Playlist
Show Playlist
Hide Playlist
Role of Interleukin 1 (IL-1) and Tumor Necrosis Factor-α (TNF-α) in Lymphocyte-macrophage Activation
-
Slides Acute and Chronic Inflammation Recruitment of Macrophages.pdf
-
Reference List Pathology.pdf
-
Download Lecture Overview
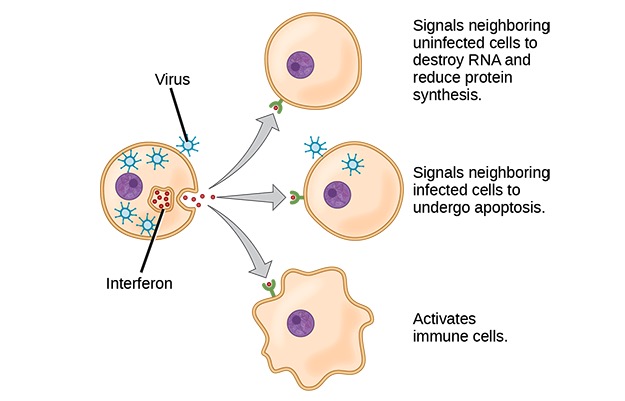
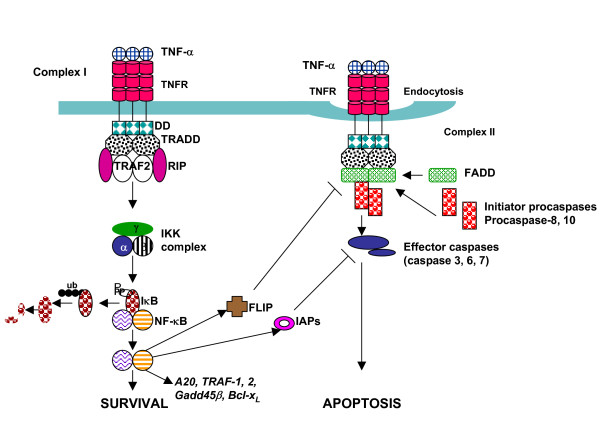
00:00 Okay, so what the activated macrophages do? This is going to be a summary slide. 00:04 There are kind of five separate things. 00:06 And we'll talk about the factors that do this. 00:09 So macrophages, as I've said many times are the definitive cleanup crew. 00:13 Neutrophils started the process. 00:15 Yes, they did, but they died after 10 hours. 00:19 So they didn't get very far. 00:22 Macrophages are going to remove and completely degrade all the injured tissue and debris. Okay. 00:28 They are going to finally, completely, definitively sterilize the area. 00:33 So, they have a lot of antimicrobial activity. 00:36 They are going to elaborate molecules that will drive the recruitment, the chemotaxis, and the proliferation of fibroblasts. 00:46 They will also drive new blood vessel formation. 00:51 And then they will direct the deposition and remodeling extracellular matrix. 00:56 So the macrophage is actually doing quite a lot. 00:59 And keep in mind, this is a combination of M1 and M2 macrophages. 01:04 So at the top, the first two are probably more M1, and the next three, probably more M2. 01:12 So the diriment process has phagocytosis. 01:15 They are elaborating things to break down matrix. 01:18 Collagenases and elastases. 01:20 Anti microbial activity driven through nitric oxide and reactive oxygen species. 01:26 Things that drive chemotaxis and proliferation of fibroblasts, transforming growth factor-beta, tumor necrosis factor, interleukin-1. 01:35 Angiogenesis, some more factors that we're going to talk about. 01:39 Let's see them right there. 01:40 We will return to those when we talk about the angiogenesis process. 01:45 And then finally, driving that deposition remodelling matrix, even more factors. 01:52 So let's talk a little bit more about lymphocyte-macrophage activation, because in the usual area where we've recruited macrophages, there are a number of T cells that are also driving the process. 02:07 And this will get us into the next set of factors. 02:11 Okay, the activated lymphocyte, as we've already talked about, makes interferon gamma amongst other things that will drive macrophages to become activated. 02:19 And we're going to make a Th1 macrophage that M1 macrophage will make other inflammatory mediators. 02:26 But in particular, we'll make interleukin-1 and tumor necrosis factor. 02:31 These are going to be key elements in driving the cycle back and activating lymphocytes. 02:38 Macrophages are also presenting antigen to T-cells. 02:41 So, it is a significant role that macrophages play in this process, in addition to the lymphocytes driving it. 02:49 So, macrophages presenting antigen, the T-cells, but also elaborating interleukin-1 and tumor necrosis factor the lymphocyte, which activates it. 02:58 So we have a complete cycle. 03:01 I don't see on this slide, any mechanism by which we turn this off, it's really important to recognize that there are pathways not shown here, where we are also anti-inflammatory, and we resolve this. 03:13 Otherwise, this would just keep going on, and on, and on in a big circle. 03:18 Okay, I'm going to emphasize now, interleukin1 and TNF. 03:23 So, these are the cytokines made by an activated macrophage unlike any many others, that are going to activate lymphocytes, and also other cell types. 03:34 Now, "Factor 2" Okay, so, we had factor 1, and again, not in the textbooks, just for this discussion. 03:40 Factor 1 was interferon gamma, driving the activation of M1 macrophages. 03:44 Factor 2 is made by the activated macrophage, driving lymphocyte activation. 03:51 I've actually combined two cytokines into one Factor 2. 03:56 Interleukin-1, and tumor necrosis factor have similar activity profiles to each other. 04:03 Just another example of the redundancy of the immune system and our body in general. 04:08 So they have similar activity profiles, that's why we can lump them together. 04:13 They are synthesized importantly, by macrophages, other cell types do <inaudible> synthesize them, but for this discussion, it's all about the activated macrophage. 04:24 What does interleukin1 and TNF do? Well, in fact, you have all experienced the systemic effects of interleukin1 and TNF. 04:33 The last time that you had a cold and felt like you were going to die. 04:37 You all you wanted to do was sleep, you had a fever, you didn't want to eat, your joints ache, your muscles ache, it felt like death warmed over. 04:45 That's interleukin1 and TNF from activated macrophages. 04:51 Who knew? Now, you do. 04:53 So these are parts of an acute phase response driven by factor 2 here, and include fever, and sleep, and anorexia. 05:03 If you think about it, these probably have important roles in recovering or responding to infections. 05:11 Although, they may be somewhat counterintuitive. 05:16 Interleukin-1 and TNF also induce other cells around the body to do various things. 05:24 And when they are present in the setting of chronic inflammation, they induce the liver to produce complement and coagulation factors. 05:34 These are called acute phase proteins. 05:38 There are many other acute phase proteins that come up as part of inflammation. 05:42 But for right now, we're going to just focus on the complement coagulation factors. 05:46 So it will turn on the liver to prepare the body to do battle. 05:51 It will have hemodynamic effects. 05:54 So in the local circulation, little l1 and a little TNF causes persistent vasodilation, increased vascular permeability. 06:03 If you have a lot of it systemically, it will actually cause hypotension because it's dilating the vessels everywhere. 06:11 And you will have edema kind of everywhere. 06:14 And you will go into shock. 06:16 So it can have hemodynamic effects. 06:19 It will also induce anticipating that we need to fight more neutrophils coming out from the bone marrow. 06:26 So IL-1 and TNF do a lot of very interesting things. 06:29 But if you just keep in mind that feeling that you thought you were gonna die when you got sick the last time that's interleukin-1 and TNF. 06:36 And if we'd measured in your bloodstream at the same time, you would have seen that your coagulation factors were more synthesised, your complement was up, and you probably had slightly lower blood pressure and more neutrophils. 06:49 These factors also activate the endothelium. 06:52 To make it more sticky. 06:53 This is exactly what you want to have happen. 06:55 Because you want to recruit more inflammation into that area. 06:58 You are not going to be content until the infection or the injury is just beaten into submission. 07:05 We're also going to increase procoagulant activity of the endothelium because we're anticipating that in the battle to come, we're going to have bleeding. 07:14 and we don't want to bleed to death. 07:15 So you would be more pro-coagulant. 07:18 And interleukin-1 and TNF are also going to activate fibroblasts. 07:22 We're going to start the process of getting them to grow, proliferate, turnover, and make work matrix. 07:28 So that's we had factor 1, interferon gamma. 07:31 Factor 2, IL-1 and TNF kind of a twofer. 07:34 And that gets us into the next phase. 07:39 We will look at some of the other Now further events that happen in healing and regeneration.
About the Lecture
The lecture Role of Interleukin 1 (IL-1) and Tumor Necrosis Factor-α (TNF-α) in Lymphocyte-macrophage Activation by Richard Mitchell, MD, PhD is from the course Acute and Chronic Inflammation.
Included Quiz Questions
The activated macrophages M1 play a role in...?
- ...the removal of injured tissue.
- ...the proliferation of fibroblasts.
- ...the deposition and remodeling of the extracellular matrix.
- ...angiogenesis.
- ...the recruitment of smooth muscle cells.
Which of the following is involved in angiogenesis?
- Fibroblast growth factor 2 (FGF-2)
- Metalloproteinases (MMPs)
- Nitric oxide (NO)
- Tumor necrosis factor-alpha (TNF-α)
- Collagenases
Which of the following is associated with the acute phase response?
- Increased release of neutrophils from bone marrow
- Increased release of anticoagulation factors from the liver
- Decreased activity of fibroblasts
- Decreased release of complement factors
- Increased systemic vascular resistance
Which of the following plays a role in elevating the body temperature during inflammation?
- Interleukin 1
- Interleukin 10
- Interferon-gamma
- Interleukin 4
- Leukotriene B4
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |