Playlist
Show Playlist
Hide Playlist
Hypersensitivity Pneumonitis (Extrinsic Allergic Alveolitis): Overview and DIagnosis
-
Slides ExtrinsicLungDiseases RespiratoryPathology.pdf
-
Reference List Pathology.pdf
-
Download Lecture Overview
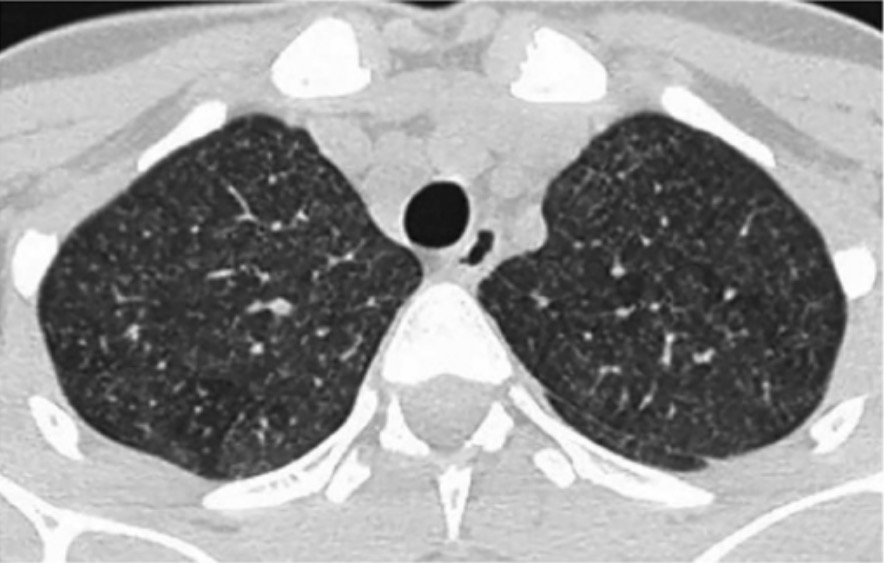
00:02 Here we have a really hot topic, called Hypersensitivity pneumonitis. Clinically called Extrinsic allergic alveolitis. Now, lets go down here for one second, make sure that you are fully aware of what’s going on. And by that I mean, we had a discussion with occupational lung diseases where we looked at pneumoconiosis and in those, or in that discussion, we looked at asbestosis, we looked at silicosis, we looked at berylliosis and we looked at coalworker pneumoconiosis, didn’t we? Leave that behind and what we have here is a patient who, once again, is'nt occupation, but in this occupation, does not develop pneumoconiosis. Does not necessarily develop all the things that we talked about earlier, but ends up developing a “allergic type of issue” and inflammatory process. Now this is a group of mixed disorder. There’s a lot of research going on in terms of what exactly is the pathogenesis. And the one thing that I wish to keep very clear here is that you do not find necessarily an abundance of eosinophilia. 01:14 Really? Yeah, you really don't. 01:17 So, at some point, when we jump into our discussion of eosinophilic pneumonia, hypersensitivity pneumonitis is really not going to be part of that. Fascinating. So you want to be really careful as to how you use the word hypersensitivity and see as to whether or not... well, your patient got exposed to something, is now having a reaction and maybe a type III/type IV hypersensitivity. 01:41 Type III, immune complex and type IV, your delayed type of hypersensitivity to environmental antigens resulting in dyspnoea, cough, chest tightness and headache. Okay. So, there will be… the cough, would be more or less your dry kind of cough, dyspnoea, interstitium is being involved. There will be chest tightness and headache. 02:02 And by environmental antigens, we’re gonna take a look at the list and this list, as we go from coast to coast in the United States, there are a lot of jobs that people have of all different types and some of these jobs may include working on the field, working with different types of growth in agriculture. So, our most researched and the most focused group here that we know much about or that we’re learning to deal, manage these patients are farmers. And that’s where your focus should be here as well. What did the farmer then get exposed to that resulted in Extrinsic allergic alveolitis? Lets continue. 02:44 Now the antibodies target specific antigens. So, here is the antigen, environmentally, a protein and even birds. Even pigeons. Be careful. If you are given a scenario where your patient is responsible for, well, we call them bird fancier, and basically that means that you have an individual that’s growing birds. Or, while they’re growing birds though, you think about maybe in their garage, a very closed environment. Oh, mighty stinky. So you walk in here, it smells bad and it’s not that you’re breathing in Cryptococcus neoformans, resulting in a type of systemic fungal pneumonia. Be careful. 03:26 It’s a fact that, well, if you’re growing these birds on a regular basis that you might then be exposed to the proteins in the wings or the proteins from the excreta. The proteins, resulting in hypersensitivity pneumonitis. 03:40 Antibodies target specific antigens and approximately two-thirds of your patients of hypersensitivity pneumonitis develop a non-caseating granuloma. Yet another example of non-caseating. You know about sarcoidosis, you know about Crohn’s disease, Berylliosis to a certain extent and then here, hypersensitivity. This is an interstitial pneumonitis. So therefore what do you think you might have? Increased fibrosis. And as soon as you have fibrosis that’s taking place around the bronchioles, what may this result in? Once again, bronchiolitis obliterans. You see as to how, that is just a very generic term or description, but it tells you a lot as to what’s actually taking place, what exactly is causing the fibrosis in your patient to then obliterate the bronchioles. 04:29 Okay. As I told you earlier, it will be the farmer that you’re going to be paying attention to. Is that the only patient? No, but the farmer is going to appear many times on this table because that’s the focus group for the most part, in which a patient then comes in with maybe fever, headache and chest tightness and coughing. Okay. 04:48 So, if it’s the “farmer’s lung”, exposure to what? Mouldy hay. And imagine, there is rain that has been, you know, going on for a week and even in the next week, if it’s been sunny, you can only imagine that the hay and as to how it is then mouldy. And then now the patient has been exposed to Thermophilic actinomycetes. How does it behave? Behaves as a hypersensitivity pneumonitis. This isn’t actinomycosis where you end up having those yellow-gold and sulphur granules around the teeth and then may even have a cervicofacial type of fissure. That’s not what this is. Be careful. Even though it seems like it’s the same bacteria, it’s the particles of proteins. 05:34 What else? We talked about the bird fancier. These individuals are growing different types of birds, maybe perhaps even pigeons. But, look at the antigen that you’ve been exposed to. Proteins and organic dust from the bird feathers or excreta, not to be confused with Cryptococcus neoformans, which will then be your, well, your caseating type of granuloma, the type of pneumonia that you’re probably very, very familiar with. Be careful. 06:02 Next. Byssinosis. So this is the textile industry. So throughout the entire week, the patient now has been working with cotton, linen, hemp fibres in which throughout the entire week, he or she is breathing this in and resulting in that chest tightness, headache, not feeling that great. Comes home on a Friday and tells your, you know, tells your loved one, “Listen, I am not feeling that great, I don’t feel like going out. Can we just stay at home and do whatever?” And then, you see what I’m saying? Hypersensitivity pneumonitis. 06:33 We have others, silo filler’s. You’re working in a silo, filling stuff up. What are you exposed to here in a silo? Fermentation, nitrogen dioxide. How is your patient going to present again? Cough. Number 2, it will be dry in nature, interstitium. Number 2, chest tightness and the most important thing here is the history of your patient been exposed to whatever antigen that was. 07:00 Then guess what your next step in management is in all of these cases? Remove the patient from the environment to see as to whether or not the patient is going to be relieved. That’s your next step of management. We’ll talk more about that coming up. 07:14 Nylon flocker’s. So, those are that are working with nylon. Proteins from nylon is a big deal. 07:20 And say that you’re working with sugar cane. This is bagassosis. So, bagassosis would be, if you’re working with sugar cane, then here, once again, been exposed to Thermophilic actinomyces. 07:31 Now in general, you can see, this is quite non-specific and vague in terms of symptoms. 07:37 It’s not thoroughly understood, but it’s understood just enough where we know that it occurs and the list, ladies and gentlemen, clinically, I have given you the most common type of exposures, but it goes by hundreds. Really. I mean, think about all the different things that you might be exposed to. 07:53 Now definition. Here, it is important that you pay attention. Extrinsic allergic alveolitis. 08:00 How would you diagnose your patient with hypersensitivity pneumonitis? Now, we’ll walk through the criteria. So, what we’ll do is, I’m going to give you the criteria listed below and then if it’s criteria 1, 2 and 3 that are met and that’s the one that I want you to focus upon, then your patient has Hypersensitivity pneumonitis. The others, well, there’s a combination of others and I’m just gonna… There it is, take a look at it, but you pay attention to 1, 2 and 3. 08:26 Number 1, I told you, history. As the patient been exposed to whatever antigen in that environment, a farmer, whether from a silo, was it from birds, so forth. 08:38 Compatible clinical, radiographic and physiologic findings, what does that mean? On chest X-ray, if it’s the interstitium that’s been affected, please understand that it will be reticular pattern. Respiratory, well, your constitutional symptoms there would be your fever, the cough, the chest tightness that we talked about, the crackles, worsening after several hours after exposure. That is criteria number 1. 09:03 Criteria number 2. It is not the eosinophilia that you’re looking for. Is that clear? So even though we call this hypersensitivity and we even call this allergic, it doesn’t necessarily mean that you have increased eosinophils. So what you’re looking for in a BAL, stands for bronchoalveolar lavage. In the lavage, you end up finding lymphocytes of a low CD4 to CD8 ratio. So, who are you… Which one of these lymphocytes do you have more of? Good. It’s a CD8. Low CD4 to CD8 ratio. Criteria number 2. Important. 09:41 Then criteria number 3. Positive inhalation challenge test. Sure, meaning to say that, now, the patient has been exposed to that particular antigen and i’ll show you a graph upcoming where it will show you that the symptoms of your patient is going to worsen. 09:58 If criteria 1, 2 and 3 have been met, then your patient has hypersensitivity pneumonitis. 10:05 Your first clue that your patient even has such a pathogenesis or clinical picture is, number 1, exposure to that antigen, and number 2, the fever, the dyspnoea, the respiratory issues and so forth. 10:20 Lets take a look at the graph here and dissect it with hypersensitivity. And what this is, and what it’s going to show you is the fact that you’ll notice that upon exposure, either to the environment in the natural habitat of your patient or, number two, you’re doing an antigen type of test that hours later, that you’re going to find worsening of the patient’s condition. On the X-axis represents the time in hours and the Y-axis represents the percentage change from normal to deteriorating type of condition. The blue curve represents the environmental challenge and the antigen is in the red curve. 10:59 Okay. So now, I told you, the first criteria is to see as to whether or not the patient… upon removing the patient from their environment, are they going to feel better? Well, if from the history you keep getting that the patient says, “Hey, doc, every time I walk in that silo, ooh, hours later, I don’t feel very well, and then I leave and then I go, you know, take a hot bath or whatever.” And imagine that, actually that hot bath itself could be, you know, another form of hypersensitivity, but anyhow. They are not gonna give you two scenarios at the same time. “I feel better when I remove myself from the environment.” You get that type of history every single time, that’s your environmental challenge. 11:39 Antigenic challenge is the fact that you are now, you have to be very careful here though. 11:43 Because if you are going to provide the antigen which is then going to make the patient feel not very good, do you understand to as to how that’s, you know what I mean? Like, exercise caution, make sure that you’re always properly equipped with any type of supportive therapy, just in case, the worst case scenario. But this is just to illustrate the importance of hypersensitivity pneumonitis and its importance in terms of exposure. 12:09 Once again, would you tell me as to what that second criteria was? Good. It was low a CD4 to CD8 ratio when dealing with the bronchoalveolar lavage.
About the Lecture
The lecture Hypersensitivity Pneumonitis (Extrinsic Allergic Alveolitis): Overview and DIagnosis by Carlo Raj, MD is from the course Disorders of the Pulmonary Circulation and the Respiratory Regulation: Basic Principles with Carlo Raj.
Included Quiz Questions
Which of the following statements regarding extrinsic allergic alveolitis is correct?
- Mixed type III/IV hypersensitivity reaction and a majority progressing to non-caseating granuloma.
- Mixed type II/IV hypersensitivity reaction and a majority progressing to caseating granuloma.
- Mixed type I/II hypersensitivity reaction and a majority progressing to caseating granuloma.
- Mixed type III/IV hypersensitivity reaction and a majority progressing to caseating granuloma.
- Mixed type III/IV hypersensitivity reaction and a majority progressing to suppurative granuloma.
Which of the following represents the correct components involved in the immunological response that occurs in hypersensitivity pneumonitis?
- Immune complexes and sensitized T cells
- Immune complexes and mast cells
- Immune complexes and sensitized eosinophils
- Immune complexes and sensitized B cells
- Immune complexes and IgG antibodies
What is the etiology of bronchiolitis obliterans in extrinsic allergic alveolitis?
- Fibrosis resulting from interstitial pneumonitis
- Necrosis resulting from interstitial pneumonitis
- Fibrosis resulting from interstitial pneumonia
- Non-caseating granuloma from interstitial pneumonitis
- Type II hypersensitivity resulting from interstitial pneumonitis
Which of the following is the inciting antigen in farmer's lung disease?
- Thermophilic actinomycetes
- Cryptococcus neoformans
- Nitrogen dioxide gas
- Ancylostoma duodenale
- Acanthamoeba
What is the most appropriate step in the management of a patient with suspected hypersensitivity pneumonitis?
- Remove the offending antigen.
- Bronchoalveolar lavage
- Pulmonary function tests
- Corticosteroids
- Chest x-ray
Exposure to proteins and dust from bird feathers and excreta would most likely result in which of the following conditions?
- Bird fancier's lung
- Cryptococcosis
- Chlamydophila pneumoniae
- Byssinosis
- Bagassosis
Which of the following is a characteristic finding in the bronchoalveolar lavage of a patient with extrinsic allergic alveolitis?
- Low CD4:CD8 ratio
- Low CD8 levels
- High CD4 levels
- High CD4:CD8 ratio
- High eosinophil levels
Which of the following is incorrectly paired?
- Farmer’s lung – Bird drops
- Byssinosis – Hemp
- Nylon flocker's lung – Nylon
- Bagassosis – Moldy sugar cane
- Silo filler's lung – Nitrogen dioxide
Which of the following is false regarding hypersensitivity pneumonitis?
- Low CD8:CD4 ratio
- Low CD4:CD8 ratio
- High CD8:CD4 ratio
- Positive inhalation challenge test
- Noncaseating granuloma formation
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |