Playlist
Show Playlist
Hide Playlist
Lichen Planus in Darker Skin: Epidemiology, Presentation, and Management
-
Slides Lichen Planus in Darker Skin.pdf
-
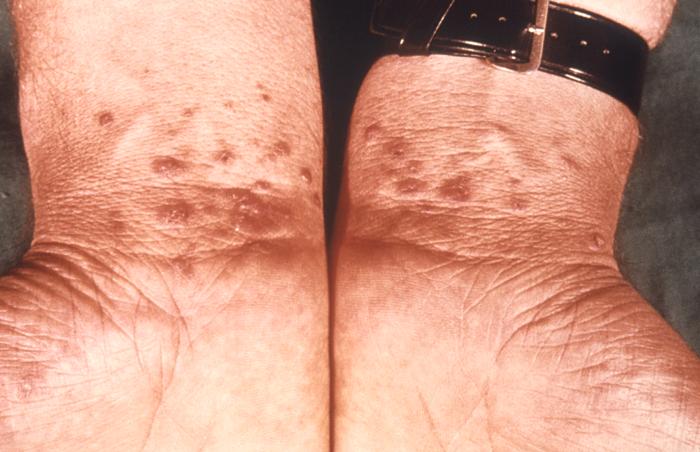
Download Lecture Overview
00:01 Welcome to our lecture on lichen planus. 00:05 So what is lichen planus? It is a chronic inflammatory skin condition that affects the skin, hair, nails, mouth and genitalia. 00:18 So if we look at the epidemiology of lichen planus, it affects approximately 1% of the population worldwide. It usually occurs in adults between the age of 30 and 60 years. 00:31 The etiology of lichen planus is unknown. 00:34 So what are the causes of lichen planus? It's a T cell mediated inflammatory disorder of unknown etiology. 00:44 Although unknown, some contributing factors have been identified. 00:50 And some of those contributing factors include genetic predisposition, physical and emotional stress, injury to the skin, and some drugs have been implicated, for example, antihypertensive drugs and some anti-TB drugs. 01:10 Lichen planus presents in six different ways. 01:14 It can be. Cutaneous lichen planus, mucosa lichen planus, for example, if it involves the oral or genital areas, lichen planopilaris, pilaris refers to hair, if it affects the hair, nail lichen planus and lichen planus pigmentosus, when you have involvement of the face or sun-exposed areas, then one can also get a lichenoid drug reaction. 01:42 So let's focus on cutaneous lichen planus. 01:46 It presents with papules and polygonal plaques which are shiny, flat topped, and firm. One can also observe fine white lines called Wickham striae, and these are usually seen in the mucosal areas. 02:04 The common signs that are affected with lichen planus are the front of the wrists, the palmar areas, the predilection for the extensor, the knees and ankles, and the lower back. 02:16 The distribution of lichen planus, it tends to present with scattered lesions. 02:22 Sometimes they may be clustered. 02:25 It may be linear, annular. 02:30 So what's the differential of lichen planus? Psoriasis is one of the most common differentials for lichen planus, but typically it appears as raised patches covered with scales. 02:44 Lichen simplex chronicus. This is another differential for lichen planus. 02:49 Lesions are usually appear in areas that are easily accessible for scratching. 02:56 Moving on to oral lichen planus. 02:58 These are the Wickham striae that I was referring to previously. 03:02 Usually presents as painless white streaks in a lacy pattern of fan like pattern in the mouth. 03:09 One can also observe this in the genital area. 03:14 Leukoplakia is another differential for oral lichen planus, and here you see white thickened patches on the oral mucosa. 03:24 Oral candida is a most common differential for lichen planus, and this can be associated with HIV or diabetes or immunocompromised patients. 03:36 Moving on to lichen planopilaris, which is lichen planus involving the hair. 03:42 You can see these tiny red, spiny follicular papules spreading across smooth areas of the scalp, and it could be on any hair-bearing area in the axillae as well as on the body involving the villa's hair. 03:58 So what is the differential of lichen planopilaris? Alopecia areata. You normally have well-demarcated round or oval patches of hair loss. 04:09 Tinea capitis usually occurs in children. 04:12 It's a dermatophyte infection of the scalp involving both skin and hair. 04:16 You see round, scaly lesions with broken hairs on the scalp. 04:23 Nail lichen planus is another clinical variant of lichen planus. 04:27 One can get one or more nails affected. 04:30 The nails are thin, grooved, or ridged. 04:32 The nail discoloration is quite prominent. 04:35 Nail pitting and onycholysis can also be present when all the nails are involve, we call it a 20 nail dystrophy. 04:43 However, lichen planus is not the only cause of 20 nail dystrophy. 04:47 Even alopecia areata can cause it. 04:51 So what is the differential for nail lichen planus. 04:53 Nail psoriasis where you also get pitting, onycholysis, oil drop sign and subungual hyperkeratosis. 05:01 So some of these features that you see in psoriasis, you don't see in lichen planus. 05:05 Onychomycosis, which is fungal infection of the nails, can also be listed as a differential for lichen planus. 05:15 The next variant is lichen planus pigmentosus. 05:18 It's an ill-defined oval grayish brown marks that you see mainly on sun-exposed areas on the face and the exposed areas of the arms. 05:29 It starts on the face and neck and spreads to the upper extremities and trunk. 05:34 The pigmentation can be diffuse. 05:36 It can be reticulate, lacy, blotchy, or perifollicular. 05:43 Lichen planus pigmentosa can be easily confused with post-inflammatory hyperpigmentation, which typically arises after a prior skin disorder or injury. 05:54 Melasma can also be confused with lichen planus pigmentosa, but the history, distribution, and clinical presentation will assist you. 06:06 How do we diagnose lichen planus? Basically on history and physical examination. 06:11 And most oftentimes we may have to do a biopsy in such patients because it can be sometimes difficult to differentiate from the other skin conditions that I have mentioned like psoriasis, eczema, fungal infections. 06:26 So on histology, these are some of the features that one would appreciate which are typical of lichen planopilaris. How do we treat patients with lichen planus? There's general measures. Avoid soaps and shower gels, which will exacerbate scaling because it can cause sensitivity of the skin. 06:47 Use good emollients that are moisturizing. 06:50 Sedating antihistamines are also recommended for patients with itchy skin. 06:56 The specific treatment involves a treatment plan, which should be in place to mitigate the risk of post-inflammatory hyperpigmentation. 07:05 This is more so in patients with skin of color. 07:09 Management of pruritis is crucial because each can be unbearable for patients. 07:15 Potent topical steroids are used, but bearing in mind that one has to monitor the side effects, for example, skin thinning and infections. 07:25 Topical calcineurin inhibitors have also been used. 07:30 Topical retinoids are another option, as we know in medicine, when there are many options for treating a condition, it means it's very difficult to treat that condition. 07:39 So we spoke about the use of retinoids for localized disease. 07:44 Now we're going to talk about widespread cases or severe localized disease and how we treat it? So the first option is to use systemic corticosteroids, for example, prednisone, which is usually used for 1 to 3 for 2 to 3 months. 08:00 And this is particularly crucial for skin of color because we want to be aggressive and minimize the inflammation so that we can minimize the post-inflammatory hyperpigmentation. 08:11 We can also use retinoids like acitretin hydroxychloroquine. 08:16 We need to be a little careful with hydroxychloroquine because it can also cause an idiosyncratic hyperpigmentation. 08:23 So if the patient's pigmentation gets worse, we need to be aware of the fact that it could be due to chloroquine. Methotrexate has also been used to treat extensive lichen planus. 08:36 And those are the systemic ways of treating lichen planus.
About the Lecture
The lecture Lichen Planus in Darker Skin: Epidemiology, Presentation, and Management by Ncoza Dlova is from the course Inflammatory Diseases in Patients with Darker Skin.
Included Quiz Questions
Which clinical finding is characteristic of oral lichen planus and helps distinguish it from other oral lesions?
- Painless white streaks in a lacy or fern-like pattern
- Painful thick yellow plaques with ulceration
- Painful round ulcers with red borders
- Painless vesicles with hemorrhagic crusting
- Painless black pigmented patches
How does lichen planopilaris typically present on the scalp?
- Tiny red, spiny follicular papules spreading across smooth areas
- Well-demarcated round patches of hair loss without inflammation
- Diffuse scaling with yellow crusting
- Black dots with broken hairs
- Boggy swellings with pustules
Which pattern best describes the presentation of lichen planus pigmentosa?
- Ill-defined, oval, grayish-brown marks on sun-exposed areas
- Well-demarcated red patches with silver scale
- Symmetrical brown patches on cheeks and nose
- Deep purple patches in flexural areas
- Yellow-brown macules in a butterfly distribution
Which treatment approach is most appropriate for widespread lichen planus in patients with skin of color, aiming to minimize post-inflammatory hyperpigmentation?
- Systemic corticosteroids
- Topical retinoids alone
- Sedating antihistamines
- Emollients alone
- Light therapy
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |