Playlist
Show Playlist
Hide Playlist
Mediastinal Areas – Lungs, mediastinum and cardiac valves
-
Slides 01 Thoracic Viscera Canby.pdf
-
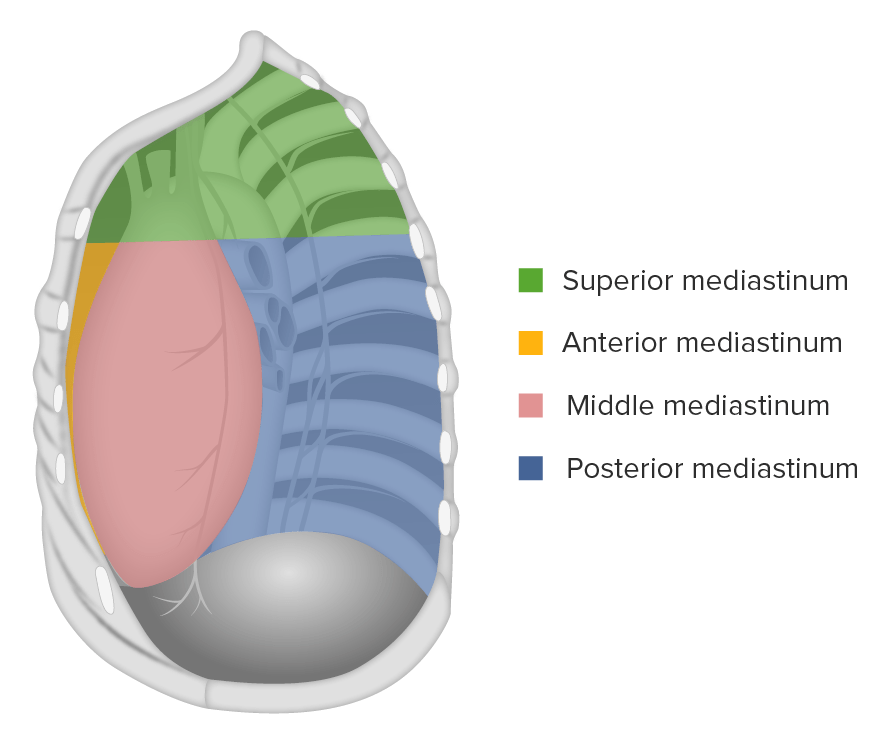
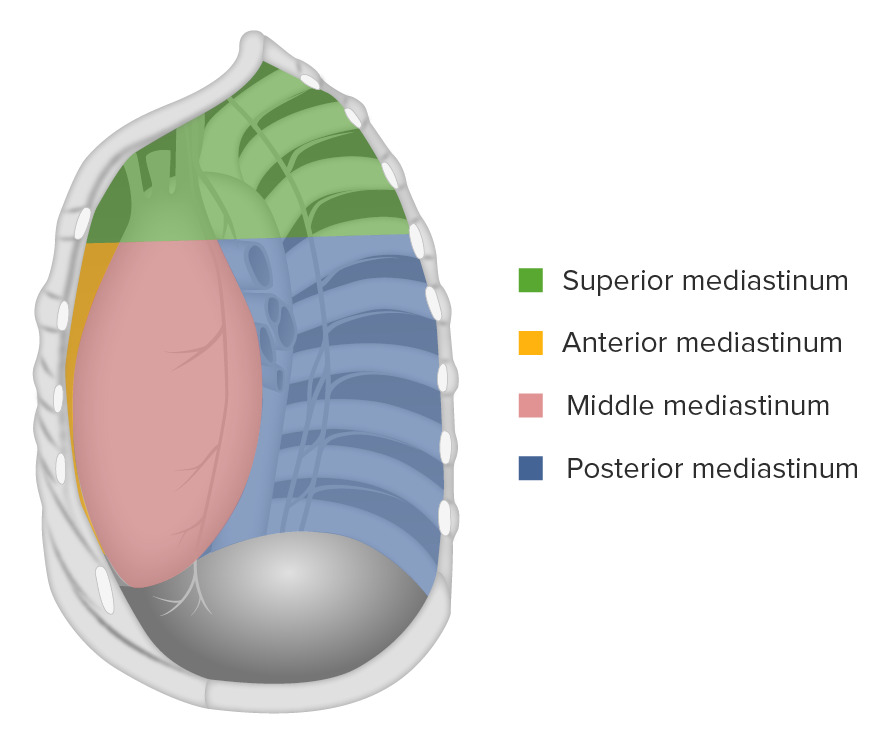
Download Lecture Overview
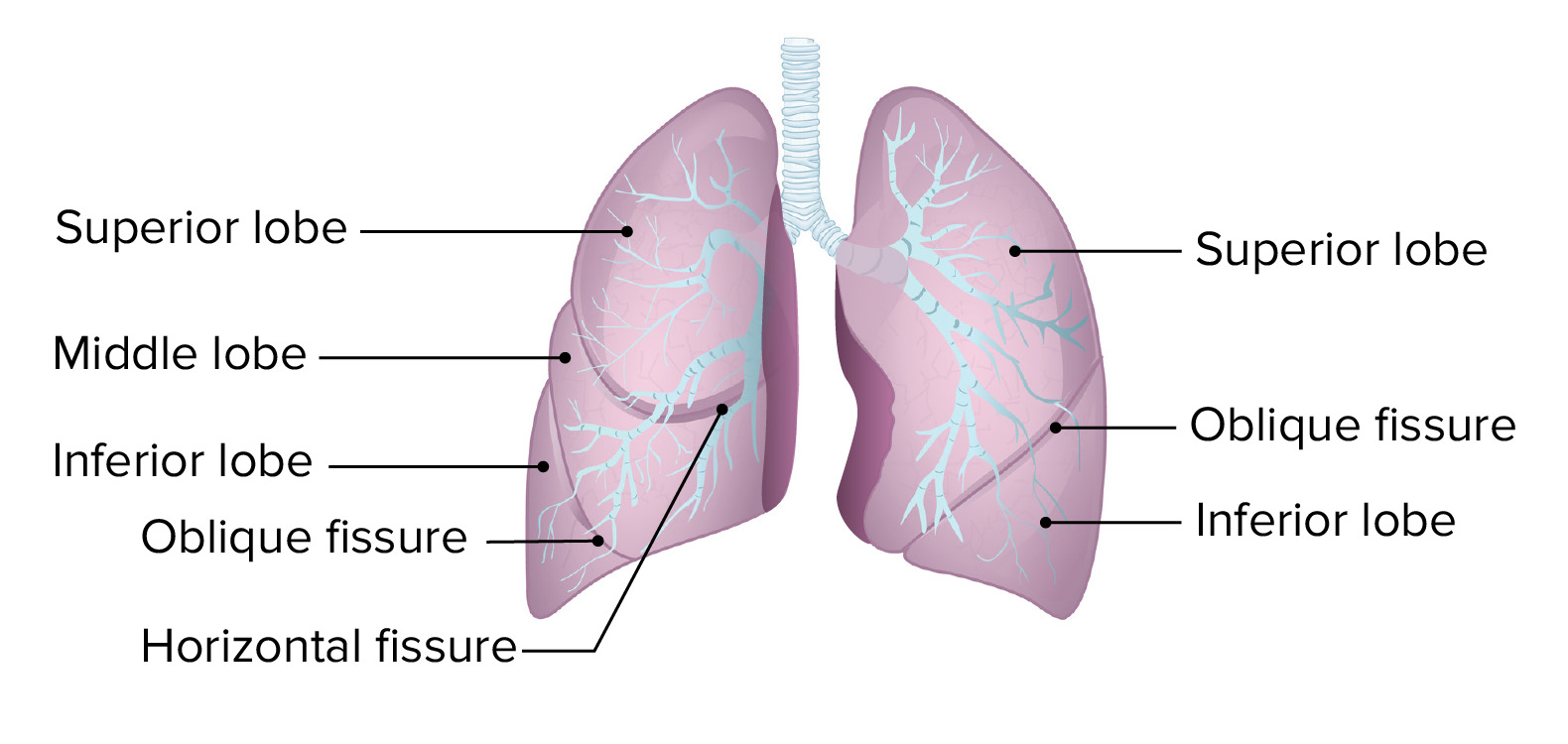
00:00 Now, we want to take a brief look at each of the mediastinal areas and the purpose of taking a look or a stop at each one is to understand the major or key viscera that are occupants of these mediastinal divisions and subdivisions. 00:19 So, the superior mediastinum will have the trachea that we see here and then running posterior to it in the superior mediastinum will be the esophagus. 00:36 In the superior and anterior mediastinum, up until puberty and a little bit beyond, your major occupant that will reside in both of these mediastina collectively will be the thymus gland. The thymus gland reaches its maximum mass at around puberty and that mass is in the neighborhood of 35 gms. Thereafter, it involutes. And so, we have a degeneration of the thymic tissue, so very little remains in an elderly person, and what does remain is scattered within adipose tissue that would be located within these mediastinal compartments. 01:25 The major function of the thymus gland is to educate: educate our T lymphocytes so that, then, they are able to recognise self-antigens. And if this educational process goes awry, that can lead to autoimmune disorders. Our middle mediastinum is depicted here. 01:55 The pericardium is shown, so that would be an occupant of the middle mediastinum. Lying deep would be the heart and the initial segments of the great vessels would also lie within the middle mediastinum. When we think about the heart within the middle mediastinum and we think about cardiac valves, the four cardiac valves, a very important part of the physical examination is to listen to the cardiac valves in your patients. There are topographic relationships that you need to bear in mind to best auscultate the cardiac valves. And so, if we take a look here, we have the aortic valve being depicted here and note the vector of blood ejection going up into the right side of the body. This is, then, the optimal location to pick up the sounds that emanate from the aortic valve and this area is in the right second intercostal space. 03:09 We also have, right in through here, the pulmonic or pulmonary semilunar valve. And again, if you follow the vector of blood flow out through this valve, you will see that the best area or the optimal area to detect closure of this valve is going to be in the second intercostal space as well, but in the left intercostal space. 03:42 If we take a look at our atrioventricular valves, which lie here and here, here’s your tricuspid. And the best location to pick up auscultation from the right atrioventricular valve is going to be in the left fourth intercostal space. And then, here’s the vector that’s associated, where we can best hear the closure of your left AV valve and that is at the level of the apex of the heart. So, that’s going to be in the left fifth intercostal space. 04:20 The posterior mediastinum. This region will house the esophagus. And so, if we take a look here, we have the esophagus extending from the superior mediastinum into the posterior mediastinum. We can also see the divisions of the trachea within the posterior mediastinum. Here, in this right view, we see the right bronchus, and on the left side, we would have the left bronchus. Some authorities, some anatomists, will assign the primary bronchi into the middle mediastinum, but others will assign these, as I am, into the posterior mediastinum. I think it’s simpler to keep that in mind because anything posterior to the posterior pericardium is, then, in the posterior mediastinum. 05:20 And now, we can do a brief quizzing session or moment with you to see if you kind of understand where we are within the thoracic cavity. And so, we could take a look here at this particular structure and note its relationship to other structures within the thoracic cavity, such as the heart. And then we have our lungs. And so, where are we within the mediastinum? Since we are posterior to the heart, this is the esophagus within the posterior mediastinum. 06:01 If we take look over here, where are we within the thoracic cavity? Left side of the image, but again, we’re viewing this as if we’re standing at the feet of a patient, looking up toward their head, so this would be the right pleural cavity. 06:28 Now, let’s summarise the key take-home messages. The thoracic cavity is divided into three major compartments. We have two pleural cavities and we have that area standing between them in the middle of the thoracic cavity called the mediastinum. 06:45 The apex of each lung extends above the clavicle to the level of C7 for the vertebral level and inferior limit of the lung will correspond to ribs 6, 8, 10. 07:00 The mediastinum is divided into superior and inferior divisions by a plane that runs from the sternal angle to an area that is located between T4 and T5. 07:14 The middle mediastinum is best defined by its major occupant, the heart and pericardium, with the other sub-divisions of the inferior mediastinum located anterior to the heart and then posterior to the heart. The points of auscultation of the cardiac valves are located in the right and left second intercostal spaces and the left fourth and left fifth intercostal spaces. The trachea is located in the superior mediastinum, as is the esophagus, and the esophagus will extend into your posterior mediastinum. 07:50 And the thymus functions to educate T lymphocytes against self-antigens and is located, at its maximum development, in the anterior and superior mediastinum. 08:06 Thank you for joining me on this lecture on an overview of the thoracic viscera.
About the Lecture
The lecture Mediastinal Areas – Lungs, mediastinum and cardiac valves by Craig Canby, PhD is from the course Thoracic Viscera with Dr. Canby.
Included Quiz Questions
A medical student places a stethoscope over the left 5th intercostal space along the midclavicular line. What cardiac valve is best auscultated in this space?
- Mitral valve
- Right AV valve
- Aortic valve
- Pulmonic valve
- Tricuspid valve
What structure is found in the superior mediastinum, posterior to the trachea?
- Esophagus
- Thymus
- Heart
- Aorta
- Bronchus
Customer reviews
4,7 of 5 stars
| 5 Stars |
|
6 |
| 4 Stars |
|
0 |
| 3 Stars |
|
1 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
Excelent teacher. Clear and precise with an according order to avoid missing anything.
For those begginer students, its a good and quick way to learn about the mediastinal areas.
Good stuff Good stuff Good stuff Good stuff Good stuff Good stuff
I want to inform in this video you made a mistake when you talk about the AV valve right and left auscultation, you said same side! left side 4th and 5th , same side and after in the summary , you said right and left 5th and 4th, you need the develop new video! Thanks