Playlist
Show Playlist
Hide Playlist
Short Bowel Syndrome and Bile Acid Malabsorption
-
Slides GIP Short Bowel Syndrome and Bile Acid Malabsorption.pdf
-
Reference List Pathology.pdf
-
Download Lecture Overview
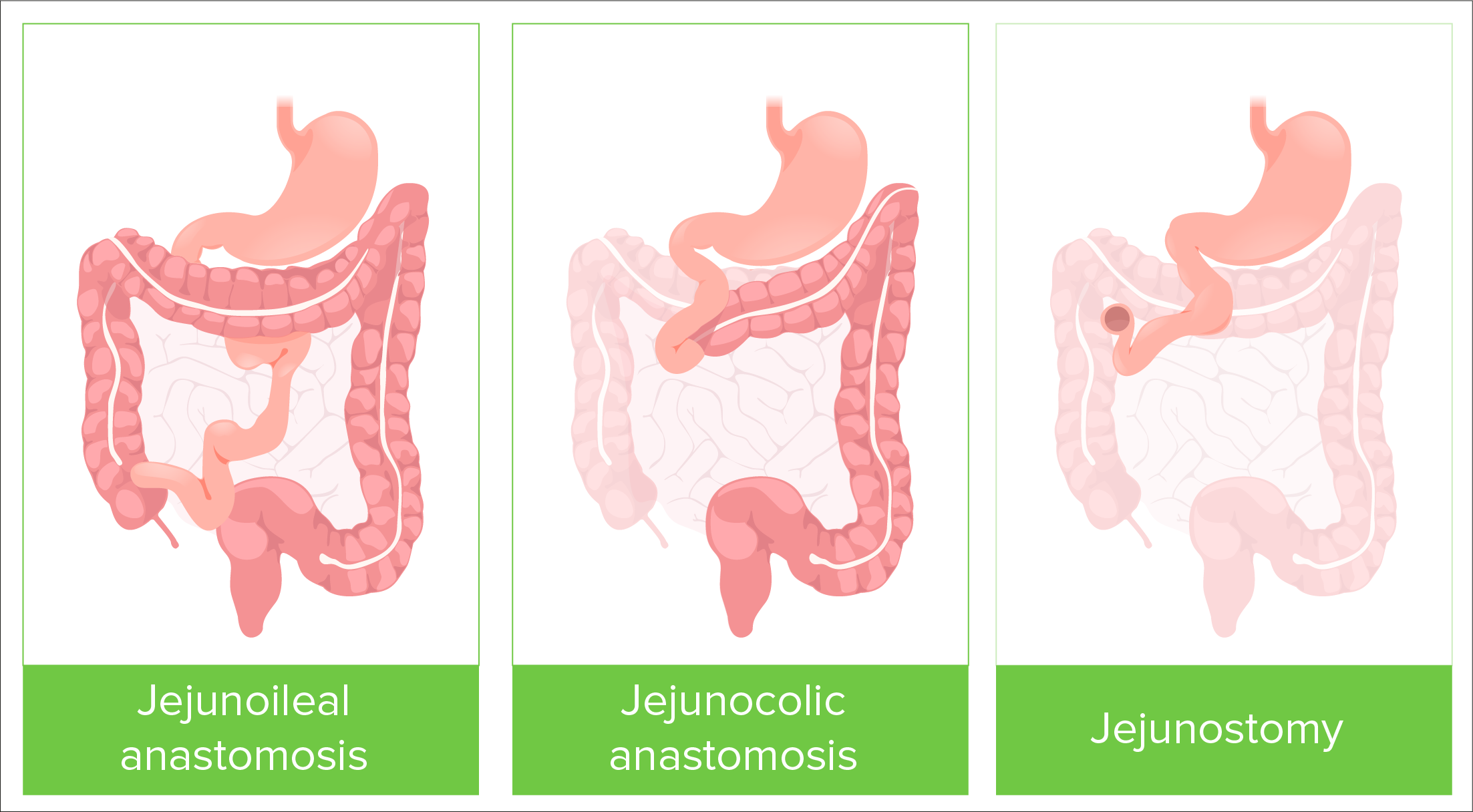
00:01 Welcome. 00:02 With this presentation, we're going to do a rather longish discussion of short bowel syndrome. 00:08 And just like the name says, this is a syndrome associated with an insufficient length of the functional small intestine, which is where the majority of nutritional absorption is going on. 00:19 So this is all about malabsorption. 00:22 The epidemiology of this. 00:25 Overall, this is something that you may never encounter in your entire medical career. 00:30 On the other hand, if you're a gastroenterologist, or a pediatric doctor, you may see it more commonly. 00:37 Overall, it's rare. 00:38 The incidence and prevalence are difficult to estimate because there may be varying degrees of small bowel atresia that are totally unrecognized. 00:48 It's estimated that between 10,000 and 20,000 individuals in the United States are on total parenteral nutrition otherwise known as TPN due to short bowel syndrome. 00:59 TPN is basically the intravenous administration of nutrition. 01:05 The pathophysiology. 01:07 In most cases, this is going to be due to a surgical resection of the small bowel. 01:14 In adults, this can happen because of mesenteric ischemia. 01:18 Atherosclerotic disease, for example, trauma, and/or bowel obstruction volvulus where we have to remove small or large segments of the small intestine. 01:29 In the pediatric population, necrotizing enterocolitis, primary intestinal atresia, or midgut volvulus with associated ischemia may be reasons why we have to resect parts of the small bowel. 01:44 There can also be functional disorders where significant lengths of the small bowel are just not able to absorb. 01:50 So Crohn's disease and/or radiation enterritis where we have really pretty much compromised vascular flow to large segments of the small bowel. 02:01 Celiac disease could potentially do this. 02:03 But usually, we recognize celiac disease and treat it appropriately before it gets to the point where the patient has a functional small bowel syndrome. 02:14 And then very rarely, congenital short bowel where there's just a relatively small segment of the small bowel present. 02:22 Keep in mind that the normal small bowel is about 7 meters, it's over 21-22 feet. 02:29 And there are some patients rarely who have segments that are only 1-2 feet less than 1 meter. 02:37 Shown here is a basic schematic of what the bowel looks like. 02:41 And in darker pink is our small bowel. 02:45 Remember, again, that it's about 7 meters over 21-22 feet, and then it goes into the cecum and around to the large intestines. 02:54 Shown on this slide are various ways to visualize what a short bowel syndrome could look like. 02:59 These are various surgical interventions that have been performed for the causes that we talked about previously. 03:06 On the very left hand side is a jejunocecal anastomosis, where we have eliminated rather large portions of the small bowel. 03:17 Another one could be a again jejunal into the transverse colon anastomosis. 03:24 And in the third one on the right hand side is a primary jejunal or ileal anastomosis that completely takes out of the circuit the rest of the small bowel and the colon that anastomosis is cutaneous. 03:39 You have a stoma with the the GI contents being drained into an external bag. 03:46 The clinical presentation. 03:49 So diarrhea is obviously very common. 03:51 Again, when we're talking about short bowel syndrome, we're talking about mal absorption. 03:56 You are not able to have sufficient length of the primary absorptive epithelium in the small bowel to take up all the nutrients. 04:05 When that happens, you have a lot of undigested food that is prime territory for bacteria to ferment and to have a field day with and there's also an osmotic pull all of that unabsorbed material sucks water out of the rest of the body to into the lumen of the GI tract. 04:27 So diarrhea, steatorrhea, again, if we're not absorbing fat appropriately because we don't have the epithelium to do so, we're going to have fatty, greasy, foul smelling stools. 04:42 Clearly, without normal absorption of nutrition, there will be weight loss. 04:46 There may be heartburn. 04:48 So depending on the transit time and depending on what's going on with the rest of the loops of the bowel, you have may have relatively low gastric emptying and so you may have symptoms of reflux disease or heartburn. 05:03 Edema occurs because of malnutrition, you're not making enough albumin in the liver. 05:09 And as a result, you've lost the normal oncotic pressure, that would tend to keep water within the vasculature. 05:16 So you will get peripheral edema. 05:18 There will be dehydration, what's been shown here is kind of pinching up folds of skin. 05:24 And normally, as you can see on me, when I release it, it goes down. 05:28 I'm well hydrated. 05:29 If a patient is poorly hydrated, that stays up, it's tenting of the skin. 05:36 There will be temporal wasting. 05:37 Again, this is due to loss of muscle mass, it's a primary malnutrition entity. 05:44 And in making the diagnosis, it's not hard. 05:47 Usually, we have a history of surgical resection of large segments of the small bowel. 05:53 But we want to also do some ancillary testing to see the downstream effects of any malabsorption. 06:01 So we'll do a complete blood test to CBC to look for anemia. 06:06 And this is going to be a big problem because we will have poor uptake of certain vitamins and components such as iron. 06:14 So we'll look to see whether we have a microcytic anemia indicating that we have poor iron absorption. 06:20 We'll see whether we have a macrocytic anemia, suggesting either a B12, or a folate deficiency. 06:25 There will be other nutritional deficiencies. 06:27 We'll be missing certain amino acids, we're missing certain fats. 06:31 So we'll be looking for those. 06:33 And then we'll do imaging. 06:34 And if necessary, in the case of our primary short bowel syndrome, we may end up doing endoscopy. 06:41 In the next two slides, I'm going to show you a patient who had had a permanent ileal colostomy. 06:47 So he had an anastomosis between portion of the ileum to the distal or to the proximal colon. 06:54 In this case, we've cut out a vast amount probably about 15 feet, about 5 meters of small bowel. 07:04 When we do the barium study, we can see flow. 07:08 So the upper left hand corner of that 5-panel figure is showing the stomach draining with a large amount of barium within it. 07:18 And then below it, we're seeing portions of the colon that have been opacified with a barium. 07:26 Basically, in the very bottom panel we're seeing, we're not seeing all of the voluminous loops of small bowel. 07:33 But in fact, we're seeing a relatively short segment of small bowel that is dumping directly into the ascending colon. 07:41 How do we manage this? So in the acute phase, usually in the immediate post surgical setting, we're going to give IV fluids and electrolyte replacement that's relatively easy to do. 07:55 But it's certainly not a long term solution. 07:57 We want to minimize irritation of this of the bowel segments. 08:03 And what can give gastric acid suppression, such as histamine antagonists, or proton pump inhibitors. 08:10 Clearly, we need to make sure that the patient especially in the early post operative period when they need to have a lot of healing, that they've got adequate nutrition. 08:18 So we give them the total parenteral nutrition. 08:21 And very slowly we add back enteral. 08:24 So oral nutrition, and we may supplement that so they get higher amounts of the necessary nutrients. 08:33 And even though they may not absorb all of them, we'll give them the best shot of having a normal enteric form of making sure that they're getting nutrition. 08:44 With time, we will slowly transition such patients to a completely oral diet, if possible. 08:50 For the first six months will suppress gastric acid, we will give anti motility agents. 08:55 Why is that? Well, in fact, we want to give that segment of small bowel that we do have as much time as possible to absorb what's there. 09:04 So if we slow the transit time with things like loperamide, we have greater opportunity to suck up all the nutrients by the small bowel. 09:13 We want to decrease GI secretions. 09:15 So using octreotide and we're doing that so that we don't kind of drive bowel transit time. 09:22 So the more gastric secretions, the more GI secretions that we have, the greater the propensity of the bowel to move that along quickly. 09:30 And Teduglutide is an analogue of the GLP, Glucagon-like peptide 2 and that is a relatively new therapy that allows improved epithelial cell growth, decreases epithelial cell apoptosis, and it also slows transit time. 09:52 And so this is something that increasingly is being used for these patients. 09:56 Finally, with relatively short segments about, you want to optimize the amount of surface area to get the most absorption. 10:05 This is a surgical technique that's been in place for probably a decade. 10:10 And what's called is serial transverse enteroplasty or STEP. 10:16 And it's a bit like origami folding. 10:18 So when you take what's small bowel that you have, and you kind of step wise put in sutures, you can actually elongate that and over time, the epithelium will fill in that and we have taken a segment of bowel that may be 30 cm, and we've made it a meter. 10:41 So that's actually pretty cool and is increasingly something that we do particularly with kids. 10:47 And with that, we have concluded a long discussion of short bowel syndrome.
About the Lecture
The lecture Short Bowel Syndrome and Bile Acid Malabsorption by Richard Mitchell, MD, PhD is from the course Small and Large Intestines Disorders.
Included Quiz Questions
What is the most common etiology of short bowel syndrome?
- Surgical resection of the bowel
- Crohn disease
- Radiation enteritis
- Celiac disease
- Irritable bowel syndrome
Which of the following is NOT a common symptom of short bowel syndrome?
- Decreased reflexes
- Diarrhea
- Steatorrhea
- Weight loss
- Heartburn
Which of the following is a possible physical examination finding in a patient with short bowel syndrome?
- Tenting of the skin
- Rapid, irregular heart rate
- Clubbing
- Cherry-red spot
- Painful lump in the tongue on palpation
What is the acute-phase management of short bowel syndrome?
- IV fluids and electrolyte replacement
- H2 blocker
- PPI
- Enteral nutrition
- Gastric acid suppression
How long should gastric acid suppression continue?
- 6 months
- 12 months
- 3 months
- 18 months
- 24 months
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |