Playlist
Show Playlist
Hide Playlist
Chest Pain: Pulmonary Embolism and Thoracic Aorta Aneurysm
-
Slides ChestPain AcuteCare.pdf
-
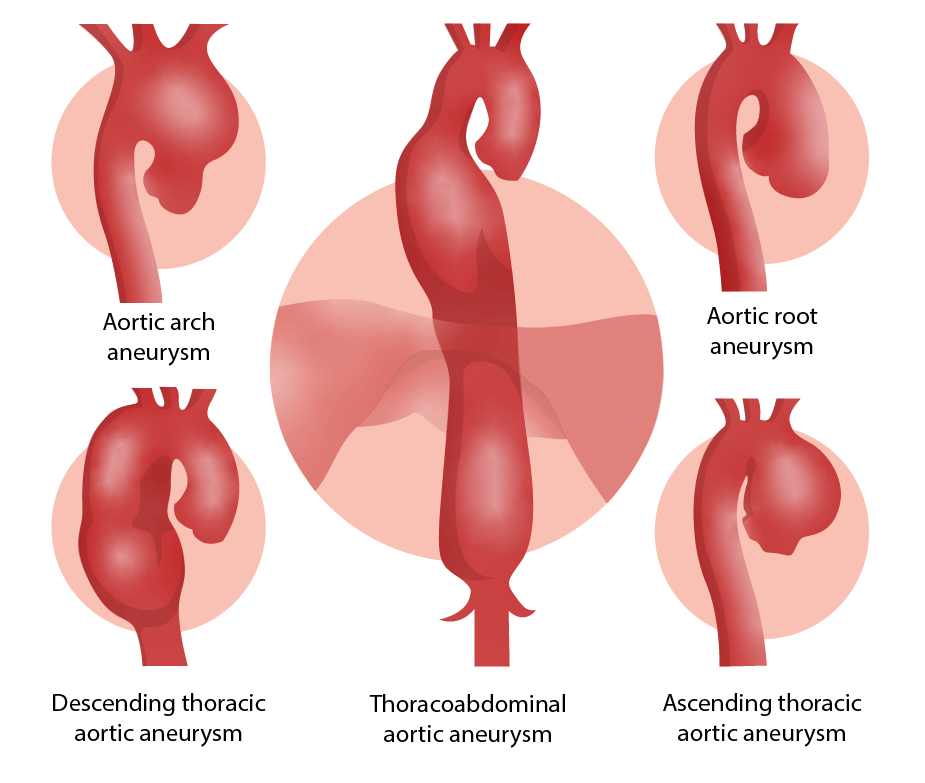
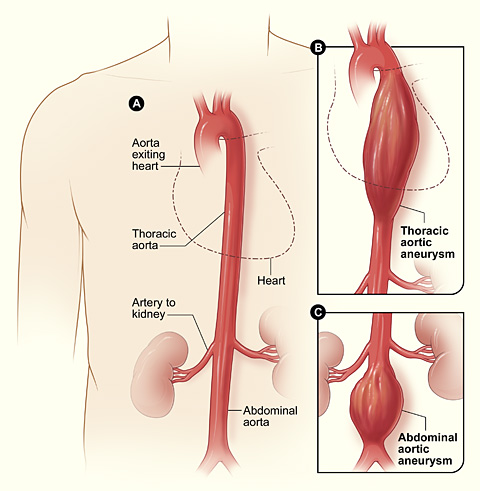
Download Lecture Overview
00:01 And one thing to always think about, it's another great imitator, is pulmonary embolism because it can mimic angina, chest pain, but it can also mimic things like heart failure, even COPD because it promotes dyspnea, promotes some chest pain, it can promote a lot of different symptoms. 00:22 There is a great tool to help rule out DVT and pulmonary embolism called the Wells’ criteria. 00:30 It’s seven items. 00:31 So, that can give you an idea of what the patient's baseline risk for a pulmonary embolism is. 00:37 If they’re low risk, it’s acceptable to do a D-dimer serum study. 00:41 The value of the D-dimer is if it's negative. 00:44 If it's positive, it doesn't really tell you a lot, but if it's negative and they have a low pretest probability for PE, the patient doesn't necessarily need any further workup. 00:54 This is a patient you’ve evaluated, you’ve listened to them, they don't have any of the other symptoms or signs they would need to have, say, a CT of the chest to evaluate for pulmonary embolism. 01:05 So, that's a quick way that you can rule out pulmonary embolism without having to do the extra step of imaging studies, but everybody who is more complex or a higher risk of some kind of thrombosis, D-dimer is not an option. 01:23 They should get a full scan. 01:26 Let’s move on to thoracic aortic aneurysms. 01:28 The classic is a tearing pain that goes through to your back. 01:32 That's the difference in this one. 01:34 It is more rare than either angina or pulmonary embolism, but it can be just as deadly. 01:40 One thing to look out for, depending on where the tear is, you might actually get to measure a difference in the brachial blood pressures. 01:50 So, therefore, if this is suspected, always get a blood pressure in both arms and a differential of 20 points or more is significant and should merit further evaluation. 02:01 CT scan of the chest is the evaluation of choice. 02:06 Some other considerations, just briefly, among patients with chest pain, just remember, panic attacks – having chest pain with panic attacks, very, very common overall and a lot of people have panic disorder. 02:16 Pericarditis is more rare. 02:18 It’s going to produce kind of a generalized pain that's persistent. 02:24 Not like angina where it comes and goes, not in a simulated exercise. 02:27 Can be related to position. 02:29 What you want to see on EKG is either the classic diffuse ST segment elevation or you can also see diffuse PR depression with no T-wave elevation as well. 02:40 So, those are signs of pericarditis. 02:42 And that really – the pericarditis, remember, that goes through all the leads. 02:46 That’s the thing that separates pericarditis from other conditions that cause EKG changes. 02:51 It’s one of the ones that promotes ST changes or PR depression across all leads on your EKG. 02:59 So, overall, just to summarize, a good history looking at those cardiovascular risk factors, a good description of the type of pain that patients are having, how persistent it is, the character of the pain and then a focused physical examination, particularly focusing on chest wall tenderness can be really helpful. 03:18 An EKG is done most of the time in my practice. 03:21 It's a simple test to do, It’s very low risk. 03:24 It's cheap and it's available. 03:26 And so, many patients get an EKG and that will tell us a little bit more about what's going on, put their risk stratification in the appropriate place. 03:35 But I try to be parsimonious with my use of other types of studies, including CT scans, even echocardiography. 03:44 I try to be much more selective with those because many patients don't require them. 03:48 But certainly the ones who are – who appear ill where it just doesn't seem like things are adding together and they do have at least some probability of one of these more serious diagnoses, aneurysm, PE, unstable angina, they should be transferred to the emergency department for further evaluation. 04:09 So, with that, hopefully, you feel a lot more confident in managing chest pain. 04:12 Look forward to seeing you next time.
About the Lecture
The lecture Chest Pain: Pulmonary Embolism and Thoracic Aorta Aneurysm by Charles Vega, MD is from the course Acute Care. It contains the following chapters:
- Pulmonary Embolism
- Thoracic Aorta Aneurysm
- Summary of Chest Pain
Included Quiz Questions
Which of the following is most appropriate next step in the evaluation or management of a patient with chest pain and a Wells criteria score of 1.5?
- D-dimer
- Treatment with heparin
- computed tomography angiography
- Ventilation-perfusion scan
Which of the following findings on ECG is most indicative of pericarditis?
- Diffuse ST-segment elevation
- Diffuse ST-segment depression
- High-amplitude R waves in the precordial leads
- Prominent U waves
- PR prolongation
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |