Playlist
Show Playlist
Hide Playlist
Vagus Nerve – Thoracic Nerves
-
Slides 05 Thoracic Viscera Canby.pdf
-
Download Lecture Overview
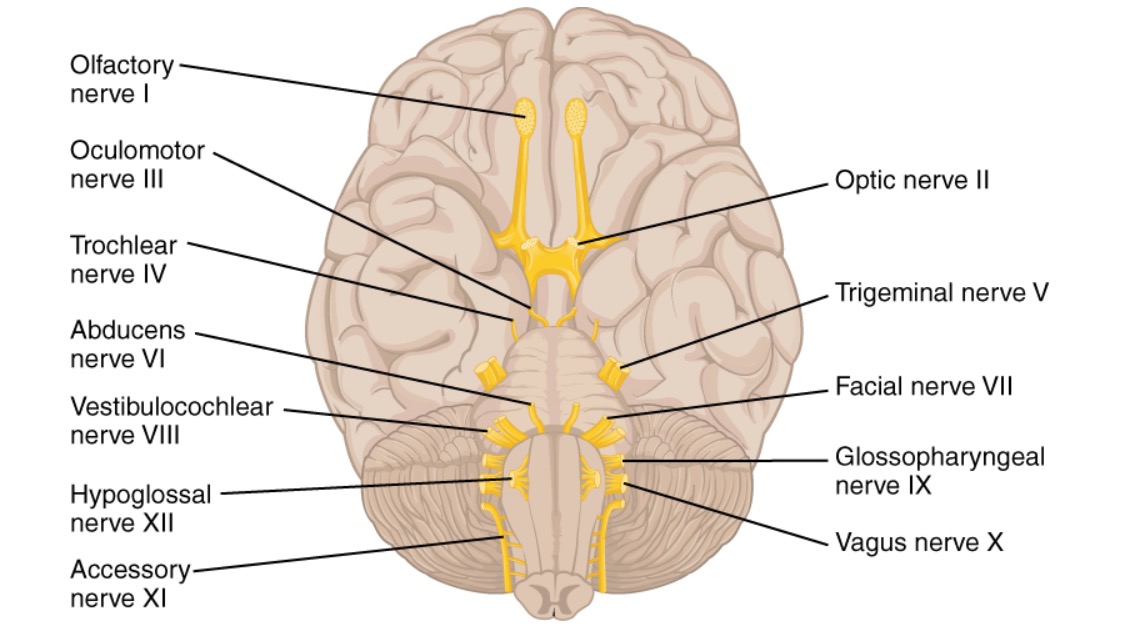
00:01 The vagus nerve is a cranial nerve. It is the longest of the cranial nerves. 00:08 It has the most extensive distribution. Vagus is derived from a word meaning “wandering” and so, it does wander throughout the entire body almost. It conveys various fiber types. 00:23 These are somatic, afferent or sensory fibers. Going to the body wall, we also will see visceral afferents. So, these are sensory fibers that are conveying senses from the organs. Somatic afferents and so these are motor fibers to somatic muscles. 00:42 We also have two types of visceral afferent fibers being conveyed to the vagus nerve. 00:48 These will be general visceral afferents as well as special visceral afferents. And if we take a look at the course of the left vagus nerve, we see the left vagus nerve descending from the neck into the thoracic cavity and it is crossing anterior to the arch of the aorta. And the visceral afferents that are conveyed in the vagus nerve, these afferents are parasympathetic fibers. 01:29 Here, we are looking at the same image, but I want to call your attention to the right side of this illustration. Here we have the right vagus descending from the neck. It was cut and removed to show more clearly some additional structures in this region, but here’s your right subclavian artery. The right vagus nerve will course anterior to your right subclavian and then, we see the distal cut end of the vagus and then, we will see it continuing in the thoracic cavity along the right lateral margin of the esophagus and left one will also start to occupy here initially a similar course on the left margin of the esophagus. 02:20 Now, let’s take a brief moment to explore the various fiber types and their distribution. 02:29 This slide shows us the general visceral efferents and the general visceral afferents. The general visceral efferent fibers are innervating the smooth muscle that’s associated with respiratory tree. We also have the mucous glands that are associated with the respiratory tree. 02:50 Hence, they are innervated by these visceral general efferents. The heart also receives distribution through this fiber type and these same fibers are conveyed and distributed to the esophagus. Sensory fibers from the viscera, the thorax, constitute the general visceral afferents of the vagus nerve. 03:20 Here, we are looking at the distribution of the vagus nerve to the heart. These general visceral efferents are parasympathetic fibers and they are shown in purple in this illustration. 03:34 So, we have our right vagus here purple, we have our left vagus and then, you can see branches are coming off the vagus nerves and are distributed to the atria and then, very sparse distribution to the ventricles and the primary distribution to the ventricles would be the coronary vessels that supply the ventricles. 04:02 Functionally, the parasympathetic fibers being conveyed in the vagus will decrease the heart rate. 04:10 They have minimal influence on myocardial contractility or force of contraction because of that sparse distribution to the ventricles, but they do directly vasodilate the coronary vessels and then, those coronary vessels will subsequently start to, then, constrict because of the decrease in heart rate. 04:40 This particular slide is demonstrating the parasympathetic fibers that are being distributed to the esophagus. These are the general visceral efferents again. We see both vagus right and then, left here and we see various branches that contribute to the innervation of the esophagus, more distally. 05:06 What will happen is the left vagus will come more anterior whereas the right will turn more posterior in relationship to the esophagus and the left vagus will become what is known as the anterior vagal trunk. The right vagus being rotated posteriorly will become the posterior vagal trunk and this is due to developmental events of the primitive GI tube being rotated to the right side of the body. There is a pneumonic to help you remember which vagus is the anterior trunk versus the posterior trunk. That pneumonic is LARP and this simply means that the left becomes anterior, the right vagus will become a posterior. 06:01 The visceral efferents, that are generally supplying the esophagus, are involved in peristalsis of the esophagus and the parasympathetics will also allow for a bolus of food to move from the esophagus into the cardiac region of the stomach, thereby relaxing the lower esophageal sphincter. If there is damage to the parasympathetic components anywhere along this pathway within the wall of the esophagus via parasympathetic components, mediastinal mass compressing the vagus or even a stroke where the motor nuclei are located, any one of those kinds of events can cause failure of the sphincter mechanism and as a result, you have a disease or disorder called achalasia. 06:52 Within the thoracic cavity, the vagus nerve will give rise to recurrent laryngeal nerves. 06:59 Both of these recurrent laryngeal nerves are detected in this illustration. So, let’s take a brief moment for you to take a look at them. Here is your left vagus nerve coursing anterior to the aortic arch. And right at this particular point, we see the left recurrent laryngeal nerve branching off the left vagus. It will then wrap underneath the aortic arch and then, will ascend posterior to it into the neck and here, we can pick it up again and it will disappear under cover of the thyroid gland that we see here more superiorly. 07:37 On the right side, the right recurrent laryngeal nerve has a slightly different course to ascend into the neck and what it will do is, it will issue from the right vagus, we see the right vagus here, right vagus, as mentioned before, will cross anterior to the subclavian. The subclavian has been cut right along here distally and it’s more proximal attachment will be back in this general direction, but right here, we can see coming up this distal segment of the vagus, we can see the right recurrent laryngeal nerve. It would then ascend along the trachea and then, pass deep or posterior to the right subclavian vein and then would continue its ascend upwards into the neck under cover of the thyroid. 08:30 The recurrent laryngeal nerves convey special visceral efferents and these visceral special efferents are going to innervate all the intrinsic muscles of the larynx except for the cricothyroid. 08:45 The special visceral efferents will also innervate muscles of the pharynx with the exception of the thyropharyngeus muscle and the palate with the exception of the tensor veli palatini. 09:00 If you have a mediastinal mass such as the mediastinal tumor, that tumor could, in some cases, encroach upon one of your recurrent laryngeal nerves and let’s just say, the mass is over here on the left side encroaching upon the left recurrent laryngeal and if there is too great of a involvement of that mass on that recurrent laryngeal nerve, that can lead to hoarseness and even vocal cord paralysis.
About the Lecture
The lecture Vagus Nerve – Thoracic Nerves by Craig Canby, PhD is from the course Thoracic Viscera with Dr. Canby.
Included Quiz Questions
The right vagus nerve crosses anterior to what structure?
- Right subclavian artery
- Left subclavian artery
- Aortic arch
- Trachea
- Esophagus
A patient with a mediastinal tumor has hoarseness. What nerve is involved?
- Recurrent laryngeal nerve
- Phrenic nerve
- Posterior vagal trunk
- Anterior vagal trunk
- Sympathetic trunk
Which type of fibers are present in the vagus nerve? Select all that apply.
- Somatic afferent
- Olfaction afferent
- Visceral afferent
- Somatic efferent
- General visceral efferent
Which soft palate muscles are innervated by the vagus nerve? Select all that apply.
- Levator veli palatini
- Tensor veli palatini
- Palatoglossus
- Palatopharyngeus
- Musculus uvulae
What is innervated by the general visceral afferent fibers present in the vagus nerve?
- Viscera of the thorax
- Pericardium
- Elastic muscles of the respiratory tree
- Smooth muscles of the respiratory tree
- Mucous gland of the respiratory tree
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
Not boring at all. I don't like the topics about nerves, but I listen your lectures with great pleasure