Playlist
Show Playlist
Hide Playlist
Multiple Sclerosis: Diagnosis and Treatment
-
Slides 01 Multiple Sclerosis Neuropathology II.pdf
-
Reference List Pathology.pdf
-
Download Lecture Overview
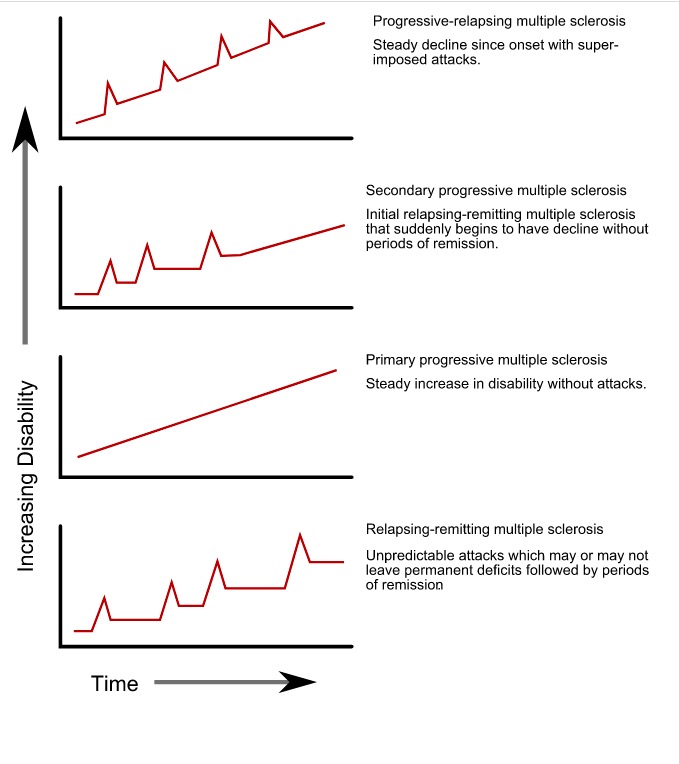
00:02 How are we gonna diagnose it… how are you going to diagnose it? CSF, mildly elevated protein. Gamma globulin is increased and most importantly oligoclonal bands. What do oligo mean? Little. So here I want you to think of your clonal bands or the bands in general and as your interpreting a band, you have these little bands called oligoclonal bands and those are quite indicative of multiple sclerosis if found by investigating the cerebrospinal fluid. 00:35 Visual evoked potentials. Remember you do have vision issues. 00:39 Useful in demonstrating evidence of prior optic neuritis but keep in mind though, frequently, the visual evoked potentials abnormalities are found and there's no history of the visual loss – just keep that in mind as well so you could have such abnormalities taking place but there is no history of optic neuritis. 00:57 These are things that you wanna put everything together, obviously, they're not just gonna give you one fact and expect you to know what's going on. 01:04 I'll give you multiple clues and then you have to make sure that you use your clinical judgment to come to the proper diagnosis. 01:12 What about treatment as such? If it’s acute relapse you're thinking about high dose IV corticosteroids and then you have disease modifying agents and these include your beta interferons. 01:25 Beta interferons, beta interferons. I'll repeat that multiple times here because you don’t want to confuse this with alpha interferons or gamma interferons – it’s your beta. 01:38 Let me add something you call glatiramer acetate and you have monoclinic antibodies Additionally, there are the sphingosine-1-phosphate receptor modulators, and other immunomodulators, such as the fumarates, and terflunomide. 01:52 In refractive cases, you do not really left with much of an option except to start using chemotherapy to drugs in other words immunosupressants and that of course has its own whole host and adverse effects. 02:04 At this point, really to agree to focus on acute relapses and disease modifying agents such as your monoclonal antibodies and the beta interferons. 02:14 It also have as I said, the glatiramer type of acetate. 02:19 To summarize your multiple sclerosis, risk factors – Caucasian, female population. 02:24 The genetic predisposition I told you about family history, may increase risks. 02:28 Preventive medicine, really we don’t know of any, really difficult unless there's a family history already. 02:34 Signs and symptoms we've talked about this quite a bit. 02:37 We talked about the blurred vision, the optic neuritis. 02:40 We talked about internuclear opthalmoplegia, the conjugate gaze type of issue. 02:44 And then also medial longitudinal fasciculus. 02:47 In addition to that there might be ataxia, numbness. Remember, CNS type of issues. 02:51 Differential diagnoses include infections maybe vasculitis and I showed you an imaging study where I showed you these plaques around your ventricles -- ventricles. 03:01 And what those plaques represent please, again, white matter degeneration. 03:07 And we've talked about the treatment. What kind of interferon? Beta interferon and glatiramer acetate. 03:13 And if it’s an acute type of relapse, then you're thinking about high dose of IV corticosteroids. 03:18 So once we've done, you've noticed now over and over again your pathology that it have these topics and these pages in which I've summarized the pinpoint information or details that you wanna take out of each one of these diseases, these are important. 03:35 Now the variants, just very quickly, I don’t want to spend so much time here. 03:39 Rarely, if ever asked, but just to make sure that you're clear, you can have neuromyelitis. 03:43 It’s called or Devic’s disease. It’s the bilateral optic neuritis, very rare but variants nonetheless – just to make sure that we're clear. 03:51 Rapid progressive in the acute this we call, Marburg form in which this is in young individual, maybe even lesser or younger than twenty. 04:02 Fulminant course during the period of several months – what does that mean? Remember, it usually takes years and decades and decades and decades for this to usual most common clinical course, my goodness, this is rapidly acting – months. 04:15 Large and numerous plaques, wide spread destruction of myelin, it’s the variants that are extremely difficult in terms of to arrive at a diagnosis quickly but nonetheless they exist for multiple sclerosis.
About the Lecture
The lecture Multiple Sclerosis: Diagnosis and Treatment by Carlo Raj, MD is from the course Multiple Sclerosis. It contains the following chapters:
- Multiple Sclerosis: Diagnose and Treatment
- Multiple Sclerosis: Summary
- Multiple Sclerosis: Variants
Included Quiz Questions
The CSF in a patient with multiple sclerosis shows an elevation in which of the following?
- Gamma globulins
- Alpha globulins
- Beta globulins
- Albumin
- Paraproteins
A 28-year-old woman presents to your office with difficulty in her left vision. An examination reveals a disorder in the conjugate lateral gaze. She does not have any medical conditions but says that she has had several episodes of shooting pain in her spinal cord for the past several months. Which of the following is most likely seen in this patient?
- CSF with oligoclonal bands
- Lymphocytic pleocytosis
- CSF with elevated beta globulins
- Decreased glucose
- Increased opening pressure
Which of the following tests can show evidence of optic neuritis that occurred in the past?
- Visual evoked potentials
- CSF analysis
- Consensual pupillary light reflex
- Fundoscopy
- MRA
Which of the following is used in the management of relapses in multiple sclerosis?
- High-dose IV corticosteroids
- Glatiramer acetate
- Beta interferons
- Natalizumab
- High-dose oral corticosteroids
Which of the following statements is most appropriate in regard to neuromyelitis optica?
- It presents with bilateral optic neuritis and prominent spinal cord involvement.
- It presents with prominent cauda equina involvement.
- It presents with unilateral optic neuritis and prominent brain stem involvement.
- It presents with prominent brain stem involvement.
- It presents with bilateral optic neuritis.
Which of the following is NOT associated with the Marburg form of multiple sclerosis?
- Bilateral optic neuritis
- Fulminant course
- Large and numerous plaques
- Widespread myelin destruction
- Young individuals
Customer reviews
4,0 of 5 stars
| 5 Stars |
|
0 |
| 4 Stars |
|
1 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
Good summary of the topic but would have been also good further discuss some of the immunosuppresive agents and fingolimod. In the dx workup section the use of MRI was also omitted