Playlist
Show Playlist
Hide Playlist
Tachycardia: Wolff-parkinson White Syndrome: Diagnosis and Treatment
-
Slides Tachyarrhythmia MultifocalAtrialTachycardia CardiovascularPathology.pdf
-
Download Lecture Overview
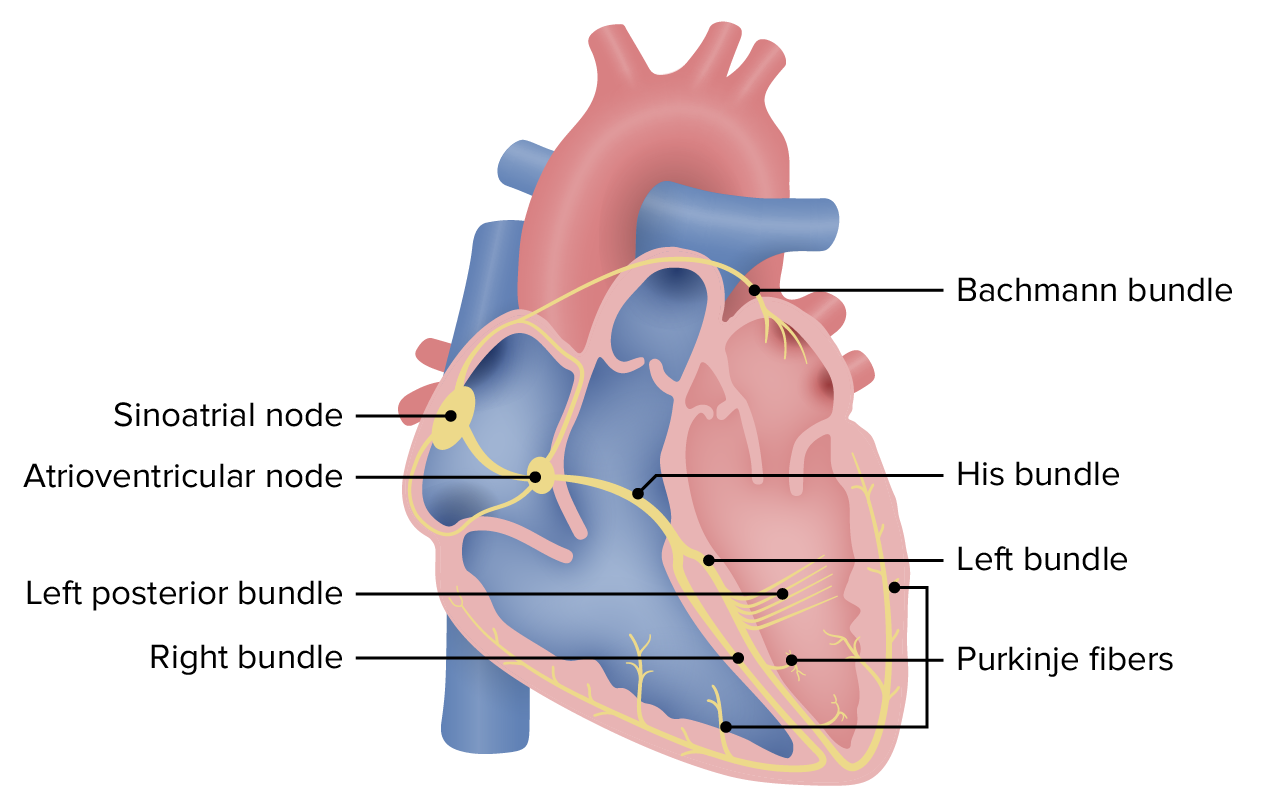
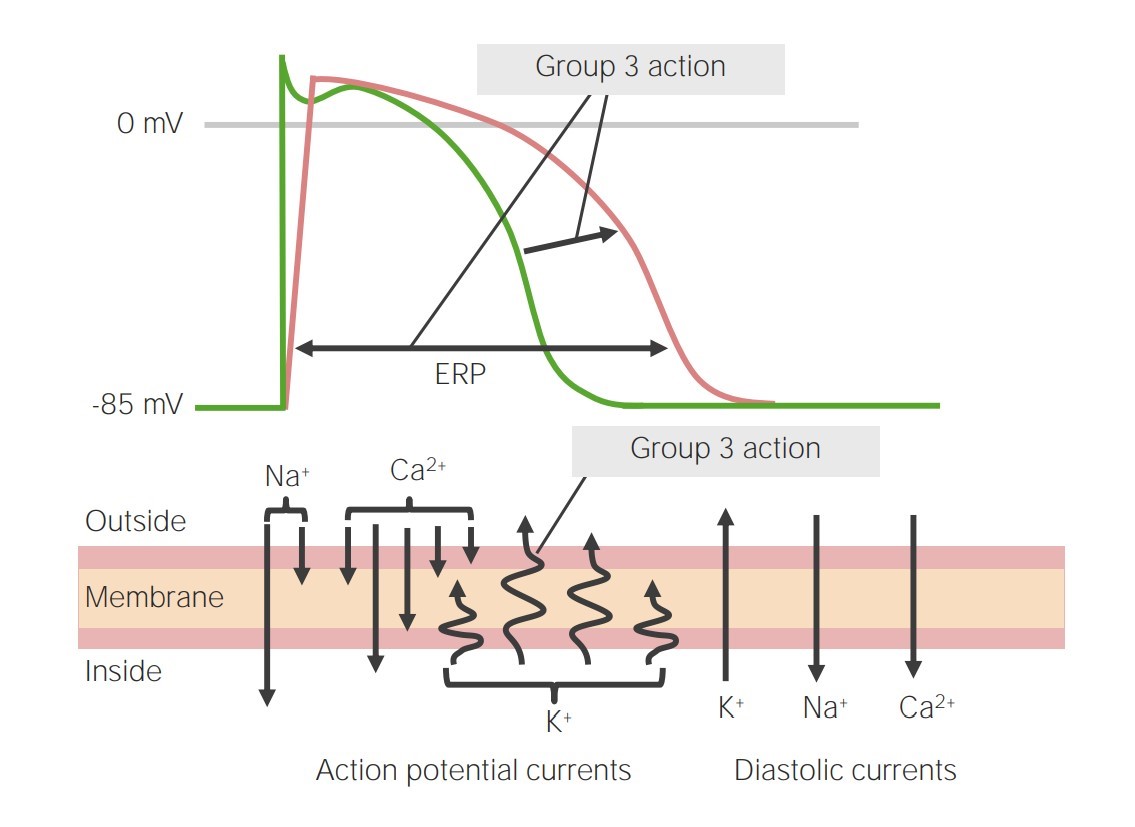
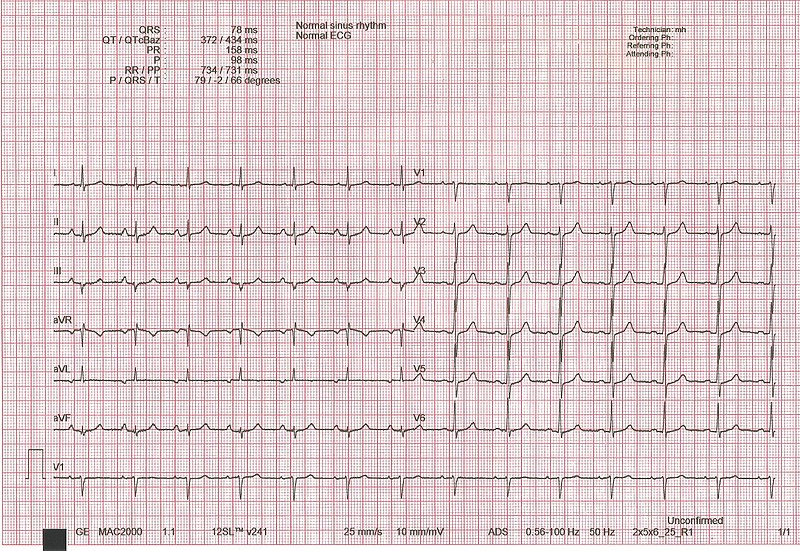
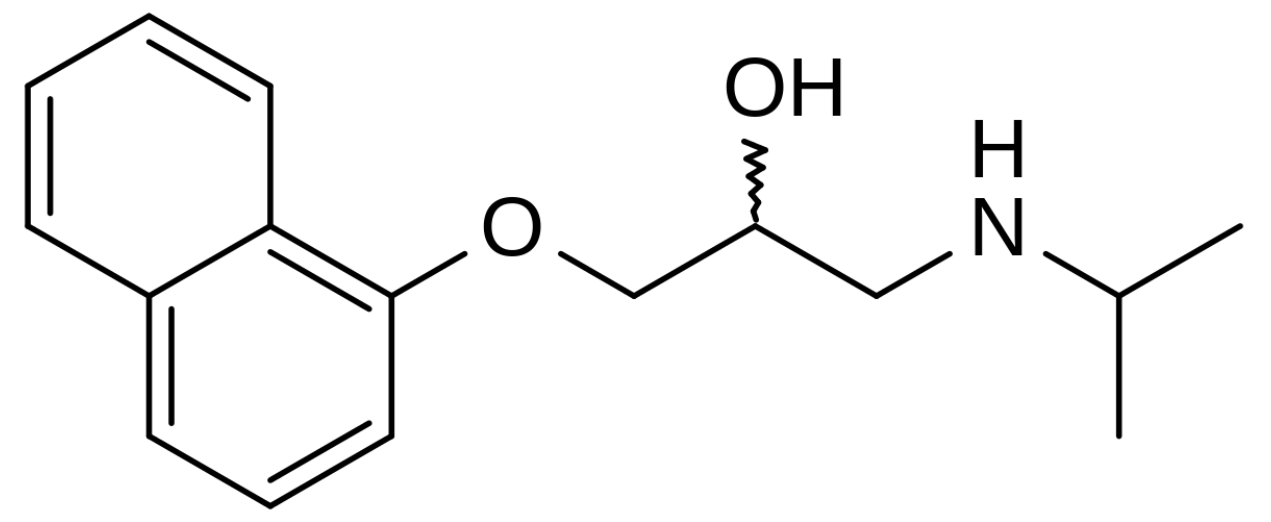
00:01 What are we looking for further? Let's take a look at what we have done already. What did we discuss with PR interval? Shortened. What does that mean? Less than 0.12 seconds. What other components do we have of WPW? Well, the next two are going to be combined. On that QRS complex, you are going to have something called a delta wave or a slurred wave. And once you form that delta wave on the QRS complex, understands the QRS complex actually widens. So the only thing that you are going to find widened or prolonged in Wolf-Parkinson-White will be the QRS complex. The PR interval will be shortened and you will have a delta wave. You put those to be together, the pre-excitation syndrome, you cannot miss this. But it begins with understanding the foundation. It is with knowing that you have accessory pathway pathology. If you take a look at this ECG, I want you to take a look at the very bottom in which you end up finding is exactly what I just said, with your delta wave, widening of the QRS complex in a shortened PR interval. 01:19 Let us take a look at management of Wolf-Parkinson-White. Now it is just as important that you pay attention to how you wish to control your rate and such with arrhythmias. It is just as important sometimes if not more to look after those drugs that are contraindicated. Why, is the big question? For example, up until now we are pretty much seeing verapamil, your calcium-channel blocker being used in every single type of SVTs. They included afib, atrial flutter and we had multifocal atrial tachycardia. Digoxin, the first time that we are seeing that really not being used or not preferred was with multifocal atrial tachycardia. These drugs were used as being antiarrhythmics because it slows things down in the heart. But why is it that in Wolf-Parkinson, why all of a sudden even though you want to control and manage and you want to cardiovert, end up being contraindicated? Because how many pathways do you have in WPW? Two. One is the physiologic normal AV node and the other one is the pathologic and no delay characteristics. So, therefore, if you were to block any impulse from passing through the AV node, what have you done ladies and gentleman? You have now forced that impulse to go through to the pathologic pathway and exacerbate the condition. No other so far SVT has an accessory pathway like what we are seeing here with WPW. You want to avoid calcium-channel blocker, digoxin and to a certain extent, adenosine as well. These are the drugs in which if you block that AV node, you are forced to go into your accessory pathway and you don't want that. That must be understood. So if that is the case in terms of the medical cardioversion and some of these drugs are contraindicated, then what choice are you now left with? Well, you are left with a couple. You have electrical cardioversion if the patient is hemodynamically unstable or procainamide infusion if stable. Keep that in mind. Why would you think about even using procainamide in a patient that has an arrhythmia? Well, procainamide is a class I drug. Stop there. Class I antiarrhythmic is a sodium channel blocker and you have three subtypes of class I. Ia, Ib, and Ic. Ic is relatively simple. Flecainide is what you are thinking perhaps and it does not distinguish between which gate of the voltage-gated sodium channel? What does that mean? A flecainide can either or class IC can block the activated channel or it can block the inactivated channel. When you block both of these gates of the channel, then your sodium channel for what intended purpose is completely rendered dysfunctional. 04:10 If you do not have a voltage-gated sodium channel, how in the world are you going to have what phase? Zero. Phase 0 of which action potential? The one with the plateau. 0, 1, 2, 3, 4. 04:26 That is the mechanical one. So if you can’t have phase 0, how in the world is heart supposed to pump? It doesn't. Are you worried about sudden cardiac death with 1c? Yes, you are. 04:36 Let us talk about procainamide. Procainamide is Ia. Ia used the atria advantage because that A then represents to you the activation gate of the sodium channel. Normally speaking at RMP. Let us say at approximately negative 90 resting membrane potential, what did your sodium channel look like? Close your eyes. Think about what it looks like. The activation gate is closed and the inactivation gate is opened, is it not? Where is my inactivation gate? How important is that? Really important. It is facing the inner side of the cell membrane. 05:10 Well, that activation gate gets opened when it is triggered and sodium rushes in. That is where procainamide works. Procainamide is a 1a class in which it blocks the activated channel, A and A. Use this as a cardioverter if your patient is hemodynamically stable. 05:30 If not, electrical cardioversion. WPW is what we are talking about. What are three major components? You begin with PR interval, shortened or prolonged, please? Shortened. What does that mean? Less than 0.12 seconds. Move on. QRS complex, give me the two components there. 05:47 One with the delta wave which is a slurred and the widened QRS complex. 1, 2, 3 for WPW. 05:52 Do you ever use digoxin? No. Because then you are forcing it to the accessory pathway. 05:59 Now, definitive treatment is ablation of the accessory pathway. Is that clear? These are important steps for management. What drugs to avoid at all cost? What kind of cardioversion, depending as to the status of your patient and then definitive therapy. Get rid of the accessory pathway, ablated. 06:22 Now, with our other supraventricular tachycardia, I am just going to mention a few things here. 06:28 Now we ask them to go AV nodal reentry tachycardia and we have atrial tachycardia. I am not going to go into great detail about AV nodal reentry tachycardia at this juncture, but atrial tachycardia, ASV and SVT, would then mean that the P waves are increasing in number. Increased heart rate. And all that the picture is showing you is another type of reentry of AV nodal. At this point, I will consider this to be a little bit too much detail, but nonetheless, I have placed it here so that you understand ladies and gentleman, that not only could you have something like Wolf-Parkinson-White syndrome has an accessory pathway, but then as you further along into education, you will learn more about these reentry tachycardias. One are be prepared versus being shocked. On your own time, you may take a look at this. Let us continue.
About the Lecture
The lecture Tachycardia: Wolff-parkinson White Syndrome: Diagnosis and Treatment by Carlo Raj, MD is from the course Arrhythmias: Basic Principles with Carlo Raj.
Included Quiz Questions
What drug is used in the medical cardioversion of tachycardia in a patient with Wolff-Parkinson-White syndrome?
- Procainamide
- Flecainide
- Propranolol
- Verapamil
- Digoxin
Which of the following is seen in the ECG of a patient with Wolff-Parkinson-White syndrome?
- Delta wave, widening of the QRS complex, and shortening of the PR interval.
- Delta wave, narrowing of the QRS complex, and shortening of the PR interval
- Delta wave, widening of the QRS complex, and a prolonged PR interval
- Delta wave, widening of the QRS complex, and a normal PR interval
- Delta wave, widening of the QRS complex, and shortening of the QT interval
What is the mechanism of action of procainamide?
- It blocks the activated voltage-gated sodium channel.
- It blocks both the activated and inactivated voltage-gated sodium channels.
- It blocks the activated ligand-gated sodium channel.
- It blocks the calcium channel.
- It blocks both the activated and inactivated ligand-gated sodium channels.
What is the definitive treatment of Wolff-Parkinson-White syndrome?
- Surgical ablation of the accessory pathway
- Procainamide
- Chronic antiarrhythmic therapy
- Placement of a permanent pacemaker
- No definitive treatment is available.
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
I love how he explains why CCBs and digoxin are contraindicated in WPW and also review of how digoxin isn't useful for MAT