Playlist
Show Playlist
Hide Playlist
Fungal Skin Infections: Pathophysiology
-
Reference List Pathology.pdf
-
Slides Fungal Skin Infections Pathophysiology.pdf
-
Download Lecture Overview
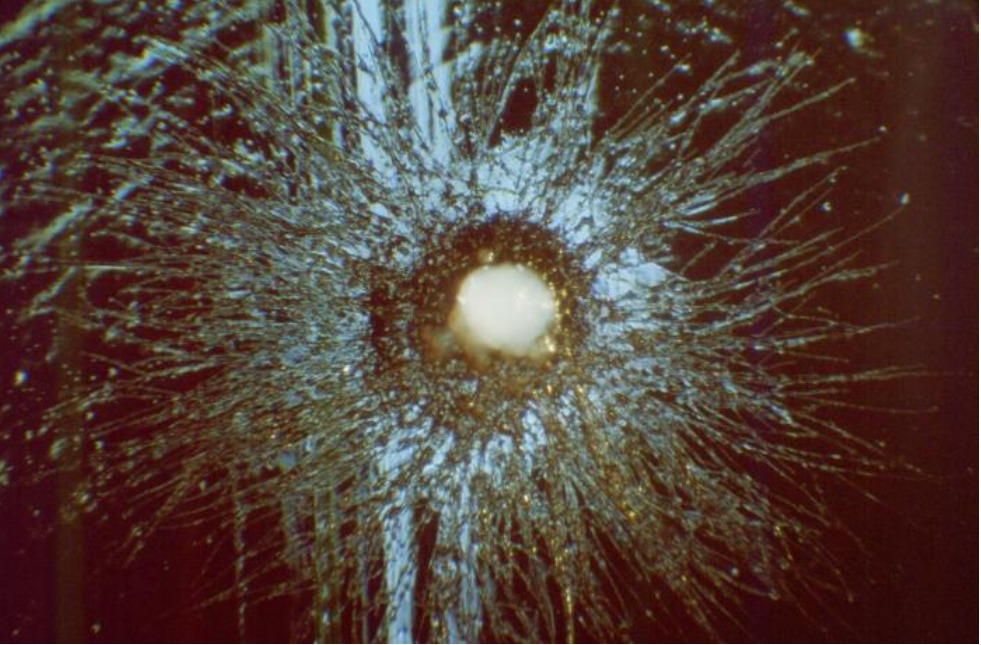
00:01 Welcome. In this talk we're going to discuss fungal infections of the skin otherwise known as dermatophytosis. So fungal infections of the skin really pretty common. 00:12 Usually, unless the host is immunocompromised they're quite superficial. 00:17 The fungus grows quite well on the stratum corneum but is not particularly invasive. 00:23 It can involve infections of the skin, hair and nail beds, as we will see. So these are all kind of generically called tinea infections. 00:34 There are 40 different species of fungus those that infect the epidermis, we will see in a moment, tend to be of one particular species, but others can be involved. 00:44 But depending on which part of the body is being invaded by the fungus, we will give the different names to it. 00:53 So you can have tinea corporis, that is a fungal infection of the body. 00:58 That's ringworm, also generically. 01:01 Tinea pedis, that's athlete's foot, and that's involving the feet. 01:06 Tinea cruris, jock itch. 01:09 Tinea faciei, smooth part of the face. 01:12 And tinea manuum, that's the hands. 01:14 Again, although we call them different, tinea s, that's just to describe where we're finding them. 01:20 They are often the same fungal organism. 01:24 In the hair, it can be called tinea capitis, involving the scalp or in the beard area, tinea barbae. In nails, it's tinea unguium. 01:34 And another name that we use for that is onychomycosis, kind of ugly looking nails. 01:41 Again can be all the same fungus, even though we're giving it different names. 01:45 So the epidemiology of this, it's exceptionally common. 01:50 Involvement of the skin or various areas around the body vary somewhat in terms of gender, in terms of age. 01:59 And you can see that here. 02:01 We'll go through this kind of briefly. 02:03 So ringworm, tinea corporis, involving the trunk of the body. 02:07 Males more common than females. 02:09 Half of the time it'll be in children less than 15 years of age. 02:13 Tinea pedis: 3 to 15% of the population. 02:16 So really common, typically in older men. 02:20 Tinea cruris, that's jock itch 20 to 25% of the population. 02:25 And if it's more hot or humid, it tends to be more common. 02:29 And adolescent males who aren't known for their hygiene in the first place are more commonly going to be victims of tinea cruris. 02:37 Tinea capitis, very common infection, mostly in pre-pubertal children and onychomycosis. That's the tinea involving the nails is going to be typically in older individuals. So the pathogenesis of this overall, as I say it's the same fungus in different areas for the most part. 03:00 So Trichophyton rubrum is the most common cause, and we're seeing examples of it on culture plates. 03:07 And then what it looks like on KOH preps that we're going to discuss in a moment. 03:11 KOH is potassium hydroxide. 03:13 Other fungal species that can be involved Trichophyton tonsurans, Microsporum canis, and Trichophyton interdigital. 03:22 So again there are over 40 species but these are the primary actors. 03:27 When we find them on the body and there are various locations, the pathophysiology. So the fungus colonizes keratinized human tissues. 03:36 That's hair, that's skin, that's nails. 03:39 They protest. They they have in them proteases that allow for the penetration of the stratum corneum. And they can metabolize keratin as their fuel source. 03:49 So that's what they're living off. 03:51 As I said at the very beginning, they're typically quite superficial unless the patient is immunocompromised. 03:58 And we really only see the epidermis and or nail beds and or hair superficially involved. 04:05 Interestingly, most of the fungi do not survive at core body temperature of 37 degrees. They just don't like that. 04:12 The clinical presentation is again kind of recognizing it when you see it. 04:18 They are typically pruritic erythematous scaly patches or plaques. 04:23 They the active advancing border may be raised. 04:28 They spread centrifugally, which means that they start typically on the trunk and then can go out to the extremities. 04:34 And as they move, as the immune system catches up with them in one location and they move on to the next, you will have central clearing of the lesions as they occur. 04:45 In hair bearing areas, the fungal and fungal metabolites can actually drive the hair follicles into a, into catagen and then telogen. 04:58 So you may have alopecia in those areas. 05:01 Once the fungal infection is cleared, the hair will come back. 05:05 You can also get very deformed and dystrophic nails when you have it involving the nail beds. And those are those big, ugly great toenails that we showed earlier. 05:17 Diagnosis. It's not that hard once you've been kind of seen what they are and what they look like. It's a clinical diagnosis, but if you need to confirm that the easiest one is on the site, a potassium hydroxide preparation, basically you scrape the skin, put it on a slide, add potassium hydroxide, which degrades all of the keratin, and then you see the fungus left behind. 05:42 And that's something you can do in your office, in the emergency room, at home, in your dorm room, if you're so inclined. 05:50 Histopathologic examination will show fungus by a periodic acid-schiff or PAS stain. 05:57 You can do fungal cultures, but that's not usually indicated because we know what the what the organisms are and we know how to treat them more broadly. 06:06 Almost never would you do PCR unless you have some sort of deep seated infection, and it really becomes important to understand what's driving that. 06:14 The management overall, well, the skin lesions and non-hair bearing areas typically respond to antifungal agents, topical antifungals. So a little bit of itraconazole or terbinafine will be more than enough. And you can use those as topical agents. 06:37 For refractory disease where that didn't seem to work, go to oral variants on that. 06:42 And hair-bearing areas, griseofulvin or terbinafine are used orally and for onychomycosis for that severe involvement of the nail bed, you may require oral terbinafine or itraconazole. 06:56 And with that, we've discussed fungus, and hopefully, you've not been too grossed out by what we had.
About the Lecture
The lecture Fungal Skin Infections: Pathophysiology by Richard Mitchell, MD, PhD is from the course Infection Conditions of the Skin.
Included Quiz Questions
Which fungal species is the most common cause of dermatophytosis?
- Trichophyton rubrum
- Microsporum canis
- Trichophyton tonsurans
- Trichophyton interdigitale
- Epidermophyton floccosum
Why do most dermatophytes remain superficial in the skin?
- They cannot survive at core body temperature (37°C)
- They lack invasive enzymes
- They require UV exposure
- They need atmospheric oxygen
- They cannot penetrate blood vessels
Which type of tinea infection most commonly affects pre-pubertal children?
- Tinea capitis
- Tinea pedis
- Tinea cruris
- Tinea corporis
- Tinea unguium
What is the quickest and most practical method to confirm a dermatophyte infection in a clinical setting?
- KOH preparation
- Fungal culture
- PCR testing
- Skin biopsy
- Wood's lamp examination
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |