Playlist
Show Playlist
Hide Playlist
Lichen Planus: Diagnosis and Management
-
Reference List Pathology.pdf
-
Slides Lichen Planus Diagnosis Management Dermatopathology.pdf
-
Download Lecture Overview
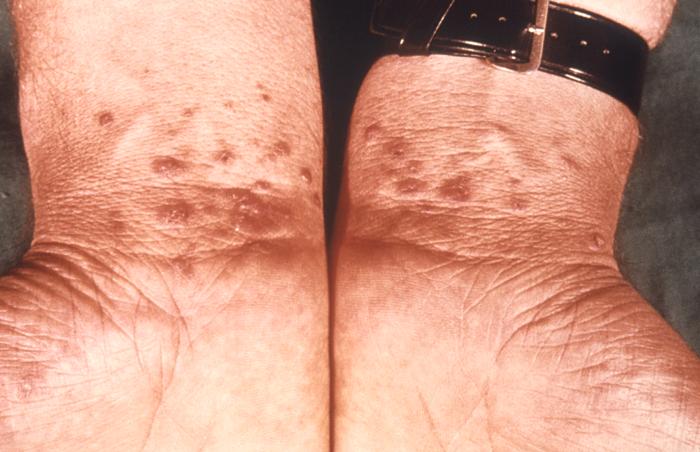
00:01 The clinical manifestations. 00:03 So again remember I said there were going to be six P's that we needed to talk about in terms of lichen planus. 00:09 So you can remember these. 00:12 They're polygonal. Why they're polygonal. 00:14 Good question. Not sure why things kind of stop and start at an edge in any inflammatory dermatosis, but there you have it. 00:22 They're purple or violaceous if you want to sound more erudite, and the purpleness actually is because of increased vascular dilation deep to it. So they can be red to purple, actually. 00:35 They're pruritic, so they are eliciting very kind of itchy, um, cytokines that drive stimulation of the of the sensory nerves in that area. 00:46 So they're often intensely pruritic. 00:48 They are planar papules. 00:50 So they're kind of flat topped and hence the name lichen planus. 00:54 And they may coalesce into larger plaques. 00:56 So those are your six P's. 00:59 There are some other manifestations. 01:01 Again, for the kind of cognoscenti in the world of dermatology, these probably won't show up on the boards. But if you become a dermatologist, you'll sound like a genius when you talk about these. 01:11 So there's Wickham striae. These are kind of lace-like white dots that are probably following lymphatics. 01:18 That's why they form lines and they can be seen on the surface of the lesions. There's also Koebner phenomenon. 01:25 And Koebner will talk about it in some other diseases later on in the dermatopathology series of talks. But a Koebner phenomenon is where we can drive disease by providing an exogenous trauma. 01:38 So this is where you develop lesions in previously healthy sites due to the trauma of scratching. 01:45 So you will develop plaques as a consequence of local trauma. 01:48 And that kind of fits in with the general, what we understand about the pathophysiology in terms of there is injury or triggering, not otherwise specified. And that can involve trauma. 02:01 Because the vessels are very leaky in this area, there is often subsequent hyperpigmentation that occurs, and this is due to the deposition of iron. 02:11 We may also see melanocyte, overproduction of melanin, and with melanin incontinence that ends up within the dermal fibroblasts population. So the the sequelae after this tends to be hyperpigmented lesions. 02:25 And these may be quite painful. 02:27 Again kind of pruritus. 02:28 Itchiness is on one end of the spectrum of pain. 02:32 It's all a stimulation of the d ermal nerves. 02:36 So the distribution can be pretty characteristic. 02:39 It's typically symmetric. 02:41 It's typically bilateral. 02:43 So that's interesting. Somehow those immune cells know to go to the same site on different extremities. 02:48 It's classically on the flexural surfaces of the extremities like the ankles and the wrists. And this is a good example here. You see on this guy's flexor surface of the wrist, most lesions will resolve by themselves within 1 to 2 years. If the patient can tolerate it. 03:03 Sometimes with therapy, as we'll talk about. 03:06 They resolve because we probably are developing a counter-regulatory regulatory T cell kind of milieu that turns off the T cells that are driving this response. 03:18 But there's a sequela and frequently the lesions are a little polygonal violaceous papules leave behind hyperpigmented macules as we talked about. 03:30 You can have genital lichen planus. 03:32 This can be incredibly itchy, incredibly painful. 03:37 It's more common in men where the lesions are typically on the glans penis. 03:41 But in women it can affect the vulva and the vagina. 03:44 So it can be even in sites that are not typically you think of as skin. 03:49 It's associated, as I said, with pruritus in both men and women, dyspareunia, particularly in women, so painful intercourse, there are erosive lesions and you can have urethral stenosis as a result of the inflammation and scarring associated with this. 04:07 And with chronic inflammation, and then chronic regeneration of the epithelium, these may become a nidus for the development of squamous cell carcinoma if they do not resolve effectively. 04:21 Other forms of lichen planus can affect any stratified squamous epithelium. 04:25 So we see it in the esophagus. 04:27 And we also see it in the otic canal. So in the ear. And so be aware that it can be in other places as well. The diagnosis is a combination of yeah you see it. You recognize it. 04:43 It's there. You know there the six PS and you go and I think that's very likely. And then you would want to do, in this case a punch biopsy to confirm that that is your diagnosis. 04:54 The features are somewhat nonspecific. 04:57 But to the trained dermatopathologist they are reasonably characteristic for the entity. 05:03 So from top to bottom in the skin we're going to see a thickened stratum corneum. This is a dysregulated kind of epithelial maturation. We're also going to see parakeratosis or nuclei within the cells of the stratum corneum which you normally see. 05:21 You're going to see a thickened granular layer or stratum granulosum. 05:26 And again this has to do with the defective or abnormal maturation of the keratinocytes. We're going to see a thickened stratum spinosum layer so otherwise known as acanthosis. 05:39 Some of the features that make it a little bit more specific for the trained dermatopathologist, not you guys, you don't have to worry about this, I do, but you don't, is that you're going to see what's called sawtoothing or kind of very irregular narrowing of the dermal epidermal interface. 05:55 Usually that's kind of rounded and little papillae. 05:57 Here it's changed probably as a combination of inflammation, but also of local fibrosis around that dermal epidermal junction. 06:05 And then we're going to see profound dermal epidermal inflammation with the secondary effects on vascular dilation with edema because of due to vascular permeability. 06:18 The other findings. So we've already talked about many of these. The hyperkeratosis of the stratum corneum with parakeratosis. 06:25 There are civatte bodies circled on your image there. 06:29 These are little anucleate. 06:31 These are apoptotic keratinocytes. 06:34 And they tend to be more common in lichen planus than other entities. 06:39 But it's a little bit nonspecific. 06:41 We will see kind of wedge-shaped hyper granulosus that is to say hyperplasia of the stratum granulosum. 06:48 That's also somewhat a, you know, nonspecific but is helpful. 06:53 I've already talked about the reedy ridges being sawtooth, and the basal layer of the epidermis, along with the Civatte bodies are going to be there's going to be some spongiosis that's the vacuolar kind of alteration. 07:05 And then a band-like a very profound lymphocytic infiltrate at the dermal epidermal junction. How do we manage this? Well, I already said that it's going to go away pretty much on its own within 1 to 2 years. And that's because of the development of T regulatory cells. But in the meantime, you want to help your patient because they are itchy. So you will give them, say antihistamines. 07:27 Emollients seem to help. 07:29 Um, for first-line pharmacologic therapy. 07:32 If we're going to go to bigger guns, you want to be adding anti-inflammatory agents. So topical corticosteroids. 07:39 For oral lesions or those around the vagina or on the penis, you may not want to use topical corticosteroids because of the risk of cutaneous atrophy. So you may go to other therapies like systemic corticosteroids, topical calcineurin inhibitors like cyclosporin. You may use PUVA. 08:00 So you may use phototherapy that will be effective in killing T cells and changing the maturation of the stratum spinosum. And oral retinoids that also have effects both of those effects. 08:17 So lichen planus tree moss that's flat. 08:22 Hopefully you've got some interesting information. 08:24 You remember your six P's and you'll be able to make the diagnosis the next time you see it.
About the Lecture
The lecture Lichen Planus: Diagnosis and Management by Richard Mitchell, MD, PhD is from the course Inflammatory Lesions of the Skin.
Included Quiz Questions
Which histological feature is characteristically seen at the dermal-epidermal junction in lichen planus?
- Sawtooth rete ridges
- Round papillae with sparse inflammation
- Thin epidermis with minimal inflammation
- Straight rete ridges with neutrophilic infiltrate
- Irregular papillae without inflammation
What are Civatte bodies in lichen planus?
- Apoptotic keratinocytes
- Melanin deposits
- Bacterial colonies
- Viral inclusions
- Fungal elements
What is the hallmark finding at the dermal-epidermal junction in lichen planus?
- Band-like lymphocytic infiltrates
- Diffuse neutrophilic infiltrates
- Scattered plasma cell infiltrates
- Perivascular eosinophilic infiltrates
- Granulomatous inflammation
What is the first-line treatment for localized lichen planus on the trunk?
- High-potency topical corticosteroids
- Systemic corticosteroids
- Oral antihistamines
- Topical emollients
- Topical calcineurin inhibitors
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |