Playlist
Show Playlist
Hide Playlist
Liver Cancer: Management
-
Slides LiverCancer Surgery.pdf
-
Download Lecture Overview
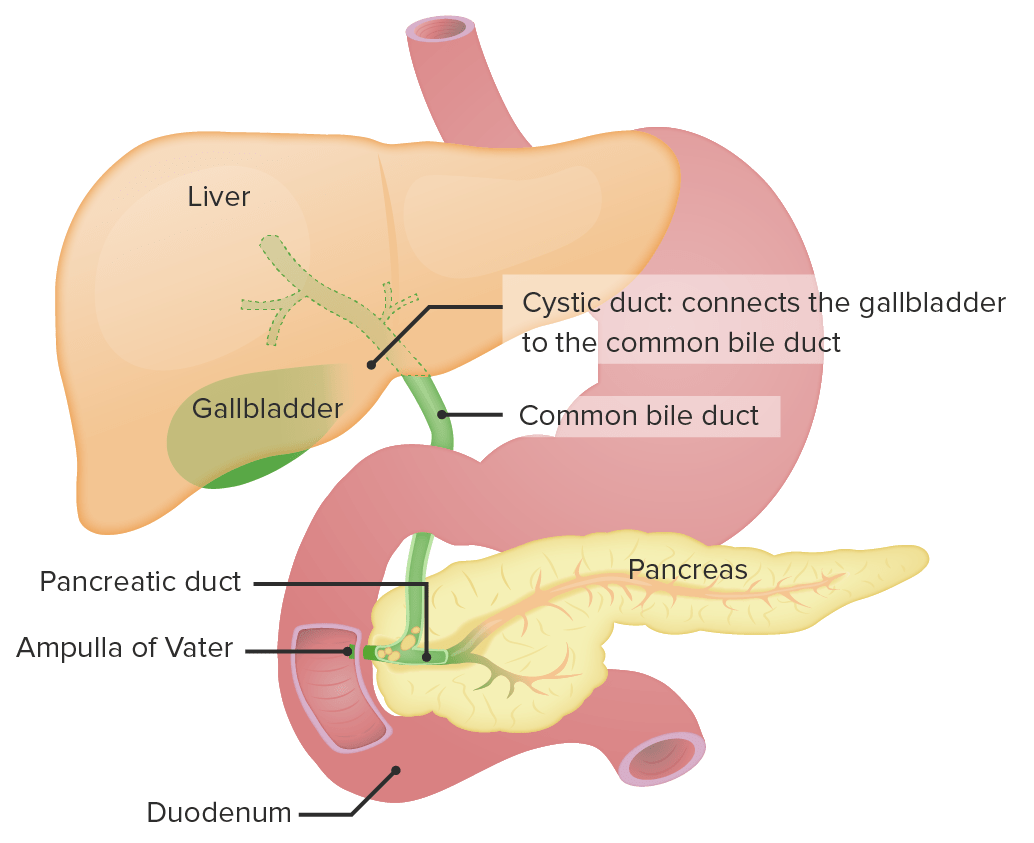
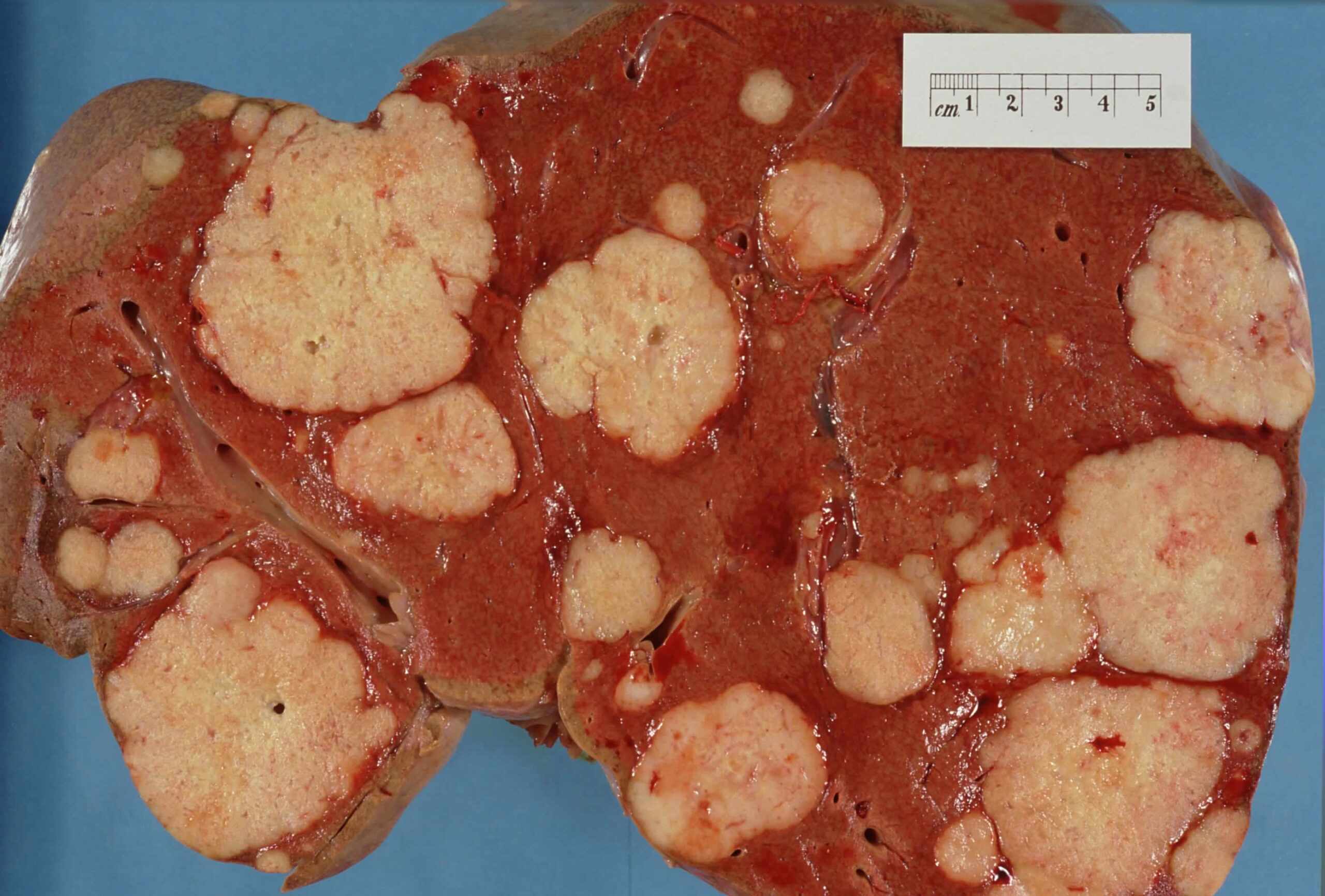
00:01 Conceptually, the way we want to think about whether or not somebody is a candidate for resection with liver cancer is to assess the tumor size, location, and metastases. This largely determines whether or not technically, the mass is resectable. It was very important also to conceptually incorporate the liver function and very importantly, the postoperative liver function. 00:27 Factors in determining resectability anatomically is the functional reserve of the liver after resection But of course, technically speaking, livers that are very close to vessels, lesions, and multiple lobes may not be amenable to resection. Liver function and particularly Child’s Pugh or MELD’s classification speak to the perioperative mortality and the liver reserve. Just because technically, you can resect a liver mass doesn’t mean that the patient can tolerate the surgery. Who’s the best candidate: small tumors, preserved liver function particularly postoperative liver function or residual liver function. 01:08 Generally, we prefer no hepatic vascular invasion and no metastases. Unfortunately, liver cancerusually presents late and few patients are candidates for surgical resection alone, whether it’s anatomic or liver function related. What if the patient is What if the patient is not a candidate for the resection? I’ll give you a second to think about this. 01:40 There are some options for patients who are not surgical candidates, RFA and TACE. 01:47 Let’s look at each individually briefly. Patients may also be candidates for transplantation. 01:55 Systemic therapies are also an option. Sorafenib can be used to inhibit angiogenesis and tumor growth, particularly if there is vascular invasion. Other immunotherapies and chemotherapeutic agents are available, depending on the clinical scenario. These may be given as monotherapy or in combination therapy. 02:07 vascular invasion. Other immunotherapies and chemotherapeutic agents are available, depending on the clinical scenario. 02:10 These may be given as monotherapy or in combination therapy. 02:17 Transarterial chemoembolization also known as TACE undergoes a very interesting concept. 02:24 As we know, the majority of hepatocellular cancer is supplied by the hepatic artery as opposed to the remainder of the liver which is the majority is supplied by the portal venous system. 02:36 This is the theory behind transarterial chemoembolization. Cut off the blood supply. 02:41 Radiofrequency ablation is also an option. In radiofrequency ablation, radiothermal energy is applied usually under ultrasound guidance intraoperatively. Radiofrequency ablation is appropriate when resection may not be possible due to the location particularly close to important vessels. 02:59 Radiofrequency ablation works best if the lesion is less than 4 cm in size. What about transplantation? Again, we’ve discussed the MELD score which was originally developed for allocation of transplantation. 03:16 Orthotopic liver transplant is appropriate for lesions less than 5 cm or cancer that involves three lesions that are smaller than 3 cm. Transplantation is discussed elsewhere. Some of the important clinical pearls to take home. Patients liver function status is an important predictor of survival. 03:39 Remember, hyponatremia or low sodium is a strong negative predictor for liver patients. 03:49 For your test, high yield information: Metastases is still the most likely lesions in the liver. 03:54 So remember, look for other lesions. This is particularly true if there are multiple lesions and there’s a potential for primary cancer such as colon cancer. Thank you very much for joining me and there’s a potential for primary cancer such as colon cancer. Thank you very much for joining me on this discussion of liver cancer.
About the Lecture
The lecture Liver Cancer: Management by Kevin Pei, MD is from the course General Surgery.
Included Quiz Questions
Which of the following patients is NOT a candidate for surgical resection of liver cancer?
- A patient with hepatocellular carcinoma and Child-Pugh class C cirrhosis.
- A patient with hepatocellular carcinoma and no metastasis.
- A patient with a small hepatocellular carcinoma.
- A patient with hepatocellular carcinoma and normal liver function tests.
- A patient with hepatocellular carcinoma and no hepatic vasculature invasion.
The hepatocellular carcinoma (HCC) cells are mostly supplied by which blood vessel?
- The hepatic artery
- The portal vein
- The cystic artery
- The hepatic vein
- The artery to the common bile duct
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |