Playlist
Show Playlist
Hide Playlist
Thyroid Gland – Neck
-
Slides 26 Neck2 HeadNeckAnatomy.pdf
-
Download Lecture Overview
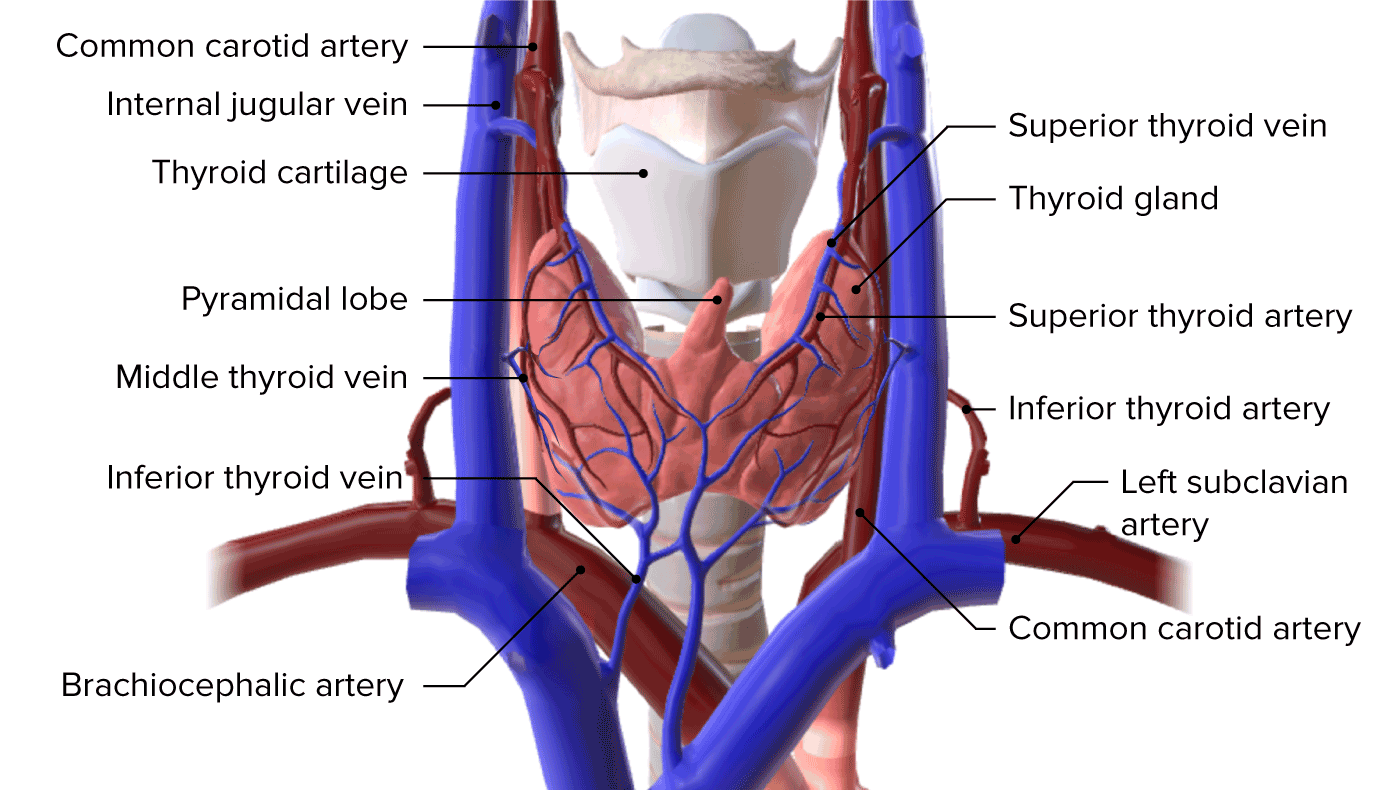
00:01 Welcome to this presentation on the neck part two. 00:09 During this presentation, we're going to cover three subject areas, we're going to begin by looking at the thyroid gland. 00:16 Secondly, we'll visit the stellate ganglion and then lastly, we'll visit the thoracic outlet. 00:23 And as we move through each of these three topical areas, we'll discuss clinical correlations. 00:31 So here we begin with the thyroid and what I want you to understand here at the beginning is some really basic anatomy. 00:40 The thyroid gland is located anteriorly to the trachea, in the lower neck, at the level of the fifth cervical to the first thoracic vertebrae. 00:48 It has a brownish-red color and a nodular appearance. 00:52 First, the thyroid is made up of lobes. 00:56 Here we see the right lobe. 01:01 Next, we have the left lobe. 01:04 And lastly, both lobes are connected by an isthmus. 01:11 The apices of the lobes diverge laterally on the laminae of the thyroid cartilage, and their bases are at the level of the fourth or fifth tracheal cartilages. 01:20 The lobes are attached on their posterormedial aspects to the cricoid cartilage by Berry's ligament. On their lateral aspect, the lobes are in close relationship with the great vessels of the neck. 01:31 This particular slide shows a very important clinical relationship or anatomic relationship, and this is the relationship of the thyroid gland to the recurrent laryngeal nerves. 01:47 Each laryngeal nerve here is the right recurrent laryngeal nerve. 01:54 It's lying within the trachea, esophageal groove, and we see that grew between the trachea and the esophagus, which lies posteriorly. 02:06 We also see the same relationship, however, it's unlabeled on the opposite side, so here is your left recurrent laryngeal nerve and again, it travels in the tracheoesophageal groove on that particular slide. 02:25 Clinically, these are important during a thyroidectomy. 02:30 The surgeon has to carefully identify these nerves and preserve them so they are not injured during the removal of the thyroid gland will also demonstrate another clinical correlation of the recurrence. 02:43 When we talk about thyroid goiter. 02:50 The thyroid gland is supplied by the superior and inferior thyroid arteries, and in some instances by the thyroid artery of Neubauer, a branch from the brachiocephalic trunk or aortic arch. 03:05 Here are some important aspects about the recurrent laryngeal nerves, both recurrent laryngeal nerves are branches of the vagus nerve, and they will supply all the intrinsic laryngeal muscles with the exception of the cricothyroid. 03:26 They are called recurrent as they come off the vagus nerve and then travel back upwards to either side of the trachea and ultimately to their destination of the larynx. The left and right recurrent laryngeal nerves do have some anatomic relationship differences, the left recurrent laryngeal nerve loops around the aortic arch in the vicinity of the ligamentum arteriosum, whereas the right recurrent laryngeal nerve loops more superiorly on the right side and loops under the right subclavian artery. 04:12 Here is an important clinical correlation here, we're looking at goiter in this particular individual has a very enlarged thyroid gland, very large mass that's very visible. 04:30 In this particular individual, there are multiple enlarged nodules, so this particular form of goiter is multi nodular. 04:45 Some of the symptoms that are associated with a goiter are as follows. 04:53 One is coughing. 04:57 And this has a mass effect on the respiratory passageways and the larynx, a second symptom is hoarseness. Very large goiters can involve the recurrent laryngeal nerves, and if they become involved, then they're unable to effectively activate the muscles of the larynx and can then create the hoarseness. Another symptom that can be associated with goiter is the difficulty swallowing dysphagia, and this would be due to a mass effect. 05:36 So the mass is compressing the structures that convey the bolus of food. 05:42 And then lastly, again, due to a mass effect, you can have compression of your respiratory passageways in the area, the trachea, and making that a problem for some patients. 05:57 A very common procedure to demonstrate whether or not nodules are functional nodules or nonfunctional nodules is to utilize a technician. 06:09 Ninety nine M protectant eight Skåne. 06:13 And we see here in the image the results of such a scan. 06:21 Hot nodules are going to show up. 06:24 In this kind of cooperation that we see here, this is due to the presence of functional thyroid nodules and they're taking up the technician. 06:36 Ninety nine. So this these areas light up when you have a hot nodule out region. 06:42 A cold cold nodule is not a functional nodule. 06:48 So these types of nodules will not pick up the technician. And this area here represents a cold nodule in this scan. 07:04 So here we are demonstrating more specifically some of the aspects of a cold nodule. 07:12 And again, it's this area here. 07:14 nonfunctional. These are usually benign. 07:23 And then lastly, the odds of being malignant are going to be greater than the hot nodules. 07:36 Here we're looking at the thyroid gland with respect to a clinical procedure, its removal, a thyroidectomy, some of the indications for a thyroidectomy are what we just went through. 07:50 For example, a goiter cancer of the thyroid gland would also be another indication for its removal. 07:59 And then lastly, persistent hyper thyroid ism. 08:05 Some complications associated with a thyroidectomy. 08:11 Include. Bleeding. 08:17 From the vasculature, either arterial bleeding or venous bleeding. 08:23 Infection is always a concern in any surgical procedure. 08:31 As we discussed not too long ago, hoarseness of the voice can occur if there is surgical injury to one of the recurrent laryngeal nerve. 08:45 So, again, it's very important to isolate them and protect them during a thyroidectomy. The last complication to highlight. 08:57 For your information, is that some patients can have hypoparathyroidism, this is due to not being able to adequately identify the parathyroid glands before the removal of the thyroid, and as a result, the thorough are also removed. And then you do not have enough functional parathyroid tissue remaining for them to carry out their function.
About the Lecture
The lecture Thyroid Gland – Neck by Craig Canby, PhD is from the course Head and Neck Anatomy with Dr. Canby. It contains the following chapters:
- Thyroid Gland
- Thyroid Gland – Goiter
- Thyroid Gland – Technetium 99m Pertechnetate Scan
Included Quiz Questions
Which of the following groups of muscles is supplied by the recurrent laryngeal nerve?
- Intrinsic laryngeal muscles
- Extrinsic laryngeal muscles
- Smooth esophageal muscles
- Extrinsic pharyngeal muscles
- Intrinsic pharyngeal muscles
What is the anatomical location of the thyroid isthmus?
- Anterior to the trachea
- Anterior to the esophagus
- Anterior to the vertebra
- Posterior to the esophagus
- Posterior to the trachea
During a thyroidectomy, which of the following structures has to be assessed for its presence in the tracheoesophageal groove?
- Recurrent laryngeal nerve
- Vagus nerve
- Inferior thyroid vein
- Internal jugular vein
- Common carotid artery
Which of the following is NOT a characteristic of cold nodules in the thyroid gland?
- Increased T3 and T4 production
- Usually benign status
- T99 scan showing less than normal activity of the thyroid gland
- Odds of malignancy being greater than for hot nodules
- Nonfunctional status
Which of the following complications results from unilateral damage to the recurrent laryngeal nerve during thyroidectomy ?
- Hoarse voice
- Hyperparathyroidism
- Laryngeal obstruction
- Bilateral vocal cord paralysis
- Cough
Customer reviews
4,1 of 5 stars
| 5 Stars |
|
8 |
| 4 Stars |
|
2 |
| 3 Stars |
|
0 |
| 2 Stars |
|
2 |
| 1 Star |
|
1 |
I like this Guy I am the Last Hope Yes Yeah Si SIp
i like the videos very much because of the clear presentations
Excellent thank you. Thank you Dr. Craig, this video is very helpful.
good job loved it easy abdsorbing and can understand english very well