Playlist
Show Playlist
Hide Playlist
Factors Affecting Drug Metabolism – Biotransformation | Pharmacokinetics (PK)
-
Slides Factors Affecting Drug Metabolism Biotransformation PK.pdf
-
Reference List Pharmacology.pdf
-
Download Lecture Overview
00:00 What are the factors that affect drug metabolism? Well, you have genetic differences of cytochrome P450, you can have inhibition of cytochrome P450, you can have inhibition of cytochrome P450, you can have induction, you can inhibit P-glycoprotein, and you can alter blood flow. So all of these things are going to affect the way that we metabolize our drugs. Now, racial factors affect cytochrome P450 activation. So for example, let's talk about 2D6. So, 2D6 is one of the iso-enzymes, it has 4 different phenotypes. There are the poor metabolizers. These guys are men and women who have 2 inactive alleles. 00:43 Then you have the intermediate metabolizers. These are heterozygotes. They inherited 1 active allele from their mother and perhaps an inactive allele from their father. 00:55 So they have 1 active, 1 inactive allele so they're heterozygotes. They have a moderate amount of activity. You have extensive metabolizers. So they inherited from each parent an active allele. So these are very extensive metabolizers, they will bring down the drug level and convert it to the daughter drug very quickly. There's a 4th category. 01:17 These are the ultra rapid metabolizers. Some patients will have multiple copies of their genes that will code for very active cytochrome systems. Here is an example of what we're talking about. So this is a drug called nortriptyline. It's an antidepressant. 01:35 And let's take a look at a person who has zero functional 2D6 genes. There is the concentration curve. Okay? Now let's look at a concentration curve when a person has 1 functional gene or 2 functional genes or 3 functional genes or in fact 13 functional genes. 01:57 So the more functional genes for that 2D6 you have, the lower your drug level and the less active that drug is going to be in that body and the more drug you need to prescribe for that person or perhaps just use a different drug. Cytochrome is like a bridge and imagine you're driving in a car. As long as the bridge is empty, you can drive a car very quick. Two drugs may compete for that same pathway. So if you have too many cars trying to cross the bridge, it's going to take a long time getting across that bridge. 02:31 One drug may actually inhibit the metabolism of another. So if you have a person who is driving really slow in a car, then even though there is not too many cars around, that one person can slow down an entire chain of cars. So that's what an inhibitor does on the cytochrome system. Now, one drug may induce the metabolism of another. So if you ever seen ambulances, you always know that there is at least 1 idiot following the ambulance at a really high speed. That's like an induction enzyme. You've got 1 drug that makes the metabolism of another drug very quick. The opposite is true when the active drug is the metabolite. So I want you to imagine now that instead of having the active drug as the parent drug, you've got the active drug as the daughter drug. So a good example of that is codeine. Codeine is converted to an analogue of morphine via the cytochrome system 2D6. 03:28 So people who are fast metabolizers will have a much more potent shorter term response. 03:36 So, genetic factors that we talked about earlier with our plots are going to affect how we metabolize drugs and a really good example is that let's take a look at patients who immigrate to the United States from ethnic Northern European countries. These patients, 10% of your ethnic European Nordic American patients will have little therapeutic effect from codeine. So you have to use higher doses of codeine or perhaps switch to actual morphine to treat them. On the other hand, when you take a look at patients from the African subcontinent from the African continent, 30% of your ethnic African American patients will be hypermetabolizers, so they will be exposed to excessively high levels of morphine when they take a small dose of codeine. Being aware of racial differences is very important, but also being aware of inhibitors of cytochrome system is important too. 04:32 So I'm going to go through each of these drugs in detail. Amiodarone inhibits cytochrome. 04:39 Fluconazole which is an antifungal agent, inhibits cytochrome. Cimetidine, ritonavir which is HIV drug and grapefruit juice are all inhibitors of cytochrome system. You should memorize this list. You need to know this list code. Okay? So, although I hate telling people to memorize lists without thinking about them, in this particular case you need to memorize this without thinking about it because you need to be able to rattle off these drugs, and of course grapefruit juice as inhibitors of cytochrome. Now there are also inducers of cytochrome system and I've put them in green so you can remember that they make things go faster. The prototypical inducer is rifampin, it is also the most powerful inducer. 05:26 It's a drug that we almost never use in real world clinical practice, but whenever you look at a drug the first thing that we'll say on the drug interaction list is always rifampin and it's used as a testing agent. Carbamazepine or Tegretol is used as an antiseizure medication. Phenobarbital is an antiseizure medication. Phenytoin or Dilantin is an antiseizure medication. Ethanol is of course alcohol. And St. John's Wort is a herbal product that has been particularly problematic for a lot of our patients. You should memorize this list. Now, I'd like to talk to you quickly about St. John's Wort. St. John's Wort is a herbal product that is used in the treatment of depression. It's somewhat effective. 06:13 In fact, its effectiveness is greatly exaggerated by the press but one of the most important things we need to know about St. John's Wort is its effect on drugs. Now, people can die if they take St. John's Wort in combination with their medication. Here is a paper that was released some time ago where heart transplant rejection occurred due to St. John's Wort so these patients who received heart transplants took St. John's Wort and it interacted with their antirejection medications causing heart transplant rejection, in other words death. So, it's a terrible type of drug reaction that was caused by something that we weren't really aware of in the medical community. So it's always important when you're talking to your patients to get them to give you a list of their herbal products they take and preferably stop them all. Now, let's go back to that P-glycoprotein that we were talking about, the P-glycoprotein or MDR inhibitors. So we have a whole list of them. P-glycoprotein, I'm going to repeat this, is also called MDR1. 07:17 It is a transport protein and it moves drugs from outside of the cell into cells or into intestinal lumen. Inhibiting MDR at the gene level causes toxic levels of a drug. So here are inhibitors of P-glycoprotein, verapamil and grapefruit. And substrates of P-glycoprotein are cyclosporine and digoxin. So cyclosporine can be affected quite significantly by grapefruit or by verapamil. You need to memorize this list of P-glycoprotein or MDR1 inhibitors and substrates. Okay, so here's a list of everything. And when you take particular attention, the inducers are generally antiseizure medications, ok? Okay, let's do a question. This is a drug interaction in the coronary care unit. A 55-year-old man was diagnosed with atrial fibrillation. 08:19 His cardiologist prescribed verapamil. He was later found to have atrial fibrillation rhythm with a ventricular rate of 136 beats per minute. His nurse practitioner prescribed digoxin to help with his rate control. Which of the following is false? A. The verapamil and digoxin both cause a reduction in heart rate. B. The verapamil is metabolized through the same cytochrome P450 system and may interact based on a common final pathway. 08:51 C. Verapamil is an MDR1 inhibitor and may result in digoxin toxicity. Or D. Digoxin is cleared by the P-glycoprotein transport molecule. Which is false? Well, let's look at our list and let's look at our answer. So the answer is B. This is wrong. The verapamil is metabolized through the cytochrome P450 system but the P450 system does not play a major role in digoxin metabolism. 09:21 The truth is, is verapamil is an MDR1 inhibitor, it may result in digoxin toxicity. 09:27 The mechanism of verapamil is to reduce blood pressure and reduce heart rate and also digoxin will reduce heart rate so A is correct, C is correct, and D is correct because digoxin is cleared by P-glycoprotein. Remember that P-glycoprotein and the MDR1 we're talking about the same thing. Let's look at another question. Rifampin relevance, realizing rifampin relevance. I love alliterations and you'll see that commonly throughout my lectures. A new drug is tested at Gargantua Pharmaceuticals. The scientist administers rifampin along with a new drug to look for the risk of drug reactions. The following is true, so pick one answer that's true. So the answer, it is induced by rifampin. So take a look at the question. You've got a lot of inhibited there. 2D6, 3A4, 3A5 is inhibited by rifampin and then you have one answer that's induction and then finally the 5th answer is PGP is induced by rifampin. Well that's not true and it's certainly not an inhibitor. Rifampin is an inducer of cytochrome and it actually induces most of the isoenzymes. So the correct answer is D. Let's do a question on cytochrome isoenzymes. Which of the following cytochrome isoenzymes is the most active in metabolizing drugs? Is it 1A2? Is it 2C9? 2C19? 2D6? Or 3A4 and 5? The answer is always 3A4 and 5. And when you're looking at an exam, 3A4 and 5 is going to be your answer and when you're out in clinical practice you're going to need to know if your drug is metabolized through 3A4 and 5 because almost certainly that patient's other drugs will be too. Okay, let's look at a question for inducers of cytochrome P450. Which of the following drugs is the most powerful inducer of cytochrome P450? Is it abciximab? Is it verapamil? Is it phenobarbital? Is it acetaminophen? Or is it rifampin? The answer is rifampin. So remember rifampin is your prototypical inducer. It is also the most widespread inducer and the most powerful inducer.
About the Lecture
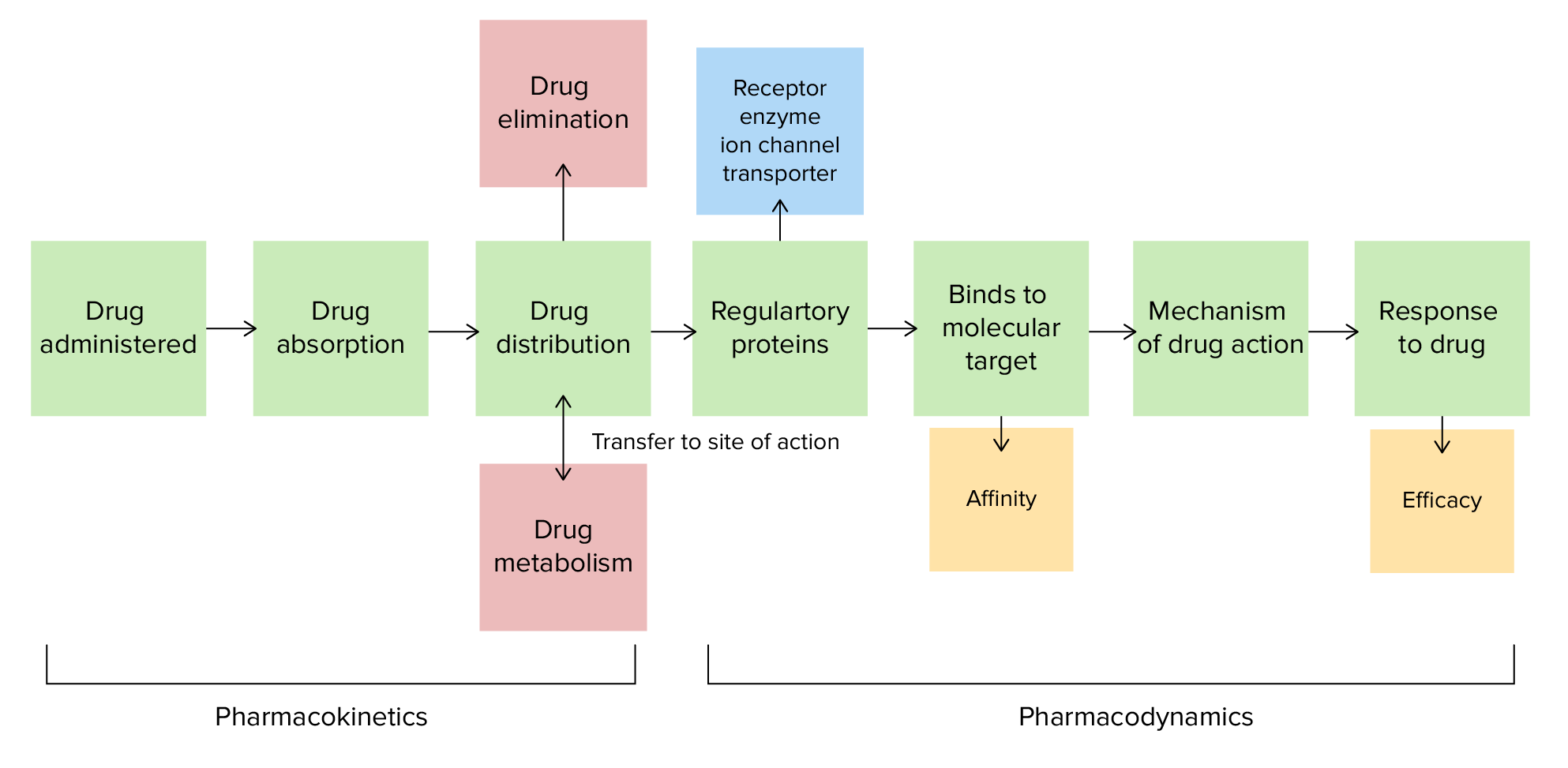
The lecture Factors Affecting Drug Metabolism – Biotransformation | Pharmacokinetics (PK) by Pravin Shukle, MD is from the course Pharmacokinetics and Pharmacodynamics. It contains the following chapters:
- Factors Affecting Drug Metabolism
- Interactions of CYP450
- Inhibitors & Inducers of CYP 450
- P-Glycoprotein Inhibitors
- Case Study: Drug Interaction in the CCU
- Questions and Case Study
Included Quiz Questions
Nortriptyline is metabolized by cytochrome P450 2D6. Which statement regarding homozygotes for inactive alleles of cytochrome P450 2D6 is most accurate?
- They have higher nortriptyline levels in the blood than heterozygotes.
- They have lower nortriptyline levels in the blood than patients with 2 active genes.
- They require a higher dose of nortriptyline to achieve the same concentration seen in heterozygotes.
- They require a higher dose of nortriptyline to achieve the same concentration seen in patients with 2 active genes.
- Homozygotes for inactive alleles of cytochrome P450 2D6 are not possible.
Which drug is an inducer of cytochrome P450?
- Rifampin
- Amiodarone
- Grapefruit juice
- Cimetidine
- Fluconazole
A patient currently takes drug (A), which is metabolized by CYP450. How would you change the prescription for drug (A) once the patient tells you that they are now taking St. John’s Wort?
- Increase the dose of the drug (A) since St. John’s Wort is a CYP450 inducer.
- Increase the dose of the drug (A) since St. John’s Wort is a CYP450 suicide inhibitor.
- Decrease the dose of the drug (A) since St. John’s Wort is a CYP450 suicide inhibitor.
- Decrease the dose of the drug (A) since St. John’s Wort is a CYP450 inducer.
- No need to change the dose of the drug (A) since St. John’s Wort is a CYP450 inhibitor.
Which medication is a P-glycoprotein inhibitor?
- Verapamil
- Rifampin
- Phenytoin
- Carbamazepine
- St John's wort
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
2 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
I would recommend this lecture to all my coursemates, both videos on biotransformation are really helpful!
This is a great overview of CYP and PGP issues. Drug biotransformation is a very complex topic and this is an excellent primer on some key issues. I hope to see more like this.