Playlist
Show Playlist
Hide Playlist
Hepatitis C Infection with Case
-
Slides Gastroenterology 11 Liver Pt1 Hepatitis.pdf
-
Reference List Gastroenterology.pdf
-
Download Lecture Overview
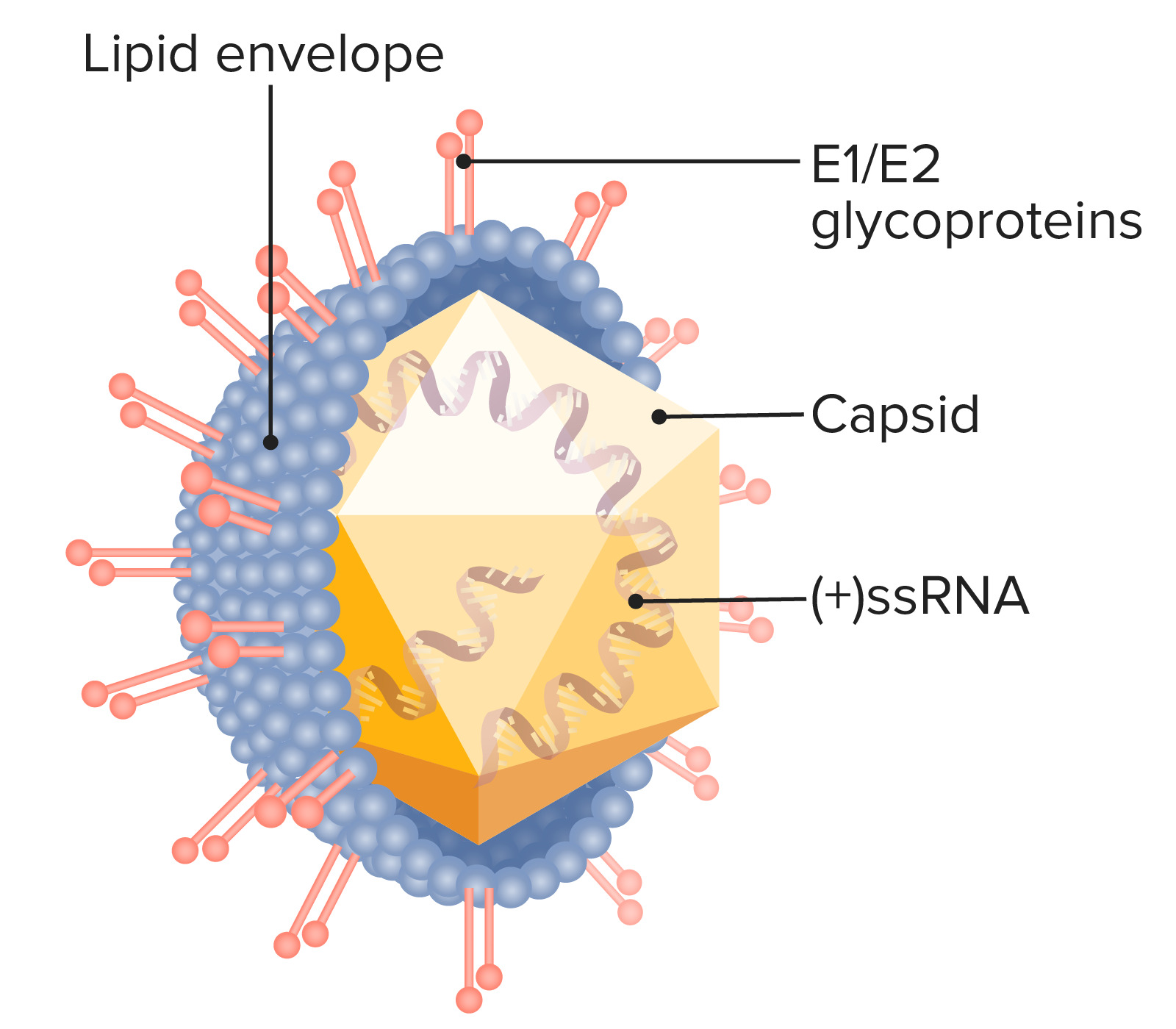
00:01 We'll move on to our next case. 00:04 A 37-year-old woman is seen in clinic after a recent diagnosis of hepatitis C infection. 00:10 She has a history of injection drug use 15 years ago. 00:13 She feels well and takes no medications. 00:16 Vitals and physical exam are normal. 00:19 Lab studies show the following: Her hepatitis C antibody is positive. 00:23 Her RNA, PCR is also positive with 1.2 million copies. 00:29 She has a positive hepatitis B surface antibody. 00:33 And her surface antigen and core antibody are both negative. 00:37 What is the best next step in management? So let's go through some key features here. 00:43 She has a known history of hepatitis C infection from her exposure to intravenous drug use. 00:50 She has a positive hepatitis C antibody and a positive viral load which indicates that she has an active infection. 00:59 She also has an isolated positive hep B surface antibody. 01:04 We will talk about what that means. 01:08 So, let's talk now about hepatitis C. 01:12 Hepatitis C begins with an acute infection. 01:15 A majority of patients will then go on to develop chronic inflammation and only a small proportion of patients will develop spontaneous cure, so this is in contrast to hepatitis B where most patients develop spontaneous cure. 01:31 Then, after chronic inflammation, a small minority will then go on to develop fibrosis and eventually, cirrhosis of the liver. 01:39 After patients have developed advanced fibrosis or cirrhosis, they are then at risk for cancer of the liver or hepatocellular cancer. 01:51 So hepatitis C is the most common blood-borne infections in the United States. 01:55 All adults 18 years and older should be screened for chronic infection at least once in their lifetime. 02:01 And patients are usually asymptomatic carriers of this infection. 02:06 So the treatment for hepatitis C has actually evolved quite a bit in the last 10 years. 02:12 We now have new therapies that are over 95% effective in allowing treatment for all individuals with hepatitis C. 02:21 The goal really is to stop disease progression, prevent cirrhosis and prevent the end-stage complications that occur with cirrhosis. 02:29 The initial direct acting antiviral regimens no longer fully depend on the patient’s hepatitis C genotype. One example that you may hear about is this combination of sofosbuvir and velpatasvir. There are many others as new treatments emerge. 02:45 So now let's return to our case. 02:47 Our 37-year-old woman with a known hepatitis C infection from her IV drug use. 02:54 She has a positive antibody to hepatitis C and a positive viral load which indicate an active infection. 03:01 And we review now her positive hepatitis B surface antibody, because it's an isolation, indicates that she has had prior vaccine and immunity to hep B. 03:12 So, what is the best next step in management? We know that she has an active hepatitis C infection, so she should be treated for hepatitis C. 03:21 You can start with one of the preferred direct-acting antiviral combinations, and you’ll want to check her hepatitis C genotype (if it is easily accessible), as there may be some treatment considerations for certain genotypes. 03:35 And as part of the screening, you should obtain an abdominal ultrasound or transient elastography to screen for fibrosis.
About the Lecture
The lecture Hepatitis C Infection with Case by Kelley Chuang, MD is from the course Disorders of the Hepatobiliary Tract.
Included Quiz Questions
All adults aged 18-79 should be screened for...?
- ...hepatitis C virus
- ...hepatitis A virus
- ...hepatitis E virus
- ...HIV
- ...hepatitis D virus
Which of the following medications is used for the treatment of hepatitis C virus?
- Sofosbuvir
- Lamivudine
- Adefovir
- Tenofovir
- Entecavir
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |