Playlist
Show Playlist
Hide Playlist
Helicobacter Pylori
-
01-15 Helicobacter.pdf
-
Download Lecture Overview
00:01
Helicobacter pylori, a bacteria.
00:04
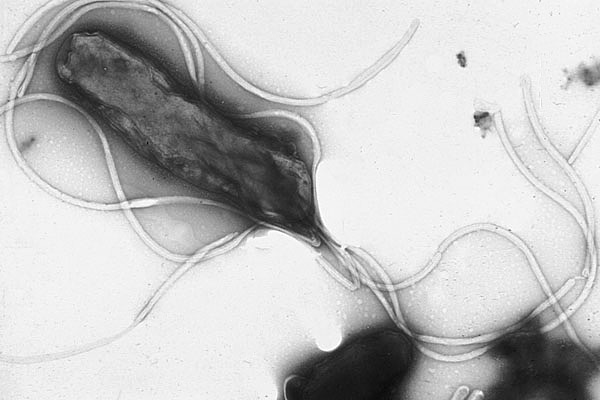
Helicobacter are gram-negative motile-rods
which have a almost novel curved or helical shape with
multiple flagella.
00:13
As we'll see in just a little bit when we discuss
pathogenesis,
this helical or screw like shape is essential to allow the
organism
to insert itself through the mucosal layer of its enteric
target and attach to underlying enterocytes.
00:25
to insert itself through the mucosal layer and attach to
underlying cells.
00:27
Helicobacter are microaerophilic and they have very complex
growth requirements,
but they are oxidase, catalase, and urease positive.
00:37
The image on the screen shows in a scanning electron
microscopy picture,
the organism itself and the surrounding flagella which are
all important
to help it enter into the junction of the enterocytes.
00:51
Now, Helicobacter pylori are ubiquitous organisms. They
indeed do exist everywhere.
00:57
And as many people have come to realize, the older one gets,
the more often one is colonized with these.
01:05
They exist by ingestion and are typically associated with
poor sanitation,
meaning water supply, poorly prepared foods, but there is
also person-to-person contact which allows them to develop.
01:20
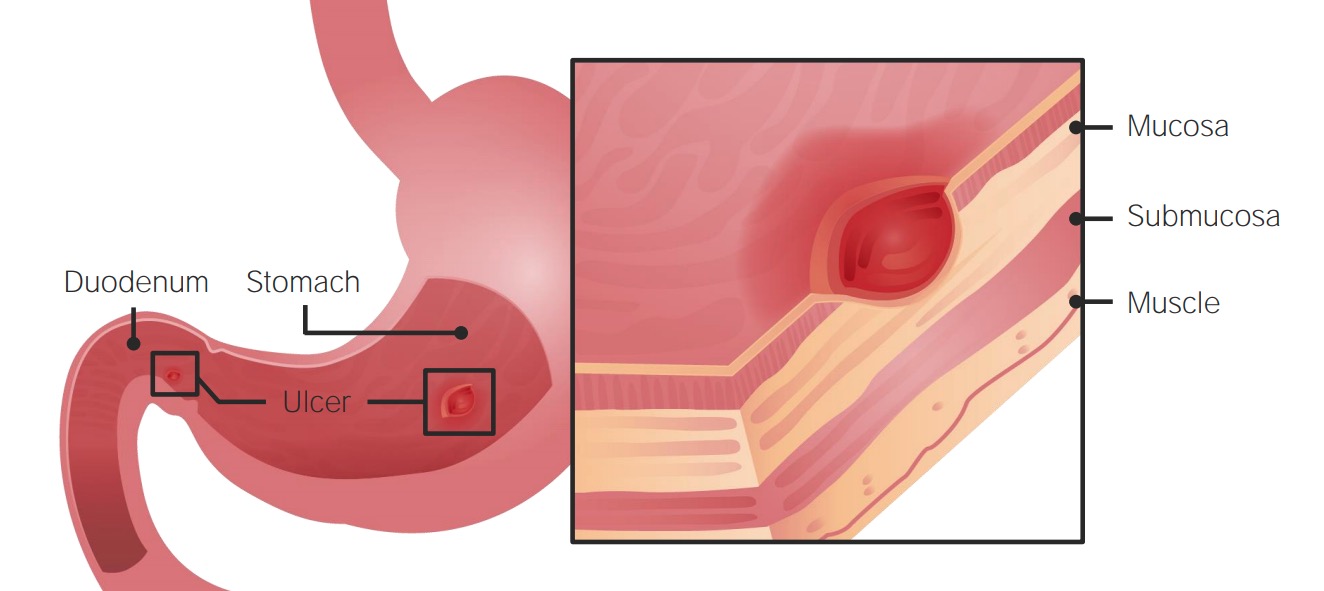
Once the initial aspiration or ingestion of the organism
occurs,
they will set up shop as you see in the images in the
stomach.
01:29
Typically, in the antrum, but also perhaps a little bit
further on closer to the duodenal junction.
01:36
And their typical target is the superficial gastric cells.
01:41
As mentioned before, the prevalence of infection in children
is quite low even though,
children do typically explore the world through their
mouths.
01:50
However, as we age and expose ourselves to a variety of poor
choices,
either for our foods or sometimes by being exposed to poor
sanitation,
we as adults become more and more colonized.
02:04
And those who are older adults and older adults in countries
where sanitation is not up to first world standards become
even more colonized.
02:14
Most of us however, 50% are colonized by the time we reach
age 65 years.
02:19
Helicobacter pylori
releases Urias as a way to neutralise
stomach acid.
02:24
This causes that outer gastric mucin gel
layer to liquefy, allowing the
bacteria to swim through and attach to the
underlying gastric alveolar cells.
02:35
So how does Helicobacter pylori produce its pathogenesis?
First and most important, is the targeting of the gut, along
with that,
Helicobacter pylori is very acid sensitive.
02:49
So in a way, it creates its own neutral or even alcohol and
pH-based environment.
02:56
It does this by production of urease -"Ase"- an enzyme which
cleaves urea into ammonia and carbon dioxide.
03:04
Those byproducts are able to neutralize the normally acidic
pH of the gut
and allows the Helicobacter to colonize that superficial
layer.
03:15
Then as mentioned, the multiple flagella and that helical or
screw like shape
allows the organism to burrow itself through the mucous
barrier
and into the top layer; the mucosal surface of the stomach.
03:31
When there, the local alkaline effect triggers release of
gastrin secretion or gastric acid
from other surrounding parts of the stomach in an attempt
to return back to the fully acidic environment.
03:47
However, this production of gastrin and an acid in a way
creates further erosion of the stomach
creating peptic ulcer disease and then putting the patient
at risk for gastric metaplasia
which increase the risk for gastric cancer.
04:04
So all these are simply due to the Helicobacter trying to
create its own perfect environment
in which to nest or burrow into the stomach.
04:12
While there however, because it is still a pathogenic
bacteria, the Helicobacter pylori
also create mucinase, again an enzyme to cleave the mucous
structures and also cytotoxins.
04:27
The development and production of the toxins
especially will then recruit inflammatory cells to the site
of the infection.
04:35
And due to almost an innocent bystander type attack,
the attempt to kill the Helicobacter pylori actually takes
out other healthy gut tissue
furthering the damage of the peptic ulcer disease.
04:49
Helicobacter pylori is very common and is in
fact the most common chronic
bacterial infection in humans.
04:56
It can be identified in the gastric biopsy
with the routine and stain as seen in the
lower left part of the slide.
05:02
But there are also special stains that
highlight the organism even better, including
the worth in stari silver stains and gums
stains as seen in the lower
left with the hand stain.
05:13
Early acute superficial gastritis is caused
by Helicobacter pylori.
05:18
You can see the marked neutrophil
infiltrates as they appear in the mucosal
neck region and lamina with the pit micro
abscess as shown by that red arrow.
05:27
On the lower right is a Werth and star
silver stain, which demonstrates
easily many of the H.
05:33
Pylori organisms colonizing the surface of
regenerative gastric epithelium.
05:38
So how do we know all this? It's actually been very
difficult to demonstrate
because Helicobacter pylori is so ubiquitous.
05:46
The link between the organisms presence in the stomach and
the development of gastritis or acid-based disease
was more definitively demonstrated by
Dr. Barry Marshall, one of two researchers;
physicians who studied the link.
06:03
Dr. Marshall, very committed to his science
and very committed to demonstrating the link drank a flask
of active Helicobacter pylori
and then charted the development in himself of peptic ulcer
disease.
06:17
When neutralizing the acid, his disease started to improve.
06:21
So as close as was possible, using himself as a test
subject, he demonstrated Koch's postulates
and definitively demonstrated the link between the organism
and gastritis.
06:32
Once that was demonstrated, it was then easier to
demonstrate the secondary risks for gastric and duodenal
ulcers.
06:39
And then the chronic atrophic gastritis further down putting
patients
at risk for known complications of gastric adenocarcinomas
and the low-grade gastric malignant lymphoma's.
06:51
So without drinking our own flask of Helicobacter pylori,
how can we demonstrate the presence of the organism present
within ourselves as a risk factor for developing peptic
ulcer disease?
One mechanism is to use the Campylobacter like organism
test; the CLO test.
07:10
Helicobacter pylori shares many cell wall components similar
to Campylobacter
and thus one can test for those components with an antibody
reaction. Also, serologic tests exists.
07:24
Remembering again, that an immune reaction does occur
to the Helicobacter pylori infection along with antibody
production.
07:32
However, the most common mechanisms to demonstrate
Helicobacter pylori
are a radiolabeled urea breath test and a stool antigen
test.
07:41
The stool antigen test; again, fluorescent antibody reaction
against antigens
expressed by the Helicobacter wall.
07:49
The radiolabeled urea breath test incorporates its presence
of urease to demonstrate positivity.
07:56
The patient drinks radiolabeled carbon-14 urea and as the
patient
undergoes normal processing by the Helicobacter and urease,
it delivers carbon dioxide and ammonia.
08:11
The ammonia stays, the carbon dioxide is exhaled and can be
measured.
08:16
So if one exhales, you know, radiolabeled carbon from carbon
dioxide,
then the patient most likely has active Helicobacter pylori
in their stomach.
08:27
So, once that has been demonstrated and the patient has
either early onset
or very active peptic ulcer disease and gastritis, what can
one do?
And there are multiple triple drug regimens that have been
recommended.
08:40
Triple drug meaning that a single agent and a single focus
of therapy is not sufficient.
08:48
One can't just neutralize the acid to improve. One also has
to treat the organism.
08:54
So the first combination which you see here; combination of
a bismuth containing product,
along with metronidazole; an antibiotic to cover anaerobes,
and either amoxicillin or tetracycline has partial success.
09:09
The similar combination of the bismuth salt with ranitidine
and clarithromycin,
also partial success. But the most definitively successful
regimen is this one here.
09:19
Combining amoxicillin with clarithromycin and a proton pump
inhibitor, something such as omeprazole.
09:27
However, this regimen needs to be conducted for more than
several weeks
along with modification of dietary regimen, rest,
relaxation, the whole 9 yards.
09:38
So Helicobacter pylori is not our friend.
09:43
Unfortunately, it's quite ubiquitous and if one has it and
unfortunately as one gets older, one likely does.
09:50
There is an increased risk for peptic ulcer disease,
gastritis and the secondary complications of malignancies.
09:58
To avoid that, eat well and eat healthy.
About the Lecture
The lecture Helicobacter Pylori by Sean Elliott, MD is from the course Bacteria.
Included Quiz Questions
Which type of special stain can be used to highlight Helicobacter pylori under a light microscope?
- Silver stain
- Hematoxylin and eosin stain
- Gram stain
- Romanowsky stain
- Periodic acid-Schiff stain
Which structure of Helicobacter pylori allows it to attach to the superficial gastric cells?
- Flagella
- Cell wall
- Cell membrane
- Cilia
- Pseudopodia
Helicobacter pylori shares common features with which bacteria?
- Campylobacter jejuni
- Salmonella typhi
- Staphylococcus aureus
- Streptococcus pyogenes
- Proteus mirabilis
Which enzyme is produced by Helicobacter pylori to neutralize the acidic environment of the stomach?
- Urease
- Hydroxylase
- Oxidase
- Catalase
- Lipase
Which of the following is/are common non-invasive test(s) used to diagnose active Helicobacter pylori infection? Select all that apply.
- Urea breath test
- Campylobacter-like organism (CLO) test
- Antinuclear antibody test
- Stool antigen test
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |