Playlist
Show Playlist
Hide Playlist
Pediatric Bleeding Disorders: Von Willebrand Disease (VWD)
-
Slides Bleeding Disorders.pdf
-
Download Lecture Overview
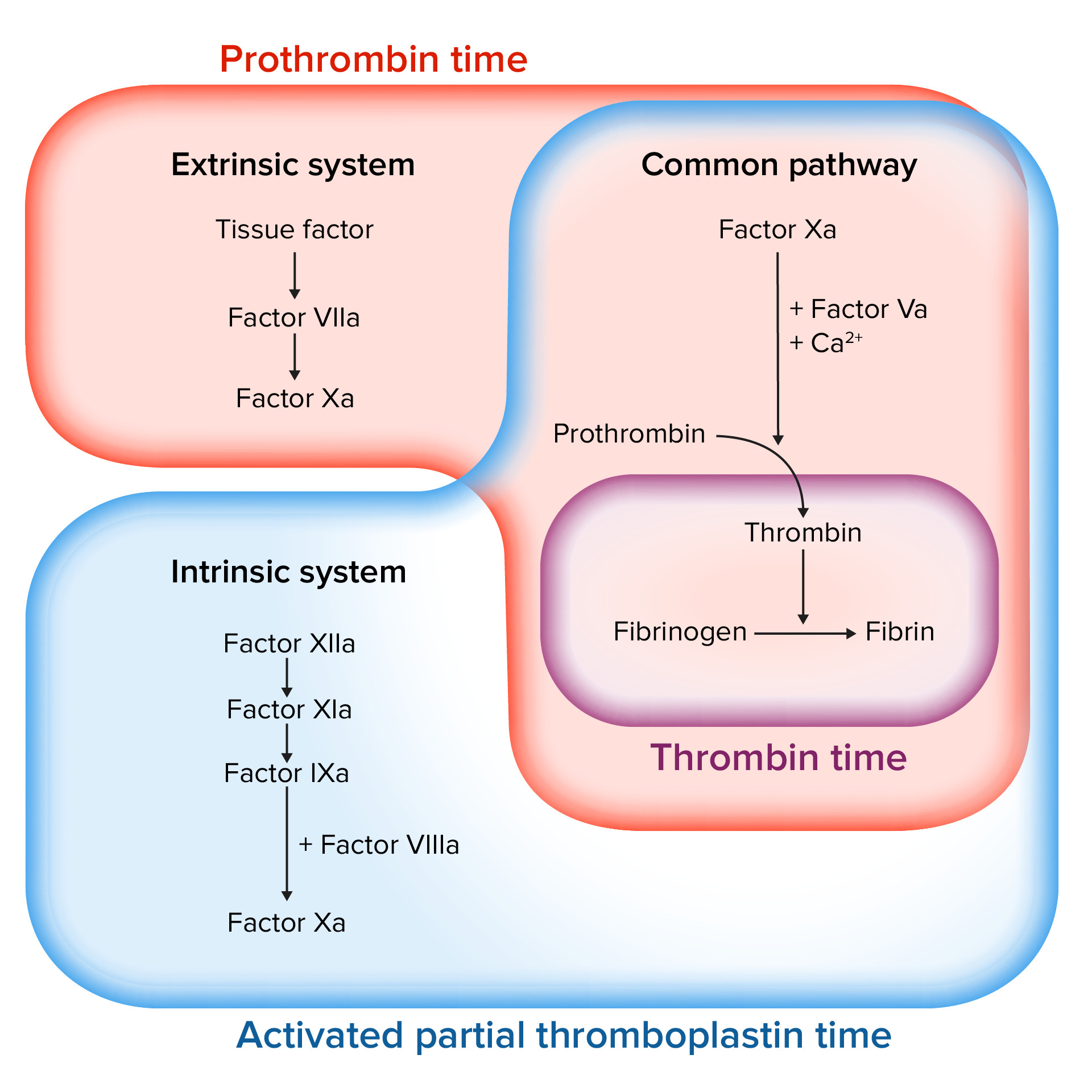
00:02 In this lecture, we’ll discuss bleeding disorders in children. 00:06 So we can think of bleeding disorders based on how we know clots form. 00:11 First, there is tissue damage and then both platelets and the coagulation cascade occurs that help form that clot. 00:19 In children, there can be problems with both the coagulation cascade and platelet activation. 00:25 We’ll discuss platelet activation first. 00:28 So here’s an inherit cartoon where you can see how platelets activate together and collide together and there are 2 major problems that can happen with platelets that can lead to platelet dysfunction. 00:41 One is problems with Von Willebrand’s factor and the other was intrinsic problems within that platelet. 00:47 Let’s start with Von Willebrand’s factor. 00:50 So Von Willebrand disease is a genetic defect in Von Willebrand factor. 00:55 It is the most common inherited bleeding disorder in children. 00:59 We have to remember that Von Willebrand’s factor does two different things. 01:03 First, it does bind the platelets, but then also it acts as a carrier protein for factor VIII. 01:10 So these patients may have problems with factor VIII as well. 01:15 So there are many different types of Von Willebrand’s disease and I’d like to go through a few of them. 01:21 Some of them are important to understand and some are so rare that we can just discuss them briefly. 01:28 So type 1 is very common. 01:31 It’s the most common type of Von Willebrand disease. 01:34 It’s autosomal dominant and it affects about three-quarters of patients. 01:39 The severity of the disease can vary a lot from mild to severe. 01:44 Type 2A is also autosomal dominant and is present in about 15% of patients. 01:50 Usually they have moderate degree of severity of illness. 01:54 The same thing can be said of type 2B, again, autosomal dominant, about 5% of patients and again moderate degree of illness. 02:03 And then there are the rare types. 02:05 There is the platelet-type which is extremely rare, but is a gain of function mutation and these patients actually have hypercoagulability rather than a bleeding disorder. 02:16 Type 2M is fairly rare and these patients have a normal level of Von Willebrand’s factor but it doesn’t work correctly. 02:25 Type 2N is autosomal recessive. 02:27 These patients have a low factor 8 level and often, these patients are mistaken for a patient with hemophilia. 02:35 And there's type 3 which is extremely rare, but these patients are very sick, they have a completely unmeasurable amount of Von Willebrand’s factor and resultingly a low factor VIII as well. 02:48 So how do these patients present? Well, they will present absolutely with easy bruising, bleeding, bleeding from the nose and mouth and excessive menorrhagia. 02:59 So the easy bruising is usually spontaneous. 03:02 These bruises are usually large and they’re often in unusual locations. 03:08 Sometimes, you might think that this child might have been a victim of child abuse, but in fact they have Von Willebrand’s disease. 03:15 They will often bleed excessively from minor lacerations with prolonged bleeding and they may get excessive scarring of those lacerations. 03:24 Nose and mouth bleeding is common and these patients usually have frequent nose bleeds. 03:31 Often times, these nose bleeds are hard to control and require afferent spray and ice and all kinds of intervention that most kids don’t require. 03:39 They also will bleed excessively with tooth loss or simply when they’re brushing their teeth. 03:46 In terms of menorrhagia, we usually pick this up in young girls who are having their first period and they will have dramatically increased bleeding with their menses. 03:55 And the menses will last longer than usual. 03:58 So if we wish to diagnose Von Willebrand’s disease in a child who is presenting with excessive bleeding, we get a PT/PTT and in most of these cases, it’s normal. 04:08 This is because their factor VIII is working enough that they have a normal coagulation cascade. 04:15 However, if we further investigate, we will find further testing which reveals a diagnosis of VWD. 04:22 The first test we will get is a VWF antigen. This is measuring directly quantity of VWF proteins in the blood. 04:32 A level below 30% indicates VWD. 04:36 A level over 50% is normal, and in the 30-50% range the disease may be suspected if there is a history of bleeding in the child. 04:46 We can also test the activity of the VWF that is in the blood, not just the quantity that is there. 04:53 For this, we will bind the VWF to various binding partners. Usually, we’ll use a GP1b receptor on platelets, or we can bind it to collagen. 05:05 The most common test for function is the “ristocetin cofactor” which assesses GP1b binding. 05:12 Ristocetin was an antibiotic that they took off the market because it caused thrombocytopenia and the reason it did that is because it bound to Von Willebrand’s factor. 05:22 Results are interpreted just like the antigen levels. A level below 30% indicates VWD. 05:29 A level over 50% is normal, and in the 30-50% range the disease may be suspected if there is a history of bleeding in the child. 05:37 The factor VIII level is obtained but will be different in different patients depending on the subtype of disease as we discussed earlier, and a normal level does not preclude VWD as a diagnosis. 05:49 We no longer use either a bleeding time, or a platelet function assay, which are older methods of testing for bleeding disorders in children. 05:57 The PFA had a high false positive rate, and the bleeding time was inaccurate and time-intensive to perform. 06:07 So how do we treat Von Willebrand’s? Well, we usually start with a DDAVP challenge. 06:13 DDAVP increases Von Willebrand factor and presence of factor VIII. 06:18 It’s not effective for all subtypes of disease, for example, type 3, it will have not much effect at all, but it is good for types 1 and 2. 06:27 DDAVP is usually used as a nasal spray. 06:31 Also, we have to watch for hyponatremia. 06:34 Remember, DDAVP causes insertion of aquaporin channels and causes reclaiming of free fluid, so these patients may develop a low sodium. 06:45 Von Willebrand’s factor viii is usually reserved for patients with very severe disease and for a severe bleeding event, we will usually give factor VIII as well as recombinant Von Willebrand’s factor. 06:58 And we may use topical thrombin to mucous membranes to help them stop the bleeding. 07:05 There are some other unusual platelet aggregation problems where the platelets have an inherit problems sticking together. 07:12 The patient will have a normal number of platelets, they just won’t be working correctly. 07:16 These patients tend to present with severe bleeding disorders. 07:20 The normal number of platelet is there. 07:21 They will have a normal Von Willebrand’s factor and a normal PTT and PT. 07:27 So, it can be a challenge to make this diagnosis and a platelet function assay is the way to do it. 07:32 When you think about this, remember Glanzmann’s thrombasthenia, this is probably the most important kind to remember for a test.
About the Lecture
The lecture Pediatric Bleeding Disorders: Von Willebrand Disease (VWD) by Brian Alverson, MD is from the course Pediatric Hematology.
Included Quiz Questions
Which of the following abnormal lab findings is most likely to be seen in patients with von Willebrand disease?
- <30% VWF antigen levels, or <50% in a patient with a bleeding history
- Prolonged PT
- Prolonged PTT
- Prolonged INR
- Thrombocytosis
Which of the following coagulation factors is bound to von Willebrand factor in its inactive form?
- Factor VIII
- Factor VII
- Factor IV
- Factor II
- Factor I
Which of the following is the most common type of vWD?
- Type 1
- Type 2A
- Type 2B
- Platelet type
- Type 3
Which of the following tests is not indicated in the diagnosis of von Willebrand disease?
- Bone marrow aspiration
- Von Willebrand factor antigen
- Ristocetin cofactor
- Factor VIII levels
- Complete blood count
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
Excellent lecture. Hematology is a topic that is often a poorly explained topic. Thanks for bringing so much clarity to it!