Playlist
Show Playlist
Hide Playlist
Optic Disorders and Visual Field
-
Slides OP Vision Disorders.pdf
-
Reference List Pathology.pdf
-
Download Lecture Overview
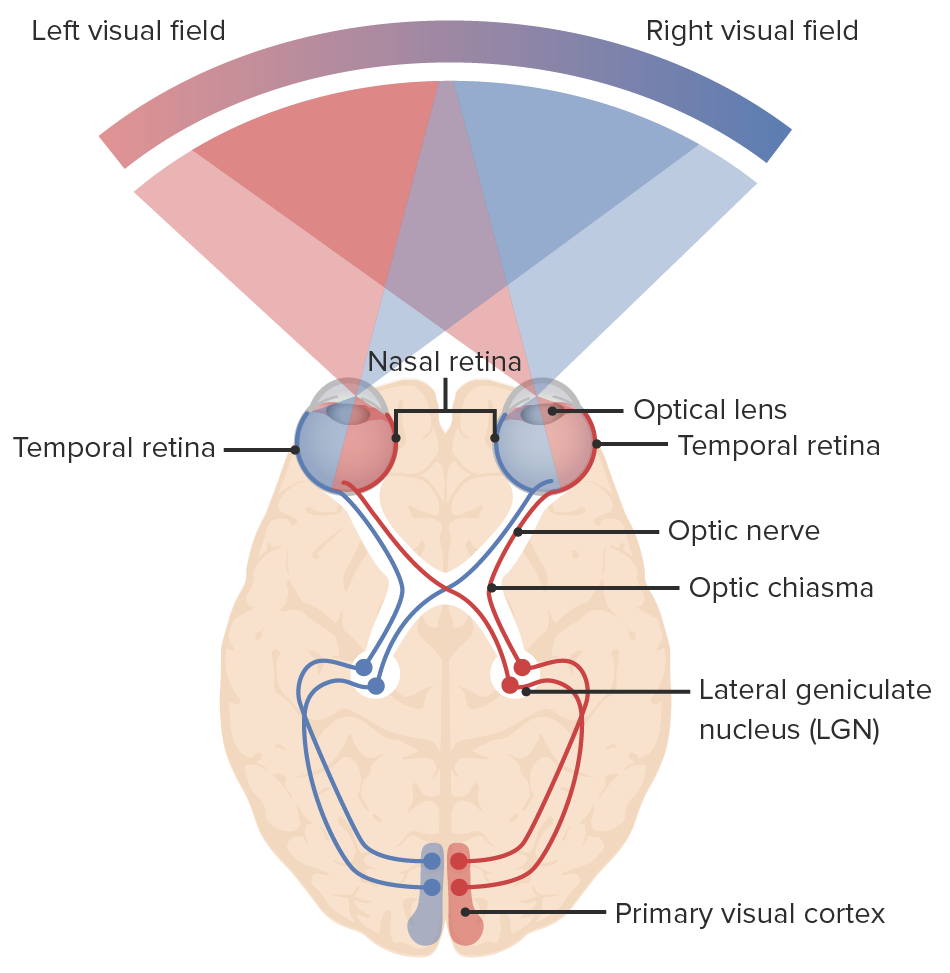
00:00 Welcome back. We're going to now explore how the visual information gets from the eyes back into the visual cortex. And this involves some gymnastics. We have to think in a mirror because things get flipped as they go through the eyes and then they get flipped again when we re-sort things out in the visual cortex. So you may have to watch this 2 or 3 times, I hope you enjoy my voice because this is complex. But it will also, if you do a really good visual exam and see where patients have field cuts, you can be quite specific in saying where the defect is. With that, we're often running. We're going to see this kind of image over and over again. Again, I want to acknowledge the efforts of Dr. Jose Mata who worked really hard to make this as understandable as possible, and so I think this is beautiful. If we think about what the eye is seeing, you have to imagine that we're staring at this sitting upright and the top is top and bottom is bottom. And we have different kinds of circles. We have a solid red circle, we have a dotted red circle. We have a solid green circle, and a dotted green circle, solid and dotted all the way around, top and bottom. And that's what the eyes are looking at on either side, it's that same image. When it goes through the lens, it all gets inverted side to side, top to bottom. And so what is being seen on the back of the retina indicated all the way on the right hand side, is that what used to be on the bottom is now on the top in terms of the representation and what used to be on the right hand side is now on the left hand side. So again, if you follow along with the solid lines, the green lines, the dotted lines, all of that you'll see that things have flipped entirely, it's through the looking glass, it's Alice and following the rabbit down the hole. Okay, we are looking at the way that the retina saw what was represented in real life. Okay, and then all that information has to be relayed back to the visual cortex and reassembled. Okay, we get into some anatomy and this is a good review at least of the visual pathways. So, the lateral representation of the right eye, the medial representation of the left eye is all going to be in green, again because of the way that the fields have changed. Alright. And you will have solid green and you will have dotted green depending whether it's coming from the top of the visual field or the bottom of the visual field. Perfect. Okay. so this is coming out of the optic nerve and you can follow those tracks and you can see solid red lines, dotted red lines. Dotted green lines, solid green lines. And that's being the representation of what was seen in the original field all the way on the left. Okay. Take a little time. Keep that in your mind. That's coming out of the optic nerve. Now, the information from the medial portion of each eye. So for the right eye it's the red field, from the left eye it's the green field. That information crosses in the optic chiasm. Okay, so we're bringing everything that's green, everything that was originally on the left hand side of our visual field. We're bringing it up into the right visual cortex. 03:39 And everything that was on the right hand side of our original visual field is going to the left visual cortex because that information is crossed in the optic chiasm. Okay. One step further back in the process. So, the top of the visual field represented in solid, the bottom of the visual field demonstrated in dotted. Same thing for the red top and bottom. Okay, so we've got that in terms of those various tracks. Okay, one step beyond the optic chiasm in the way that the visual information will travel is the lateral geniculate nucleus. And the lateral geniculate is actually going to split the information, the green information for example on the top is going to be split in 2 things that go to the bottom of the visual field and the top left of the visual field. There's going to be an extra little bend that we're going to have to pay attention to because defects or injury in that area will affect just 1 quadrant of what the eye is looking at. So the lateral geniculate nucleus has got some processing. We have our optic radiations coming out of the lateral geniculate and it goes up to the top of the visual field or to the bottom of the visual field depending on which optic radiation you're talking about. And then, so we're also, again just in another way to think about it you have the superior and inferior portions of our optic radiations. Okay, good. That extra loop that's going to the superior portion of what was originally represented of our optic radiations goes actually through the temporal lobe. So injury to the temporal lobe may give us a superior field cut. Okay, I think at this point we've got all the anatomical stuff laid out and again you may want to rewind this and go through it again to make sure that you kind of understand in a visceral way how these things are going. Because it is complex, but it's really cool. It's really cool. Okay, so now we're going to talk about various visual field cuts. These are anopsias, not being able to see, anopsia. Good. So you can have a right visual field loss, the entire right eye goes if we transect or injure the optic nerve coming out of the right eye. Gee, that's kind of a no brainer. It's very easy to understand. Right? And because of the way that this has now been drawn, you can see which parts of the subsequent radiation from that cut had been affected because they're no longer red or green, they're black. 06:24 So you will completely wipe out the top and bottom of the visual field in that eye and the right and left in that visual field in that right eye. Okay. so, that's right anopsia or visual loss. Let's do bitemporal hemianopsia. Bitemporal hemianopsia. So that means that both of the temporal, the lateral fields have been cut. And this is by having a defect, an injury at the optic chiasm. Classically, this occurs with pituitary tumor. So sitting right at that point where the red bar is, there is pituitary and if the pituitary gets too big it presses on the optic chiasm and all the nerves that are crossing in there get compressed and the patient will have bilateral field cuts so they can see ahead perfectly well, but they can't see things coming in from the side. So that's bitemporal hemianopsia, and that's due to a defect right there at the optic chiasm. And again, you can follow and see which lines had become blacked out and it becomes obvious then why you would have blacked out areas in your respective visual fields. Excellent. Still with me, right? Okay, let's do left homonymous hemianopsia. So this is now the left field on both sides, not the temporal field but the left side of both sides. And that's by getting those optic radiations coming out of the lateral geniculate nucleus. And again, you can see what's being lost, it's the bottom left of the visual field and the top left of the visual field. Okay, that makes sense and you can have obviously right homonymous hemianopsia if we get the other side, if we get the optic radiations that are going from the right visual fields bottom and top. Okay, now, suppose I only hit right there at that loop, remember, that little loop that's coming out. Alright. So you can have a defect say in the right Meyer's loop, that's going to give you a quadrant defect. So only kind of the upper outer quadrant is going to be affected. So this will be a left homonymous superior quadrant anopsia due to injury to that right Meyer's loop. You can also have it superior. Okay? Just depends on which other radiating segments is coming back in these radiations. And obviously, you can have it on the right side as well just depends on where we have that lesion. If we have lesions all the way to the back, so this is a specific instance and it's going to require some very sophisticated visual assessment in order to pick this one up. But instead of having a homonymous hemianopsia, okay, with entire field cut all the way through, the area around the macula is preserved. So, central vision is well preserved and that's why we have that white in that area. And what's happening is that we had a specific defect that's only affecting the posterior cerebral artery and there has been some collateral circulation so the information coming from the macula is spared. So this is a left homonymous hemianopsia with a macular sparing, it's a specific entity. But again, if you do a really good visual exam you'll be able to pick this up and see that there is central macular sparing. You can also have central problems. So you can specifically injure nerves in and around the macula and that degeneration or that injury will give you a spot right in the middle of your visual acuity. Everything else looks okay, peripheral vision is fine but you will have a central scotoma, a central defect. And then amaurosis fugax and this is due to abnormal or reduced vascular flow and it feels like a curtain is coming down over your visual fields. Okay. And this can happen just before you pass out from hypotension, but can also happen with a variety of other things such as vasculitides, so reduced vascular supply right there can give the entire eye that feeling of a curtain being pulled down over the top or amaurosis fugax. You can have isolated demyelinating diseases that give you very focal defects. The patient may not even be aware of them because they're so small. So, demyelinating disease as vascular injury, nerve fiber injury, etc. can give you little focal scotoma or focal defects. And with that, we've covered a very complex topic made possible through some terrific illustrations. And I do encourage you to watch it again just to hear my lovely voice.
About the Lecture
The lecture Optic Disorders and Visual Field by Richard Mitchell, MD, PhD is from the course Posterior Segment Eye Diseases.
Included Quiz Questions
What structure is associated with processing the visual representation?
- Lateral geniculate nucleus
- Caudate nucleus
- Solitary nucleus
- Lentiform nucleus
- Basal ganglia
What condition causes bitemporal hemianopsia?
- Pituitary tumor
- Pineal gland tumor
- Cerebrovascular thrombosis
- Cerebral palsy
- Glial tumor
What is the area called where the optic nerves cross?
- Optic chiasm
- Optic disc
- Meyer's loop
- Lateral geniculate nucleus
- Optic radiations
What structure is affected in the clinical finding of homonymous hemianopsia with macular sparing?
- Posterior cerebral artery
- Anterior cerebral artery
- Superior optic radiation
- Inferior optic radiation
- Middle cerebral artery
What visual defect is seen with macular degeneration?
- Central scotoma
- Hemianopsia
- Quadrantanopsia
- Anopsia
- Bitemporal hemianopsia
What visual condition is caused by a reduced vascular supply?
- Amaurosis fugax
- Optic chiasm
- Bitemporal hemianopsia
- Anisocoria
- Quadrantanopsia
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
I like that it is showing not only hemoanopsias, but also abput macula, peripheral scotomas. It is useful!