Playlist
Show Playlist
Hide Playlist
Estrogens and Progestins – Reproductive Pharmacology
-
Slides Estrogens Progestins Reproductive Pharmacology.pdf
-
Reference List Pharmacology.pdf
-
Download Lecture Overview
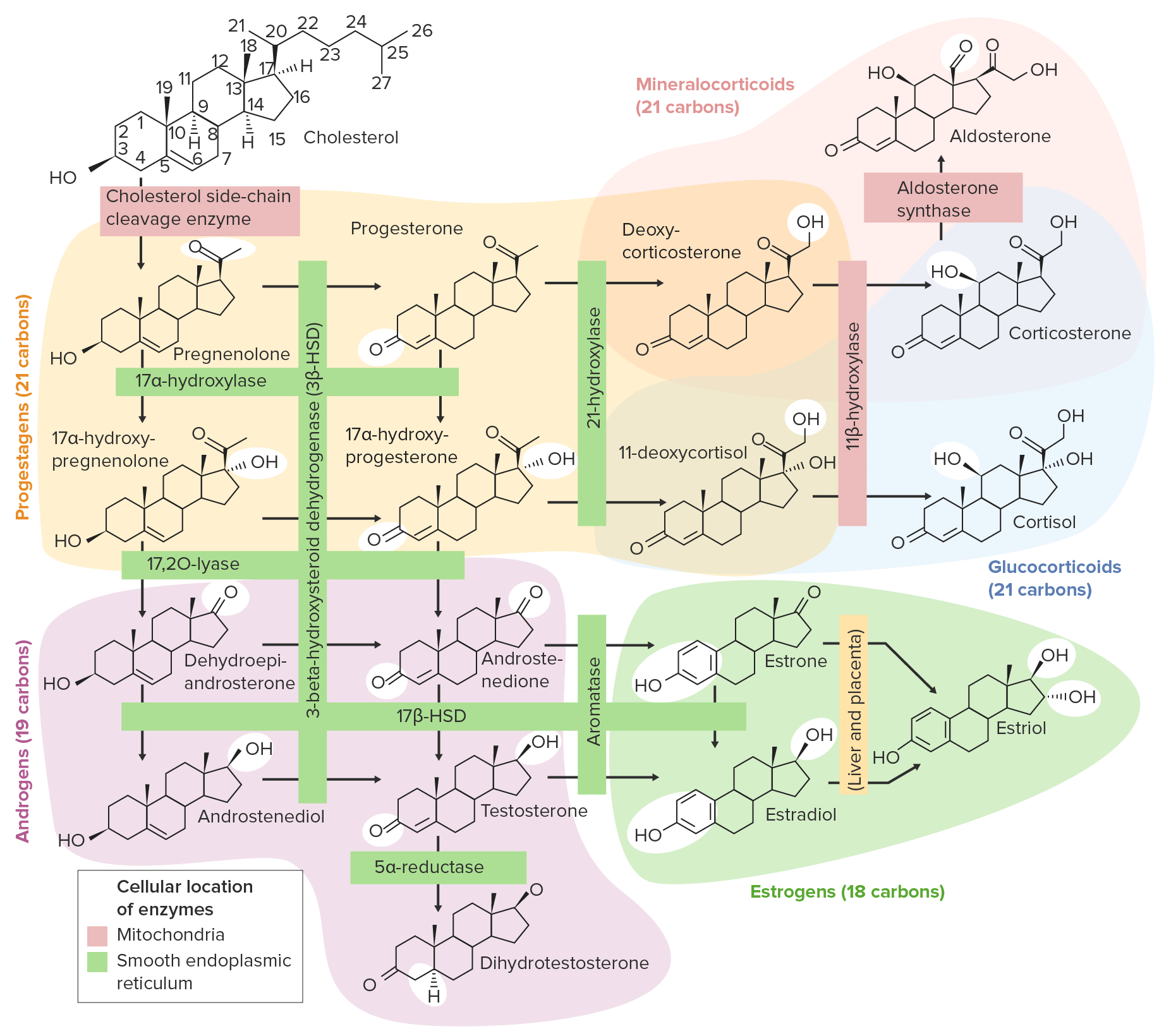
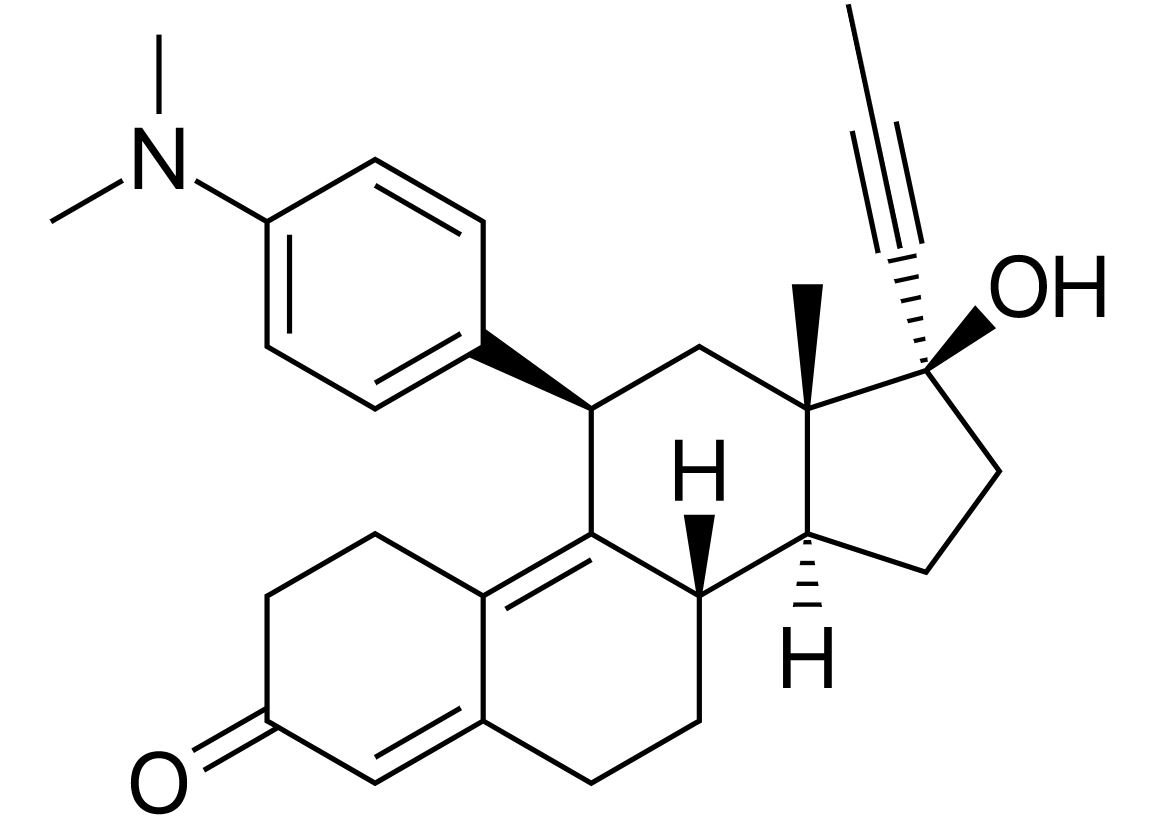
00:00 when you take these medications in uterine tubes and in the endometrium We’re going to start off with estrogens. 00:03 This is a huge topic. And I'll go over in detail for you because it's going to be very relevant when you're out in practice. 00:10 It's also going to be very relevant on the exams. 00:14 With respect to the first of the estrogens, let's talk about estradiols. 00:18 Now, these are available as a patch, as a vaginal cream or as an oral agent. 00:23 Cypionate is this long-acting version for intramuscular injection and we use this as depot injections, in some cases, for hormonal treatment and, in some cases, for anti-conception medication. 00:36 Premarin is also used for hormone replacement therapy. 00:41 Ethinyl estradiol is a high bioavailability oral contraceptive agent that is used quite frequently in oral contraceptive medications. 00:51 Now, the biological effects of these drugs are quite wide and diverse. 00:55 First of all, the obvious effect is going to be gonadal. 00:58 So, it's going to have an effect on female tract development and secondary sexual characteristics. 01:04 There are some central or neurological issues too. 01:08 So, it does reduce secretion of gonadotropins from the pituitary gland. 01:13 This is a normal feedback mechanism. 01:17 This is a controversial area too in terms of lipids. 01:20 We know that estradiols will increase your triglyceride levels. 01:24 It may reduce your LDL levels and it may increase your HDL levels. 01:30 And finally, there are issues surrounding coagulation. 01:33 We know that estradiols will increase coagulability of most patients. 01:40 So, that becomes problematic when you're giving estradiols to women who are at risk for stroke, for example. 01:47 And so, sometimes, we actually withdraw estradiols from patients who are at risk for stroke for that very same reason. 01:54 We also withdraw medications in patients who are hypertensive because we’re worried about risk of stroke. 02:02 I want to mention diethylstilbestrol. 02:06 Now, diethylstilbestrol is important not because we use it, but because we don't use it. 02:12 It was used unsuccessfully in trying to prevent miscarriages in the 1970s. 02:17 It caused severe toxicity, causes ectopic pregnancies, infertility and vaginal adenocarcinomas. 02:27 Now, we are starting to enter into multi-generation issues. 02:32 So, we start talking about DES daughters. 02:34 So, these are the daughters of women who were on diethylstilbestrol in the 1970s and 1960s. 02:42 There's a 40 times increased risk of vaginal clear cell adenocarcinoma in the daughters of women who had taken this medication. 02:50 And we believe that there may also be an increased risk of breast cancer and cervical cancer. 02:55 And we’re unsure if obesity rates are higher in these women and we’re unsure if obesity plays a role in the development of these diseases. 03:04 What about sons? Well, we believe that there may also be an increased risk of cryptorchidism and hypospadias and there may also be a risk of transgenderism and gender dysphoria. 03:16 The last one shouldn't really be called a risk per se, but we have noticed that there may be increased rates of these conditions as DES sons. 03:25 Once again, we’re unsure of the role of obesity in these patients. 03:30 Now, we talk about the third generation. 03:32 So, we’re starting to see third-generation patients. 03:35 Now, if you start to have third-generation effects from a medication, we start worrying about epigenetic abnormalities that were induced by the DES. 03:46 We have seen an increased association with irregular menses. 03:51 Now, the girls who are third-generation are often in their teens at this point in time. 03:56 We’ll have to see what happens to them as they get older. 04:00 We’re not really seeing any convincing evidence of sons or daughter predispositions. 04:05 So, we don't see a gender selectivity in terms of the children of children. 04:11 Remember that this drug was used as a post-coital contraceptive for almost 10 years. 04:17 The manufacturing of this agent discontinued in 1997, but we used it less and less in the 1990s and 1980s. 04:26 Let's move on to emergency contraception. 04:29 So, emergency contraception agents are called post-coital contraceptives or morning-after pills. 04:36 The originator of this type of treatment was the Yuzpe method. 04:41 It was named after Albert Yuzpe who was a Canadian obstetrician who treated initially rape victims in the 1970s. 04:49 They used a combination of estrogens and progestins to allow a termination of the pregnancy or a prevention of the pregnancy immediately after coitus. 05:00 It was replaced later by progestin-only regimens that work much better. 05:05 So, essentially, as you go forward in time, you start to see that the doses of the estrogen component of treatment becomes lower and lower and the progestins become more of a mainstay of treatment. 05:18 So, today, we have many different pills that are used in emergency contraception. 05:23 These morning-after pills prevent pregnancy if given within 24 to 72 hours after coitus. 05:30 Combinations of estrogens and progestins dominate the landscape, but progestin-only products have fewer side effects and are replacing the older pills. 05:40 In terms of how they work, they work by inhibiting ovulation. 05:44 Now, of course, ovulation inhibition is only relevant if these medications are administered in the first half of the cycle before the luteinizing hormone surge. 05:55 There is also a decreased receptivity of a zygote in uterine tubes and in the endometrium when you take these medications and there is altered cervical mucus gland formation that also reduces receptivity. 06:10 Here is a summary of the major characteristics of the common emergency contraceptive methods available in the United States. 06:17 t’s important to note that EC is used to prevent pregnancy after unprotected intercourse by inhibiting ovulation or interfering with the fertilization of an ovulated egg. 06:29 ECs are not designed to terminate an established pregnancy and are not abortion-inducing drugs Among the most efficacious EC methods are intrauterine devices (IUDs). The Copper IUD, known as Paragard, and the LNG IUD, sold as Mirena, demonstrate pregnancy rates of less than 1% but require clinician insertion. 06:55 When considering oral medications, there is Ulipristal acetate, also known as UPA, sold under the brand name Ella, and oral LNG, commercially known as Plan B One-Step, among others. 07:09 These oral options have pregnancy rates of approximately 1 to 3%. Notably, Plan B One-Step is available over the counter, which allows for accessibility without the need for a prescription. 07:23 Here's an example of oral contraceptives. 07:26 Oral contraceptives are progestins only or can be combinations with estrogen. 07:32 They are monophasic, which is the same dose every day, or they can be multiphasic, which means that they get variable doses each day. 07:41 There is sometimes a placebo week. 07:43 So, you can see in this particular example, There is sometimes a placebo week. 07:43 So, you can see in this particular example, we have the bottom row of seven tablets which are a placebo week. 07:49 This is usually the week that the patient is allowed to have the actual period. 07:56 Oral estrogens also can be used for non-contraceptive needs. 08:00 Sometimes, we treat hypogonadism in young females with oral estrogens. 08:05 Sometimes we treat older women with hormone replacement therapy, particularly if they've had surgical removal of their ovaries or if they’ve had premature ovarian failure. 08:15 Finally, in postmenopausal women, we sometimes use hormone replacement therapy, although that type of treatment is falling out of favor over the past five years. 08:26 In terms of side effects from the oral contraceptive agents or oral estrogens, there is an increased risk of endometrial cancer. 08:35 Now, we can reduce or mitigate that risk by combining this medication with a progestin. 08:42 There is a small increase in breast cancer risk, particularly in postmenopausal women. 08:48 If you have a patient who has breast cancer, it's particularly important to know the ER status of that patient or estrogen receptor status because women who have ER positive breast cancers are absolutely contraindicated from taking oral estrogens. 09:08 We may believe – we believe that there may be a small increase in cardiovascular risk as well. 09:13 This involves postmenopausal women. 09:15 We know, for example, that a postmenopausal woman is actually at lower risk for cardiovascular disease than a man in the same age group and we start to see an increase in risk when we start back the estrogen therapies. 09:29 In terms of toxicity and accidental overdose, clearly, nausea is the first one. 09:34 Breast tenderness is certainly present in these patients. 09:38 They can develop migraines. 09:40 The grave concern that we all have is thromboembolic disease because, remember, estrogens can be pro-coagulant. 09:47 There are theoretical and sometimes documented cases of gallbladder disease, hypertriglyceridemia and an exacerbation of hypertension. 09:58 Let's move on to the progestins. 10:02 Progesterone is the major progestin in humans. 10:06 It induces secretion of endometrium and also maintains a healthy endometrium for pregnancy. 10:13 Medroxyprogesterone is the prototypical oral synthetic progestin. 10:18 That is the one that you need to remember. 10:21 There are other ones as well that are older, more androgenic forms. 10:25 These agents are also being replaced by newer agents that are actually much better in efficacy. 10:32 Now, the synthetic progesterones support endometrium, but they don't support the endometrium for pregnancy, which is why, in some cases, they can be used in women who don't want to get pregnant. 10:45 In terms of the synthetic progestins, they do inhibit ovulation. 10:50 And in hormone replacement therapy, they are used as an adjunct to estrogen. 10:54 And they do that because it helps reduce endometrial cancer risk. 10:59 So, what are the side effects of the progestins? First of all, they do alter carbohydrate metabolism and they may stimulate fat deposition as well. 11:09 We do know that it decreases the HDL level. 11:12 We sometimes see a reduction in bone density in the long term in people who are on progestins only and we believe that it may be due to suppressed estrogen levels. 11:24 We know that there is delayed ovulation after you stop progestins. 11:28 So, sometimes, patients may take as long as three months to have ovulation start up again. 11:34 And high doses of progestins will suppress gonadotrophic releasing hormone and luteinizing hormone and follicular stimulating hormone secretion from the hypothalamus and pituitary.
About the Lecture
The lecture Estrogens and Progestins – Reproductive Pharmacology by Pravin Shukle, MD is from the course Reproductive Pharmacology. It contains the following chapters:
- Estrogens
- Progestins
Included Quiz Questions
Which patient is least likely to benefit from estrogen therapy?
- A 45-year-old mother with a history of DVT
- A 55-year-old woman with osteopenia
- A 35-year-old woman who often has painful and heavy periods
- A 51-year-old woman who is experiencing hot flashes
- All of these patients will benefit greatly from estrogen therapy.
What is NOT a side effect of DES (diethylstilbestrol)?
- Menopause
- Vaginal adenocarcinoma
- Ectopic pregnancy
- Infertility
- Increased risk of breast cancer
What is the primary mechanism of action of the "morning after pill"?
- Inhibition of ovulation before the LH surge
- Induction of uterine contractions
- Cervical gland dysfunction
- Reduced implantation receptivity of the fallopian tubes
- Drying of the vaginal mucosa
Estrogen use increases the risk of which condition?
- Endometrial cancer
- Color blindness
- Liver cancer
- Skin hemangiomas
- Osteopenia
The addition of progestin to long-term estrogen therapy is most likely to reduce the risk of which condition?
- Endometrial cancer
- Myocardial infarction
- Stroke
- Invasive breast cancer
- Venous thromboembolism
What is NOT an appropriate use of estrogen therapy?
- Treatment of deep vein thrombosis
- Treatment of hypogonadism
- Hormone replacement therapy in premature ovarian failure
- Hormone replacement therapy in bilateral oophorectomy
- Hormone replacement therapy in postmenopausal women
What is NOT a typical side effect of estrogen therapy?
- Hypotension
- Breast tenderness
- Headache
- Depression
- Nausea
Estradiol treatment is not started or is withdrawn in women who are...? Select all that apply.
- ...at risk for stroke.
- ...over the age of 50, regardless of health condition.
- ...lactose intolerant.
- ...hypertensive.
- ...experiencing frequent urinary tract infections.
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
Las explicaciones son simples pero completas, es fàcil de entender