Playlist
Show Playlist
Hide Playlist
Pediatric Rhabdomyolysis
-
Slides Rhabdomyolysis Pediatrics.pdf
-
Download Lecture Overview
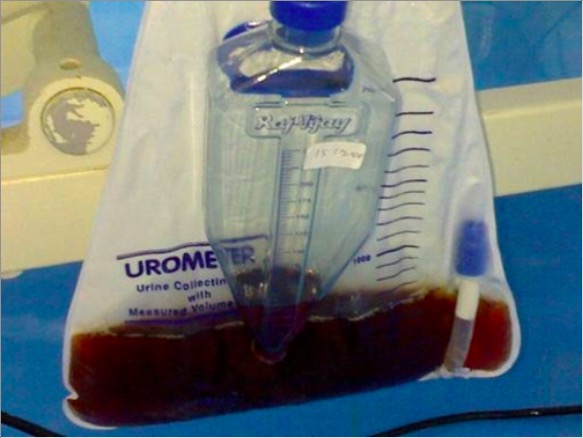
00:01 In this lecture, we’ll discuss rhabdomyolysis. 00:05 So rhabdomyolysis is caused essentially by massive muscle cell destruction. 00:11 This massive muscle cell destruction results in a release of intracellular contents into the blood, so that in turn causes myoglobin to go into the blood and then it is often peed out. 00:25 And it’s the urination that can cause problems. 00:27 So what causes a massive muscle cell breakdown? Well, there is traumatic causes such as a crush injury or immobilization. 00:37 Additionally, patients may have rhabdomyolysis from exertion. 00:42 This is particular likely among patients with sickle cell trait or patients with myopathies. 00:48 Additionally, patients may just be weekend warriors. 00:52 They are hanging out a lot during the day, during the week they are not working much, and on the weekend they decided to do some very hardcore physical activity which causes muscle breakdown. 01:03 Extreme exercise can do this. 01:05 We sometimes see this, for example, in marathon runners. 01:08 And prolonged seizure can also cause an exertional rhabdomyolysis. 01:14 Lastly, there are some other common causes of rhabdo. 01:18 One for example is influenza. 01:21 We are not really sure why, but the flu virus can often cause significant muscle pain and rarely that can in turn result in rhabdomyolysis. 01:32 Patients with myositis or inflammation of the muscle can certainly get rhabdo. 01:37 Also occasionally drugs of abuse especially stimulants can cause a rhabdomyolysis. 01:44 Lithium can do it and also malaria can do it. 01:48 Snake venoms can rarely cause a rhabdomyolysis and in particular, pit vipers. 01:53 Also hypokalemia in of itself can cause muscle breakdown and a rhabdomyolysis. 02:00 So how do patients typically present? Well, they are having muscle breakdown and that tends to hurt. 02:07 So these patients do tend to have myalgias. 02:11 Also they will note that their urine color has turned dark red or brown. 02:15 This is the myoglobin coming out in the urine. 02:19 These symptoms are usually consistent with an underlying problem. 02:22 So if a patient has, for example, underlying dermatomyositis, they should have symptoms of dermatomyositis as well. 02:32 Generally, we worry about rhabdomyolysis if the CPK or creatinine phosphokinase is over 10,000. 02:40 Those patients may be at risk for renal damage. 02:43 We are not really confident about that 10,000 mark, but it seems like a reasonable place to draw the line in the sand and say, "Now we should worry about this patient’s kidneys." Rarely, in very severe rhabdomyolysis, patients may have a high potassium or a high phosphate as a result of release of those intracellular contents. 03:03 If there is renal involvement, patients will have a high BUN and creatinine. 03:08 What I mean to say is, with very high levels of CPK, usually around 50,000 or greater, patients can end up in renal failure and that’s what we worry about in this condition. 03:19 Urinalysis will, of course, show myoglobin if you’re worried about a patient with rhabdomyolysis. 03:27 So how do we manage rhabdomyolysis? The key thing is aggressive IV hydration. 03:35 We want to give IV hydration at very high rates so that we’re keeping the urine dilute. 03:41 That prevents the renal damage from the myoglobin. 03:45 So we’re going to give sometimes as much as 2 times maintenance IV fluids, so that we can get that CPK down low and the patient will gradually get better. 03:55 Previously, you may have read somewhere about the alkalinization of the urine. 04:00 We used to believe that by adding bicarbonate to the IV fluids, you may reduce renal damage. 04:07 It turns out this isn’t really in fact really effective. 04:10 So nobody's really doing this anymore, but you might see that in older texts. 04:15 What’s key about rhabdomyolysis is managing the hyperkalemia or other electrolyte abnormalities. 04:21 Usually if it’s severe, it’s usually not necessary. 04:26 For renal injury, we’re going to follow creatinine and in very severe cases, dialysis may be required. 04:33 So that’s my review, very briefly, of rhabdomyolysis. 04:36 Thanks for your attention.
About the Lecture
The lecture Pediatric Rhabdomyolysis by Brian Alverson, MD is from the course Pediatric Nephrology and Urology.
Included Quiz Questions
Which of the following is the most appropriate initial step in the management of acute rhabdomyolysis?
- Aggressive intravenous hydration
- Intravenous calcium
- Intravenous mannitol
- High-dose furosemide
- Peritoneal dialysis
Which of the following is NOT a typical feature of rhabdomyolysis?
- Hypophosphatemia
- Myoglobinuria
- Hyperkalemia
- Elevated creatine phosphokinase
- Azothemia
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
Excellent lecture: simple, clear and concise. Thank you! It's good to have the rule of thumb for the IV hydration.