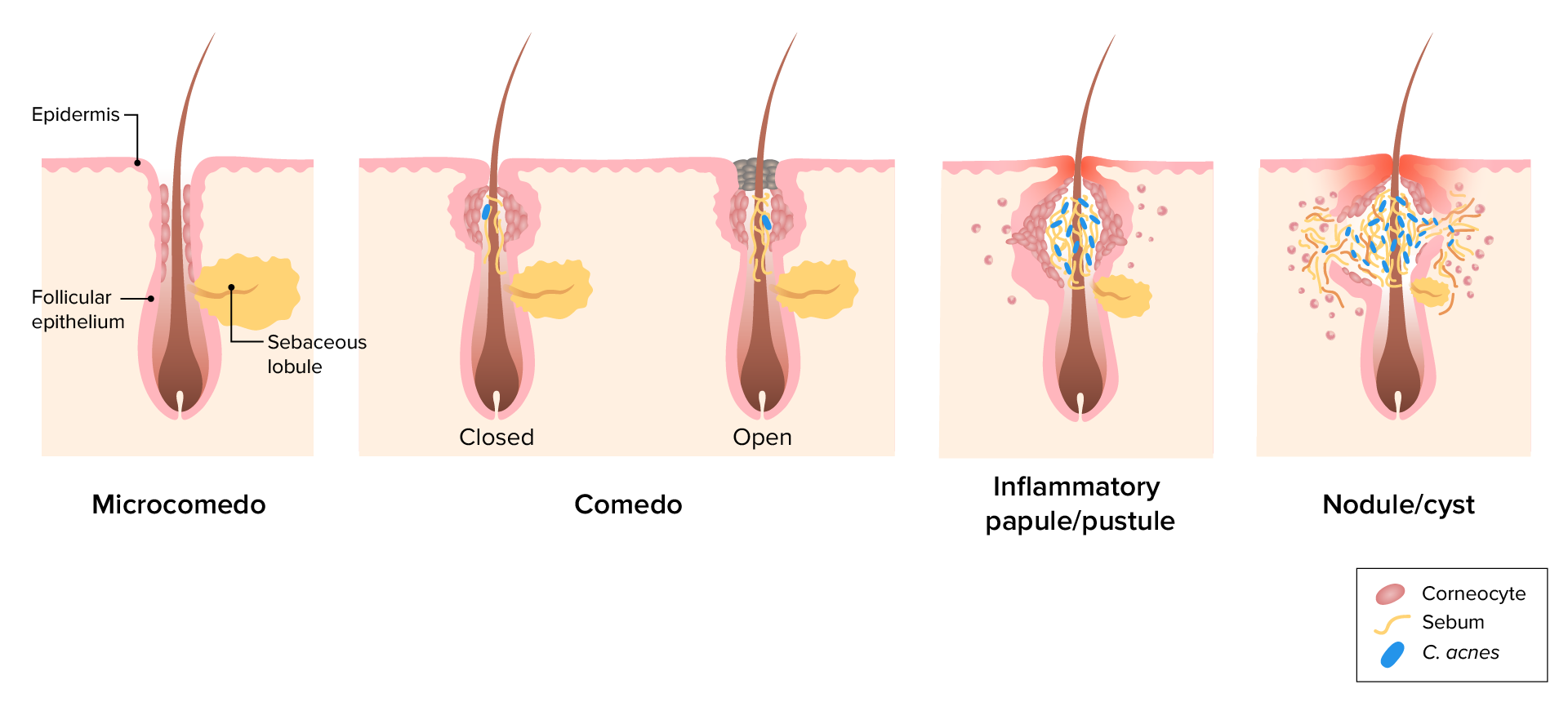
00:01 Welcome to our lecture on Post-inflammatory hyperpigmentation or PIH. 00:08 Post-inflammatory hyperpigmentation or PA is also known as post-inflammatory melanosis. 00:15 It's reactive pigmentation of the skin that occurs as a sequela of cutaneous inflammation. 00:23 So what is the epidemiology of this condition? It occurs at any age with equal incidence in both males and females. 00:34 Individuals with skin phototypes 3 to 6 are more likely to develop PIH compared to lesser Fitzpatrick photo skin types. 00:46 So what are the causes of PIH? Firstly, it could be due to infections, for example dermatophytosis or viral infections, allergic reactions, for example contact dermatitis or reactions from insect bites, what we call papular urticaria, which is very common in patients of African ancestry. Inflammatory papulosquamous disease like psoriasis, eczema, and lichen planus can also cause post-inflammatory hyperpigmentation, particularly lichen planus, which is why we have to be aggressive when we treat lichen planus to minimize the inflammation. 01:26 Drug reactions can also cause post-inflammatory pigmentation, for example, Stevens-Johnson syndrome, toxic epidermal necrolysis, which is TN and fixed drug eruption (FD), which we'll talk about later in our subsequent lectures. Cutaneous injury of whatever cause irritants, burns, or cosmetic procedures. 01:49 A lot of people do cosmetic procedures these days, and things like chemical peels and dermabrasion, etc. 01:55 can actually cause a PIH these also cause pain, particularly acne. 02:02 Acne is one of the most common conditions that we see, and it is one of the most causes of PIH. 02:08 More so again in skin phototypes 4 to 6 Pseudofolliculitis Barbae, which we see mainly in males, African males, is a common inflammatory condition in dark skin, and in 50 to 80% of cases it is almost always followed by post-inflammatory hyperpigmentation. So how does this happen. 02:33 We're looking at pathophysiology is the inflammation in the epidermis which stimulates melanocytes. Then the melanocytes increase in the production of melanin. 02:42 Then melanin is transferred to surrounding keratinocytes leading to epidermal melanosis. 02:50 In the basal layer if it is injured by whatever trigger then melanin can enter the papillary dermis and whilst it's in the papillary dermis, melanin is then trapped by macrophages, resulting in a deeper deposition of melanin. 03:07 So there are two types of melanosis. 03:11 There's epidermal and dermal melanosis. 03:14 So looking at epidermal melanosis. 03:16 Patients tend to present with dark brown or tan macules or patches. 03:22 If the pigmentation is deep in the in the dermis more lower part of the dermis, then one gets dark gray or blue gray hues. 03:31 The pigmentation is usually located on the previous site of inflammation. 03:35 So the following we're going to look through the examples of post-inflammatory hyperpigmentation following various causes. 03:43 As I mentioned, acne is one of the most common inflammatory conditions that we see, and it is not surprising that PIH is seen in this condition. 03:53 So you can see a dark skinned patient, probably for the skin type fitzpatrick five with pigmentation. The acne seems to have cleared, but there's residual pigmentation on the different areas of the face. What about contact dermatitis? I'm reminded of this patient, actually, who came to see me about four years ago, who had gone to a beautician to do chemical peels because she wanted to look nicer and brighter and glowing. And unfortunately, they use the incorrect peel for her. 04:27 And she developed inflammation and excoriations. 04:30 And that led to the irregular pigmentation that you can see on the cheeks. 04:35 It was quite devastating for her. 04:38 However, we were able to treat her. 04:41 Another cause of age is atopic dermatitis, which is, of course, another common condition that we see in dermatology clinics. 04:50 So there's inflammation you can see. 04:53 And this inflammation is quite aggressive. 04:55 You can see the hyperpigmentation on the flexural areas. 04:58 And then there's also excoriations when patients tend to scratch or rub on the lesions. 05:04 There's that triggers more inflammation and more pigmentation. 05:08 And you can see that in black patients besides treating the condition itself you have to also focus on the post-inflammatory hyperpigmentation. 05:19 This is a patient who had retroviral disease, was started on a antibiotics and developed a drug reaction. It was quite an extensive drug reaction. 05:32 It was a themata. And this is a post-inflammatory hyperpigmentation that you see post the drug reaction. So it's important to note that although the drug reaction is cleared, the PIH remains a challenge for the patient. 05:44 You can see the irregular patches and macules all over the front and back. 05:51 Another common condition that we see mainly in males is what we call pseudofolliculitis barbae, and this tends to follow shaving of the beard. 06:00 Some males have got a genetic predisposition to developing lumps and pimples and papules after shaving the beard. We will talk about this condition as well later on. 06:11 You can see the papules and pigmentation around the areas of inflammation. 06:16 So how do we diagnose post-inflammatory hyperpigmentation? It's usually based on the history and in the history the patient will relate to some inflammatory disorder or accidental or iatrogenic skin injury. 06:31 Physical examination is also important. 06:33 And we can also use Wood's lamp to try and distinguish between epidermal and dermal melanosis. Sometimes it's not easy, but sometimes it helps for us to see how deep the pigmentation is. So if it's epidermal, it's usually well-circumscribed pigmentation with accentuated borders. When it's dermal, this poorly circumscribed and not accentuated under Wood's lamp. So the Wood's lamp can assist us to differentiate between epidermal and dermal. 07:03 So what else can confuse us between PIH and other conditions? Melasma. Melasma is most commonly seen in women of reproductive age. 07:16 And you see this is a typical patient who was on hormonal contraceptives and of course developed melasma. So it's completely different from PIH. 07:25 There's no preceding inflammation and it just happens on its own. 07:31 This is another condition. 07:33 In fact, this is a young patient that I saw a couple of years ago. 07:39 And she came to me saying that she's getting darker on the face and she wasn't aware what was causing the the darkness. 07:48 And he was actually shocked to hear that this is a condition caused by basically overeating. 07:55 The patient was overweight and this is what we call acanthosis nigricans, which are slightly elevated plaques associated with obesity and sometimes with diabetes mellitus. 08:05 So the patient was advised to lose weight, see a dietician and reduce the food intake. 08:11 And most of the time this can clear if it's due to obesity. 08:15 Another differential is tinea versicolor, which we spoke about, which can also present with hyperpigmentation in some patients. 08:23 In other patients, interestingly, it can present with deep pigmentation hyperpigmentation. But we can't tell how the patient will respond to this fungus. 08:33 So this can also confuse us with PIH. 08:39 So how do we treat the patients with PIH? As I mentioned, we try to identify the cause and general measures include photoprotection , use of a broad spectrum sun protection factor of at least more than 30, and it must be applied to the entire affected area. 08:59 Photo protection won't clear the PIH, but it will minimize it and assist with the active management. We use a number of topical pigmenting agents like hydroquinone, azelaic acid, kojic acid, retinoids, arbutin, niacinamide, and other topical agents. 09:19 A physical option also can be used, for example, chemical pills in the right hands, to the right concentration with somebody who knows how to use them, and of course, laser treatments, IPL and Q-switched lasers for others. 09:32 So this is an example of a patient who developed PIH post chemical peel and another one after acne. 09:39 And they both responded well to topical treatment.
About the Lecture
The lecture Post-inflammatory Hyperpigmentation (PIH) in Darker Skin by Ncoza Dlova is from the course Hyper- and Hypopigmentation Skin Disorders.
Included Quiz Questions
Which Fitzpatrick skin types are most likely to develop post-inflammatory hyperpigmentation?
- Types III to VI
- Types I and II only
- Types V and VI only
- Types I to III
- Types II to IV
What is the mechanism that leads to dermal melanosis in PIH?
- Melanin enters the papillary dermis and becomes trapped by macrophages
- Melanocytes migrate into the dermis and produce excess melanin
- Keratinocytes trap excess melanin released by melanocytes
- Inflammation directly stimulates dermal melanin production
- Epidermal melanin naturally descends into the dermis over time
Which clinical finding helps distinguish epidermal from dermal PIH under Wood's lamp examination?
- Epidermal PIH shows well-circumscribed borders with accentuation
- Dermal PIH shows fluorescence under the lamp
- Both types show similar enhancement patterns
- Epidermal PIH shows poorly-circumscribed borders
- Neither type shows any change under Wood's lamp
Which statement regarding sun protection in PIH management is correct?
- It prevents worsening but won't clear existing PIH
- It completely resolves existing PIH within weeks
- It is only necessary for facial PIH
- It should only be used during active inflammation
- It is not necessary for darker skin types
In patients of African descent with pseudofolliculitis barbae, what percentage typically develops PIH?
- 50-80%
- 10-20%
- 30-40%
- > 90%
- > 5%
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |