Playlist
Show Playlist
Hide Playlist
Types of Peptide Hormones
-
Slides CellTypesHormones EndocrinePathology.pdf
-
Reference List Pathology.pdf
-
Download Lecture Overview
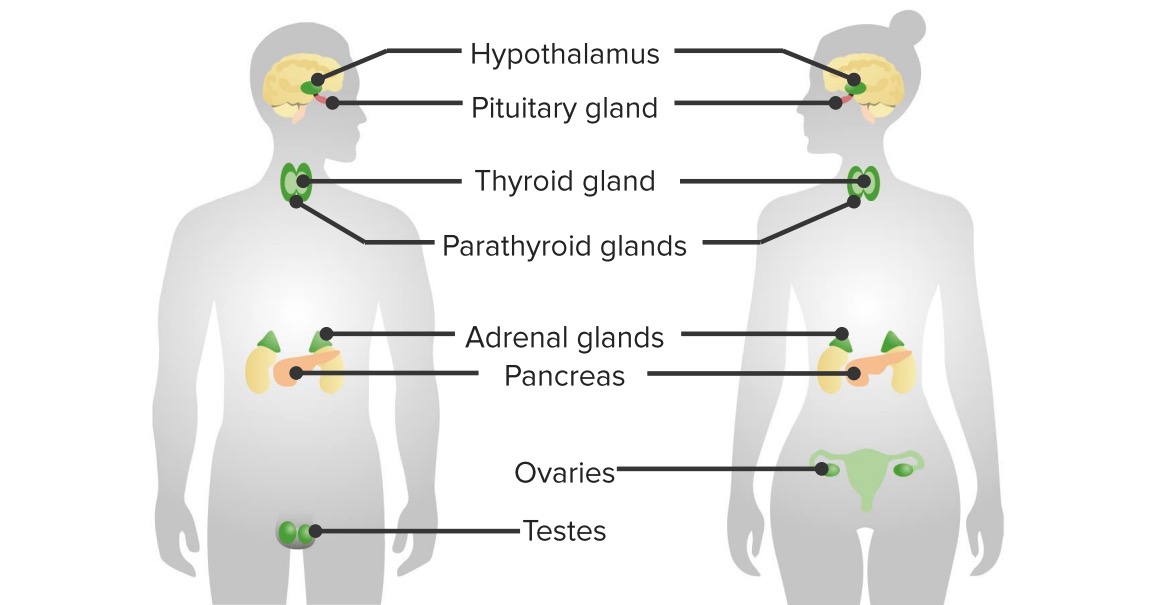
00:02 Next what we’ll do is we’ll take a look at these anterior pituitary peptide hormones and then divide it into various subgroups. 00:10 We have the glycoproteins, somatomammotropins and the proopiomelanocortin. 00:16 The glycoproteins will be important because of certain similarities between the hormones that have become really important to us and I’ll point those out to you here and I’ll keep reinforcing it throughout the entire course. 00:29 Somatomammotropins, we talked about these being growth hormone. 00:33 There is one placental hormone that we’ll refer to that behaves like a growth hormone that becomes very important to us. 00:40 So, what’s important as we go through these three structural types of your anterior pituitary hormones is where is all the sharing of the hormones taking place and what does that mean to you. 00:54 Let’s first take a look at glycoproteins. 00:57 What I’ll point out to you here in this picture are those specific glycoproteins that are important to you so that you notice as to where the sharing will be taking place. 01:07 What I mean is the following. 01:09 I’d like for you to first identify beta HCG here. 01:13 You see it. 01:14 It stands for beta human chorionic gonadotropin. 01:18 What does that mean to you? Well, you already know that that is something that is being released by a placental counterpart and when you do a pregnancy test, of course, you are always looking for beta HCG. 01:32 Okay, well, if beta HCG has been released by the placenta and your female, in fact, is pregnant, beta HCGs then works on a couple of other or behaves like a couple of hormones that become incredibly important for it to function properly and those are the following. 01:51 I want you to focus upon beta HCG, I want you to think of a pregnant woman, I want you to think about the foetus and the placenta. 02:00 Are you there? Good. 02:03 Next, well, in order for that foetus to develop within the uterus, a very important hormone that it requires so that it receives proper nourishment for growth and development is progesterone, right? Next, hmm, well, where is the foetus in the first, let’s say, eight weeks getting the progesterone from? The first eight weeks, there is absolutely no way that the foetus is going to be producing its own progesterone, right? But, it sure as heck through the placenta will be producing beta HCG and in addition, in the ovary, what did you leave behind? Remember, in the first eight weeks in the ovary, you have an empty follicle and that empty follicle is called what? Corpus luteum. 02:55 What do you call that corpus luteum? Because that entire “empty follicle” is filled with the luteinizing hormones, right, where it’s covered by luteinizing hormones. 03:08 So, therefore, that corpus luteum is responsible for secreting the progesterone that the foetus requires oh so desperately, the beta HCG. 03:19 Next, identify the LH here; is going to act upon the LH receptors and you have a nice sort of symbiotic relationship between the foetus and the maternal corpus luteum. 03:34 You’ve seen this in physiology in menstrual cycle. 03:37 If you don’t know your menstrual cycle, I would highly recommend that you go back and take a look at the menstrual cycle before we further go on with discussions in endocrinology, especially by the time we come to female repro, hmm? What else? Wow, it’s interesting too is that beta HCG which is found in the first eight weeks or so can also behave like another hormone and it can behave like TSH... 04:04 TSH, it can. 04:06 And how important is thyroid hormone for the foetus? Well, let me put it this way. 04:12 If the foetus didn’t have thyroid hormone, what’s the pathology called? Cretinism. 04:18 So, the foetus has to have thyroid hormones at all times and my goodness, that foetus will make sure that this happens. 04:26 How does that occur? Well, it’s a fact that you have beta HCG which then works on your TSH receptors so that it gives itself proper amounts of thyroid hormones always so that cretinism does not take place. 04:41 Is that clear? It’s important that you pay attention to glycoproteins. 04:47 The similarities between beta HCG and LH and beta HCG and TSH and at some point later on, in female reproductive pathology, we’ll talk about our gestational diseases, we’ll talk a lot about human chorionic gonadotropin, won’t we? And all of these will play a role again and again and again. 05:06 Let’s take a look at the next structural type, it’s a somatomammotropin. 05:11 Remember, I told you to pay attention to the suffix ‘–tropic’. 05:16 So, this does not mean inhibitory; in fact, it means what? Promotion or promoting or secreting-secreting, right? Okay, now, we have growth hormone and this time, we have another placental hormone. 05:31 This is called prolactin. 05:33 So, growth hormone prolactin from the anterior pituitary will play a role… they will… are together known as somatommamotropins and especially, if you’re thinking about during development, once again a pregnant woman, obviously growth hormone will be playing a role as will be prolactin, especially in the female because it’s responsible for milk synthesis, right? And you know that as well because if there’s excess prolactin, which is a huge topic for us in endocrine pathology, then you know there is galacturia. 06:05 Let’s go to the foetus and the placenta. 06:10 We have a placental hormone here called human placental lactogen. 06:15 Do not confuse this with human chorionic gonadotropin. 06:19 Whatever you do, one has nothing to do with the other. 06:22 Both have huge clinical applications. 06:24 Let’s talk about human placental lactogen. 06:27 Let’s go back to the foetus again and the placenta, but this time, instead of ensuring that the foetus has sufficient amounts of progesterone and sufficient amounts of thyroid hormones with the help of what placental hormone there? Human chorionic gonadotropin, this time we have human placental lactogen. 06:52 What does this ensure that the foetus is receiving? Hmm, doesn’t the foetus require glucose? Tell me about glucose. 07:00 It crosses the blood placental barrier, that it does. 07:05 Glucose passes through a lot of barriers, it has to, ha-ha, so that you can properly nourish the target in front of you. 07:13 So, therefore, human placental lactogen behaves like a growth hormone, especially in the mother in which it renders insulin receptors resistant. 07:23 What did I just say? The human placental lactogen from the foetus then works upon the insulin receptors of the mother rendering it resistant so that the mother cannot take up the glucose, right? So then who is guaranteed the glucose? The foetus. 07:44 Amazing, huh? Move on. 07:47 Our third and final structural type will be proopiomelanocortin. 07:50 You focus upon the last two portions of this. 07:54 Melanocortin pretty much tells you everything that you need to know about your specific clinical presentation. 08:01 Really? Mm-hmm, watch this. 08:03 The cortin is going to refer to ACTH from the anterior pituitary. 08:09 What about the melano? Hold on, I’ll show you when you’ll be using melano, but I’m sure that you already know as to what I am referring to. 08:16 Now, the proopiomelanocortin, POMCs, ACTH, lipotropins, MSH and beta-endorphins, all of these are important in one... in some way, shape or form. 08:26 ACTH, for obvious reasons. 08:28 Now, melanocytes stimulating hormone, MSH, is incredibly important. 08:32 Let’s say I might as well give you the pathology. 08:36 Your patient is suffering from the following - has decreased blood pressure, is failure to thrive even and in addition to that, you take a look at the patient around the oral mucosa and you find hyperpigmentation around the oral mucosa. 08:53 What am I referring to here and what’s your next step of management? With that type of clinical presentation, no doubt I am referring to what’s known as, well, upon CT, they’ll make it a little bit easier, but then abdominal CT and you find that the adrenals are atrophic. 09:09 In other words, I’m referring to primary adrenal insufficiency a.k.a. Addison’s disease, right? Decreased blood pressure I said, I said their failure to thrive because, huh, there is no cortisol and that’s going to kill your patient... failure to thrive and I said around the oral mucosa, there was hyperpigmentation. 09:32 What’s going on here? If there is no cortisol, primary adrenal insufficiency. 09:37 Then what hormone is elevated in your patient? ACTH. 09:41 Where did it come from? POM… M, Melanocytes stimulating hormone; corticotrophin POMC. 09:49 So, therefore, that elevated level of melano is going to give you your pigmentation. 09:54 You also have beta-endorphins. 09:57 Endorphins make you feel good and hopefully by going through medicine, you are feeling good about what you’re learning. 10:04 I want your endorphins to be kicking in. 10:07 Welcome to POMC. 10:08 Now, there’s a little bit more detail here than is necessary, but I like for you to focus upon ACTH. 10:14 That top runk[ph] that you’re seeing there is proopiomelanocortin, POMC precursor. 10:21 That entire segment that is then broken up into your ACTH and beta endorphin and then you have your MSHs and MSH stands for melanocytes stimulating hormone and the endorphin that you want to know is your beta-endorphins and of course, your ACTH. 10:40 These are the three structures that you want to take out of your POMC segment and therefore, giving you your pathologic... well, not just pathologic, pathologic and physiologic presentations of your patient based on the circumstances. 10:55 We talked about Addison’s, we talked about beta-endorphins. 10:57 ACTH works upon the adrenal cortex. 11:02 You have two different types of… three different types technically of your MSH, you focus upon the beta and the alpha-MSH and at times may, may be referred to as an appetite suppressant, especially the alpha and the beta endorphins of course referring to your opioid peptides.
About the Lecture
The lecture Types of Peptide Hormones by Carlo Raj, MD is from the course Pituitary Gland Disorders.
Included Quiz Questions
Which feature is NOT shared by human chorionic gonadotropin (hCG), luteinizing hormone (LH), follicle-stimulating hormone (FSH), and thyroid-stimulating hormone (TSH)?
- An anterior pituitary origin
- A glycoprotein structure
- Classification as a hormone
- An alpha subunit
- Consist of an alpha and beta subunit
Which somatomammotropin is released from the anterior pituitary?
- GH
- HPL
- LH
- FSH
- TSH
What is the placental somatomammotropin?
- Human placental lactogen
- Growth hormone
- Prolactin
- Human chorionic gonadotropin
- Luteinizing hormone
Adrenocorticotropic hormone is increased in Addison's disease. Which other hormone is most commonly increased in this disease?
- Melanocyte-stimulating hormone
- Human placental lactogen
- Human chorionic gonadotropin
- Growth hormone
- Luteinizing hormone
What is not a proopiomelanocortin gene product?
- Thyroid-stimulating hormone
- Adrenocorticotropic hormone
- Melanocyte-stimulating hormone
- Beta-endorphins
- All of the answer choices are correct
Which statement regarding peptide hormones is INCORRECT?
- They all share a similar β subunit.
- Luteinizing hormone, follicle-stimulating hormone, and thyroid-stimulating hormone are secreted by the anterior pituitary.
- Human placental lactogen is a somatomammotropin released from the placenta.
- Adrenocorticotropic hormone is an example of a proopiomelanocortin gene product.
- Adrenocorticotropic hormone and melanocyte-stimulating hormone are derived from a common precursor.
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |