Playlist
Show Playlist
Hide Playlist
Seborrheic Dermatitis: Diagnosis and Management
-
Reference List Pathology.pdf
-
Slides Seborrheic Dermatitis Diagnosis Management Dermatopathology.pdf
-
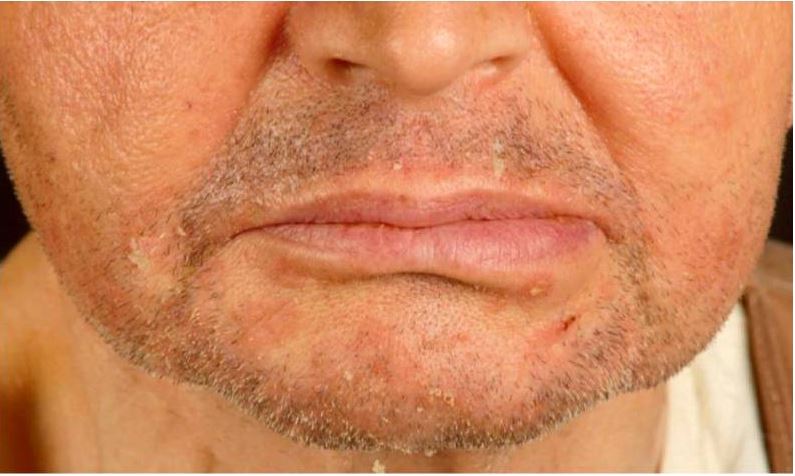
Download Lecture Overview
00:01 The clinical presentation are pruritic. 00:04 They're itchy, erythematous papules, again erythematous because of increased vascular dilation and plaque. 00:12 So it's not just little tiny pimple-like things, but things that are more extensive. 00:16 They're easily detachable. 00:17 They're greasy because of all the sebum that is there. 00:21 They have a yellow crust again because of the sebum. 00:24 And they come and they go depending on stress, temperature and other factors. 00:31 In infants will typically appear on the head. 00:35 And so you will get something that's called cradle cap. 00:38 Can also involve the eyebrows, eyelids around the mouth, etc., and onto the neck and trunk. 00:46 In adults, it tends to be more localized to the face and to the scalp. And remember I said at the very beginning, dandruff is seborrheic dermatitis. 00:56 And so what we'll see is you may not see the kind of greasy stuff on the scalp, but you will see flaking scales. 01:03 And that's that white dandruff that we kind of get off our shoulders. 01:07 On the face it will involve the eyebrows, the space between the eyebrows and the nose, the glabella, the eyelids, sides of the nose, nasolabial folds, why those areas, because that's the highest density of sebaceous glands, and then the mustache and the beard area. 01:23 And you can improve that if it's in those areas by shaving, because you remove some of the forest of hair, that's going to allow the fungus to survive and keeps the sebum from being washed away. So in patients with HIV, the lesions may be very widespread. 01:43 They may be very difficult to control. 01:46 It can also be a marker for the onset of disease, sudden severe onset uh seborrheic dermatitis in atypical areas or treatment resistance. 01:57 And then when we give antiretrovirals and get the HIV burden under control and the normal CD4 counts recover, then the lesions tend to remit. With regard to diagnosis, it's going to be mostly the clinical appearance. Biopsy can be used. 02:13 But as we'll talk about in a moment, it's fairly nonspecific. 02:17 The clinical appearance is the kind of greasy yellow red plaques in the characteristic distribution between the eyes, above the nose, the eyebrows around the mouth, etc. The histologic image is showing kind of the changes that can occur within a heightened inflammatory response to the fungus. 02:40 And what you'll see is a slight acanthosis or thickening of the stratum spinosum layer. 02:48 Disordered maturation. 02:50 So we're seeing nuclei within the stratum corneum so that those nuclei shouldn't be there. That's the parakeratosis. 02:57 We're also seeing a slightly increased inflammatory infiltrate again responding to the elevated levels of the fungus that's driving this entire process. 03:09 And as part of the inflammatory response to cytokines, we're seeing spongiosis or edema within the epithelium. 03:18 That's all kind of nonspecific. 03:20 So although biopsy can be helpful it's not usually done. 03:25 The management. Well, the management kind of, now that you understand why this is happening, you can pretty much tell me why, how we should approach it, the therapy. 03:38 So you can if there's medications that are triggering it, then we can discontinue those. 03:42 We can treat associated comorbidities, infections, etc. If alcohol intake is involved, because of the increased sebaceous gland proliferation and sebum production, we can reduce that. We can, in severe cases or more severe cases, intervene with things that are more pharmacologic. 04:04 So we can use Head and Shoulders shampoo, selenium sulfide, that has antifungal properties for the seborrheic dermatitis of the scalp. Uh, certain compounds. 04:17 Tar. I'm not talking about tar that you would put on a road bed, but in fact, some of the compounds in tar will decrease inflammation and have antifungal properties, sulfur agents, salicylic acid, and zinc pyrithione. 04:33 All of those will have antifungal activities and or will help to remove some of the expansive keratotic cells. 04:47 Antifungals clearly will be effective since the Malassezia species are the main drivers of this. They can be topical or systemic. 04:55 For very severe refractory disease, we can give anti-inflammatories, which can also be helpful, and calcineurin inhibitors such as cyclosporin can be used for delicate areas where you don't want to use topical steroids for prolonged periods of time, things like the face. And with that, a discussion of seborrheic dermatitis that hopefully has been edifying and not too flaky.
About the Lecture
The lecture Seborrheic Dermatitis: Diagnosis and Management by Richard Mitchell, MD, PhD is from the course Inflammatory Lesions of the Skin.
Included Quiz Questions
Which facial areas are most commonly affected by seborrheic dermatitis in adults?
- Eyebrows, glabella, and nasolabial folds
- Forehead and chin only
- Cheeks and temples
- Ear lobes and neck
- Entire face uniformly
Which description best characterizes the typical appearance of seborrheic dermatitis lesions?
- Greasy yellow-red plaques with easily detachable scales
- Dry silver scales with sharp borders
- Purple papules with central clearing
- Brown macules with irregular edges
- Clear vesicles with surrounding erythema
Which topical agent works primarily through antifungal properties in treating scalp seborrheic dermatitis?
- Selenium sulfide
- Salicylic acid
- Benzoyl peroxide
- Coal tar
- Zinc oxide
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |