Playlist
Show Playlist
Hide Playlist
Panniculitis: Diagnosis and Management
-
Reference List Pathology.pdf
-
Slides Panniculitis Diagnosis Management Dermatopathology.pdf
-
Download Lecture Overview
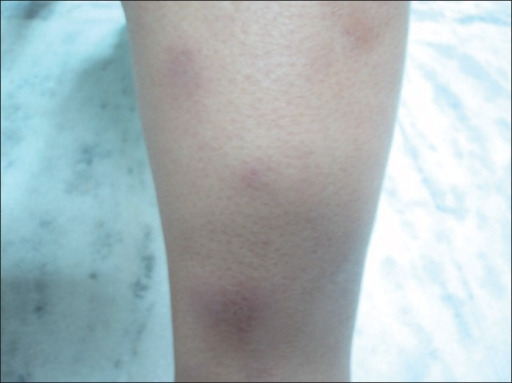
00:01 non pliable. So the clinical manifestations kind of what you would expect there's going to be nodular inflammation. 00:06 So there's going to be discrete areas of of inflammation that are red, raised, indurated, warm, and they may be painful because we are releasing inflammatory mediators that are also going to stimulate neural responses. 00:24 There may be depending on the degree of inflammation, destruction and interaction with the vessels we may compromise blood flow. 00:32 So there could be cutaneous ulceration. 00:34 We may have atrophy of the skin because it's just not getting an adequate blood supply, or that inflammation may be percolating up from the subcutaneous fat into the dermis, leading to scarring, a diffuse sclerosis. 00:49 Again, depending on the cause, whether it's infection or it is localized or whether it is autoimmune, you may have systemic manifestations including fever, arthralgias, myalgias, weight loss, night sweats, things like that. 01:06 The diagnosis is based on its appearance. 01:11 So you very classically a woman, middle aged woman on her legs, has these painful red raised nodules. 01:21 And we say, I think this is panniculitis. 01:24 A specific diagnosis requires that we actually do a biopsy and the entire full clinical context. 01:30 So the biopsy also it's not going to be superficial. 01:33 We want to get way down below the epidermis. 01:36 So this is going to be something that goes down several millimeters to get into the subcutaneous fat. So that we can look at the vessels and see whether there's a vasculitis and see whether it's nodular or septal, because that puts us in kind of two general frameworks for thinking about the causes and so on. Biopsy. 01:55 We've clearly here gotten down into the subcutaneous fat. 01:58 So this is a good deep biopsy. 02:00 You see the adipocytes those cleared out areas and then you see around it inflammatory cells and fibrosis. 02:06 So this is an example that we'd seen on a previous slide of nodular panniculitis. 02:11 And whether things are septal or nodular kind of put us into general categories. 02:16 As to causation. We also clearly want to evaluate, evaluate for the presence or absence of vasculitis. 02:24 A vasculitis will tend to infer that this is an autoimmune disorder versus something else. In this particular case, we were able to demonstrate the agent that caused this panniculitis. 02:37 This is Leishmania, which is an uncommon cause, but nevertheless is a real cause. 02:42 And we can see the the organisms that are circled in red. 02:46 So how do we manage it? Well, it really depends on what's causing it. 02:50 If it's autoimmune we may want to go with anti-inflammatories. 02:54 If it is infectious, we clearly want to treat the infectious agent and not give autoimmune or anti-inflammatory agents, because that would be the wrong thing to do. Um, in some cases, such as erythema nodosum, which tends to be self-limited, you just wait and see and provide kind of counseling and symptomatic relief to the affected individual. 03:18 And with that, we've talked about something very deep to the skin. 03:23 Not just skin deep but deep to the skin. 03:26 Panniculitis.
About the Lecture
The lecture Panniculitis: Diagnosis and Management by Richard Mitchell, MD, PhD is from the course Inflammatory Lesions of the Skin.
Included Quiz Questions
Which physical finding best characterizes the nodular inflammation in panniculitis?
- Red, raised, indurated, warm and painful nodules
- Flat, scaly, white patches
- Small, fluid-filled vesicles
- Dry, flaky, itchy plaques
- Superficial erosions
Which histological finding best helps differentiate autoimmune from other causes of panniculitis?
- Presence of vasculitis
- Depth of inflammation
- Amount of fibrosis
- Number of adipocytes
- Septal involvement
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |