Playlist
Show Playlist
Hide Playlist
Large Airways Obstruction: Causes
-
Slides 05 MajorAirwaysObstructionBronchiectasis RespiratoryAdvanced.pdf
-
Download Lecture Overview
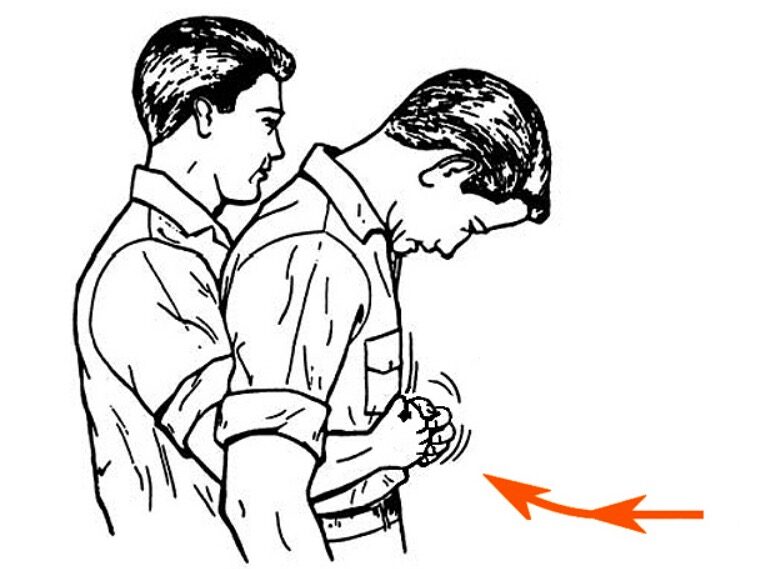
00:01 Previously I've discussed asthma and COPD in two previous lectures on airways diseases. 00:07 This third lecture is going to cover other airways diseases, which are less common but are still significant clinical problems. We're going to talk about major airways obstruction, bronchiectasis, cystic fibrosis, which is a genetic disease that is a cause of bronchiectasis and hemoptysis. Diseases that we're going to discuss today are those that cause large airways obstruction, and this is physical obstruction of the central airways, which I mean, the larynx, the trachea or the major bronchi. Now clearly, this is an important area for conducting air to the lungs, and if you block the trachea, then you're gonna get less air ventilating the lungs, and that is the major significant problem with these and that's that they are potentially life-threatening disorders. In addition, they are easily misdiagnosed as much more common diseases such as asthma or COPD. When you have common diseases like those two causes of airways diseases, asthma and COPD, it's quite easy to think that anybody presenting with airways obstruction, cough could have asthma or COPD and forget about things like larger airways obstruction which will be present in a very small minority of patients presenting with those symptoms. So you do need a high index of suspicion to make sure that you don't miss these diseases. 01:25 So what are the causes and how do people present who have large airways obstruction? Well, this depends to a certain degree on the speed of presentation. So somebody suddenly presents with airways obstruction, very acute breathlessness and stridor inspiratory wheeze then you need to think about aspiration of a foreign body or a large object lodging in the tracheal and major bronchus that's been dislodged or has been aspirated by the patient. In addition, it could be a mucous plug, but they would only normally clog off a large airway if there's a pre-existing stricture of some description. So it's basically a mucous plug on top of an another cause of airways obstruction and can present with sudden acute dyspnea and stridor. 02:15 The causes of acute airways obstruction which are not quite so sudden, but develop rapidly over hours or days include infection such as epiglottitis, and abscess of the tonsil and diphtheria and then acute deteriorations of the chronic causes and the more sub-acute causes of airways obstruction, and occasionally smoke inhalation will cause airways oedema which will cause upper airways obstruction but clearly the diagnosis of that is obvious because the patient has been recently exposed to a fire etc. So somebody presenting with the less hyperacute airways obstruction, again it's breathlessness, again it's stridor. 02:54 They also may have saliva drooling because they are unable to swallow, to get rid of their saliva and if it is an infective cause, there will be a temperature. The other causes of airways obstruction that we need to think about here are the ones which are sub-acute, the progressive, and less acute causes which build up over a period of weeks or months. 03:16 Now these tend to be diseases that get worse slowly but surely over time and hence the disease symptoms get worse over time and then they can present with acute obstruction because they finally tipped over the edge to be severe enough to cause that or a sputum plug has clogged off a partial obstruction. And the diseases we're thinking about here, the ones we really need to not miss are those of cancer. Cancer of the lung, invading the tracheal or major airways, larynx and the thyroid gland doing similar things in the upper part of the airways. Benign tracheal tumors such as carcinoids, massive mediastinal node involvement by a tumor, lymphoma or by lung cancer for example. Vocal cord paralysis, for example if you have a left recurrent laryngeal nerve palsy. Those sort of things can present, slowly progressing obstruction. Then there are a range of diseases where you may have a stenosis in the trachea or in the bronchi, but that's a fixed stenosis, it doesn't change much over time, it has occurred in the past due to some form of disease and it's now fixed at a certain level. And those situations it often happens after somebody has had a T-tube and a tracheal tube in for a long period of time. You can an inflammatory stricture that stays constant thereafter. And the same thing happens after some infections, tuberculosis being the classic example and the same thing can happen if somebody has an enlarge thyroid gland due to benign reasons such as goiter. These patients presenting with a less acute forms of airways obstruction, they're going to have dyspnoea, cough. They may cough up blood, especially if there is tumor involvement and they may get stridor but this will be intermittent, it's only present in certain positions or when the patient is slightly worse for whatever reasons. And if you have an obstruction to a major bronchus, then you can get pneumonia behind that or bronchiectasis developing and therefore they might develop symptoms as a consequence of that. If you have a tumor in the middle of the chest affecting the trachea, it could also affect other parts of the mediastinum and therefore you can get other evidence of mediastinal disease such as esophageal involvement of dyshphagia, potentially pain, potentially a neurological involvement of the phrenic nerve or paralysis of a diaphragm, etc, etc.
About the Lecture
The lecture Large Airways Obstruction: Causes by Jeremy Brown, PhD, MRCP(UK), MBBS is from the course Airway Diseases.
Included Quiz Questions
Which of the following is a more acute (rather than chronic) cause of large airway obstruction?
- Diphtheria
- Goiter
- Tracheomalacia
- Vasculitis
- Postintubation tracheal stenosis
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |