Playlist
Show Playlist
Hide Playlist
Hepatic Encephalopathy with Case
-
Slides Gastroenterology 13 Liver Pt3 End Stage Liver Disease.pdf
-
Reference List Gastroenterology.pdf
-
Download Lecture Overview
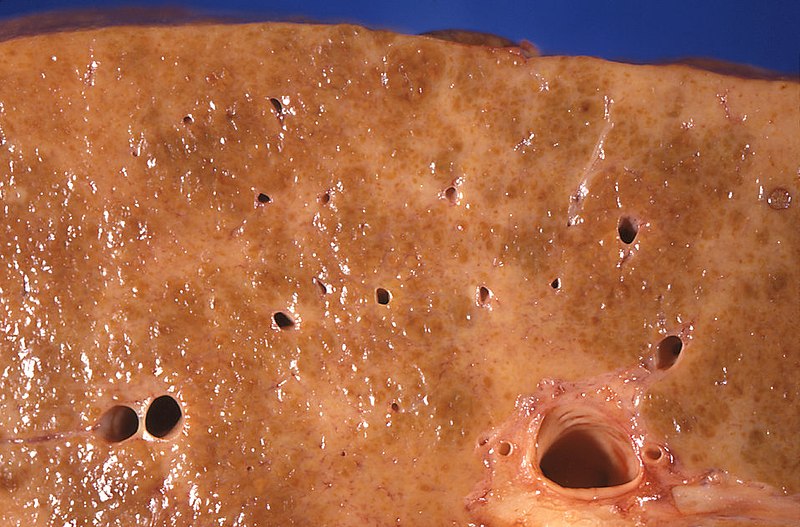
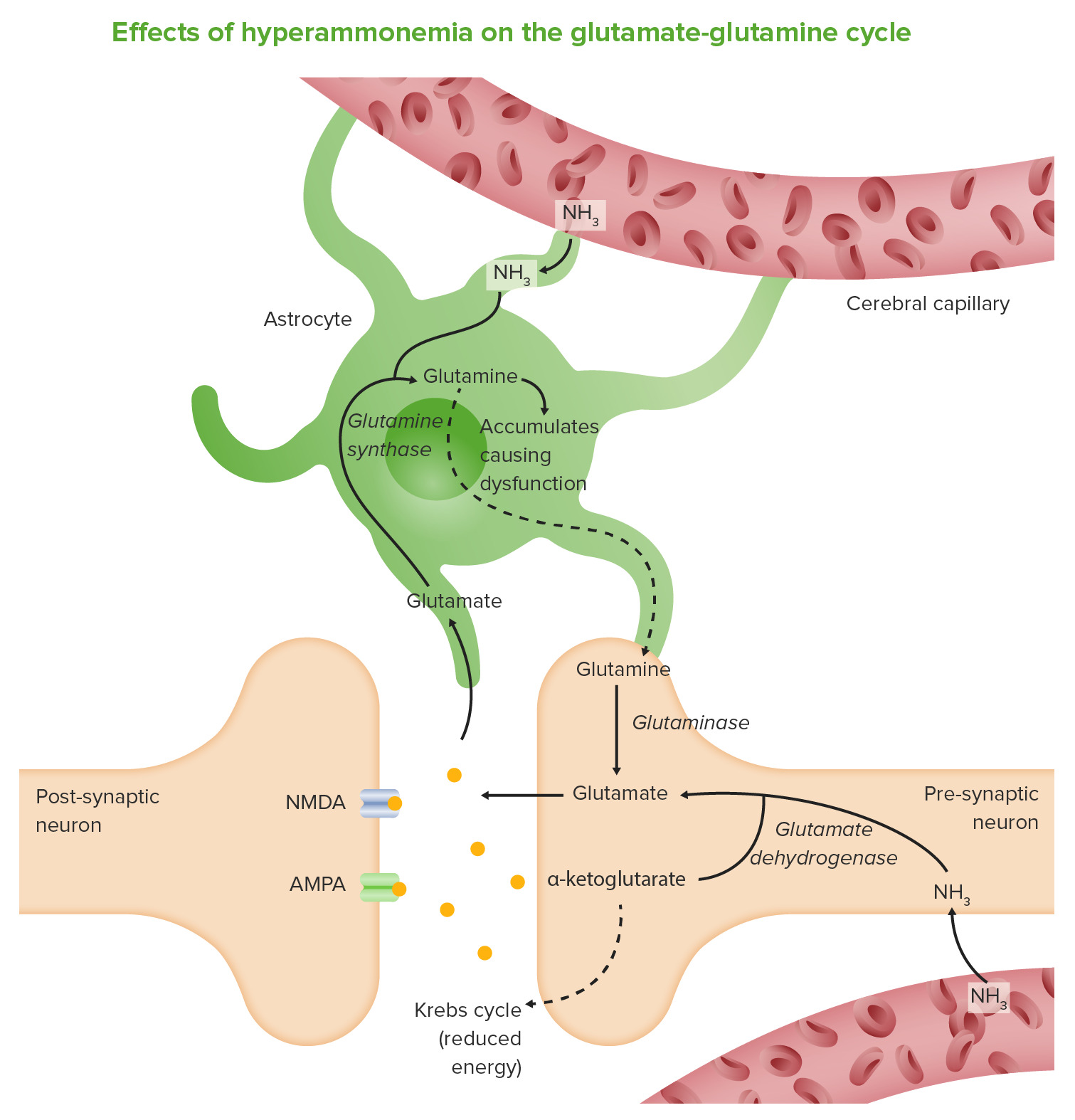
00:02 So now let's go on to our next case. 00:04 A 58-year-old man with cirrhosis from hepatitis C presents to the emergency department with new confusion for the past 3 days. 00:12 He has ascites managed with diuretics and a history of esophageal varices that were ligated one year ago. 00:20 His family notes that he has been sleepy during the day and having difficulty walking. 00:26 Vitals are within normal limits. 00:28 On physical exam, he has mild scleral icterus, a distended abdomen, flapping asterixis and slowed speech. 00:37 What is the best next step in management? So he has cirrhosis with evidence of decompensation with this presence of ascites. 00:48 He has new somnolence and gait ataxia. 00:52 And on exam, he has asterixis which is an exam finding of a lack of attention. 01:00 So let's review the topic of hepatic encephalopathy. 01:04 This is when patients develop cognitive changes or confusion due to the build up of the toxins that are normally cleared and processed by the liver. 01:11 There can be many different triggers. 01:14 So, infections are number one trigger particularly with spontaneous bacterial peritonitis or SBP, GI bleeding can also lead to an episode of hepatic encephalopathy, any issues with the kidney or electrolyte derangement can cause this, patients who have hypoxemia or hypercapnia which is the build up of carbon dioxide. 01:36 and a procedure such as a TIPS procedure which we'll discuss later and portal vein thrombosis can lead to this. 01:43 So, the symptoms can range anywhere from just mild confusion all the way to coma. 01:50 Patients also often describe a disorientation of their sleep-wake cycle. 01:56 The diagnosis is made primarily based on the history and the physical exam. 02:03 And treatment is with giving lactulose and we titrate lactulose to about 3 stools a day. 02:09 This ensures that toxins that have built up with cirrhosis are then cleared in the stool. 02:16 For cases that continue to recur, we can sometimes also give a medication called rifaxamin. 02:24 So you may have wondered why are there no labs that we can check to look for hepatic encephalopathy. 02:30 In the past we used to check ammonia levels that we thought corresponded with encephalopathy. 02:36 However, we now know that monitoring serum ammonia levels is not useful because levels can be either be high or normal in an episode of hepatic encephalopathy. 02:46 So it is simply a clinical diagnosis and you must exclude any other things that could lead to confusion. 02:55 So now let's return to our case. 02:57 Our 58-year-old man with cirrhosis who now has evidence of decompensation. 03:02 He has new somnolence and gait ataxia and this finding of asterixis which is an exam finding of inattention or confusion. 03:11 So the best next step in management is first knowing that he most likely has hepatic encephalopathy. 03:17 And then taking the next step to look for any underlying triggers for this episode. 03:22 So rule out infection, bleeding, any medication changes and then start treatment with lactulose.
About the Lecture
The lecture Hepatic Encephalopathy with Case by Kelley Chuang, MD is from the course Disorders of the Hepatobiliary Tract.
Included Quiz Questions
Which of the following is a risk factor for hepatic encephalopathy?
- GI bleeding
- Hyperkalemia
- Liver transplant
- Diarrhea
- Increased ammonia clearance
Which of the following is the treatment of choice for hepatic encephalopathy?
- Lactulose
- Diuretics
- Opiates
- NSAIDs
- Increased dietary protein intake
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |