Playlist
Show Playlist
Hide Playlist
Esophagus – Pulmonary Structures and Esophagus
-
Slides 03 Thoracic Viscera Canby.pdf
-
Download Lecture Overview
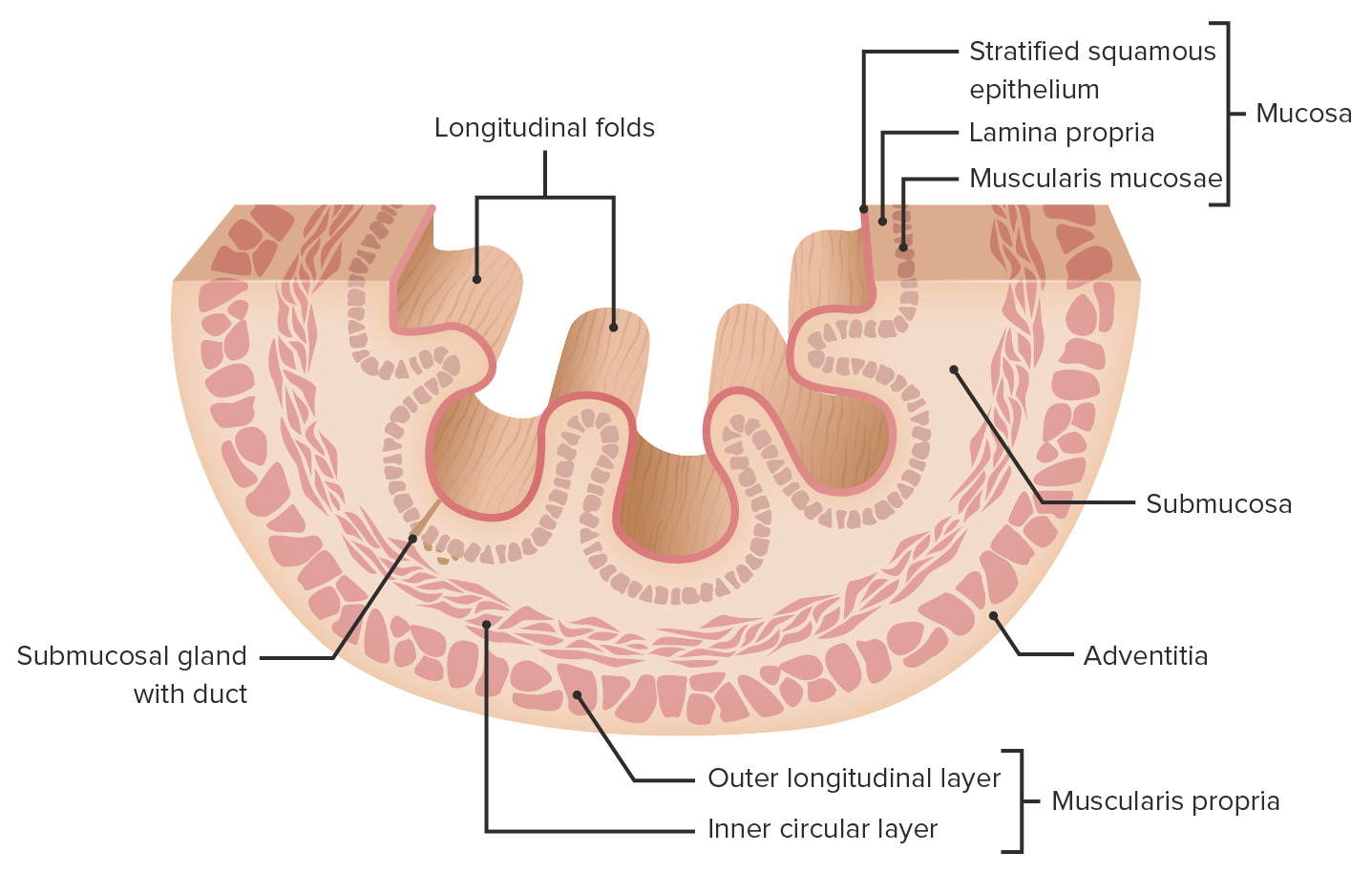
00:00 Now, let’s shift our focus to the esophagus. 00:04 And the first aspect about the esophagus is the fact that it’s divided into three parts. 00:12 We have, and it’s best seen here in this lateral view, the most superior portion of the esophagus. This is the cervical part. The most extensive part of the esophagus will travel within the thoracic cavity and that will be called the thoracic part. And then the esophagus will pass through at the esophageal hiatus within the diaphragm and become the abdominal esophagus. And then the abdominal esophagus will promptly empty into the cardiac region of the stomach. 00:51 The esophagus has layers associated with its wall. And those four layers are the mucosa, submucosa, muscularis externa and then adventitia throughout most of its length. But, within the abdominal cavity, we’ll have a serosa representing the outermost layer. 01:17 If we take a look at our illustration, here is the mucosa. Here is the deepest layer here, this thin red muscular membrane. And then the most superficial layer, the mucosa, will be the epithelium of the esophagus. Lying deep to the mucosa is the submucosa. And then we have a very thick muscularis externa with two muscle layers: an inner circular layer that we see here and then an outer longitudinal layer shown here. And then the layer that’s the outermost layer, this again is the tunica adventitia: connective tissue. But, again, if you’re looking at the abdominal part of the esophagus, the connective tissue will be limited most externally by a thin epithelial layer becoming the serosa. 02:20 This slide depicts various constrictions that can be seen along the length of the esophagus. 02:28 Three of them are identified on this illustration. The uppermost point of constriction of the esophagus is at this level. This represents the upper esophageal sphincter region. And this is at a junction between the pharynx and the esophagus. So, we can refer to this point of constriction as the pharyngo-esophageal constriction. So, this is a natural constriction point. 02:58 Down more in the middle of the thoracic esophagus we have a couple of other structures that put pressure on the esophagus thus serving as a combined point of constriction. We have the aorta and the right primary bronchus. And if we combine these two structures, this represents the aorto-bronchial constriction. And then the third and final constriction is where the esophagus will pass through the esophageal hiatus within the diaphragm. These constrictions do have clinical significance. The first example is during a procedure where you may have to scope the stomach and look for the presence of an ulcer or bleeding ulcer. 03:52 In order to do that, you have to advance the endoscope through the esophagus and gently pass the endoscope through these various points of constriction. If one is too aggressive with the advancement of the scope, you can penetrate and damage the wall. Another clinical example is with elderly individuals. In the elderly, they have decreased salivary-gland secretions and, if they’re taking numerous pills and don’t drink enough water, a pill can lodge at these points of constriction. And if a pill remains lodged at a point of constriction for too long of a period of time, that can irritate the mucosa of the esophagus and cause esophagitis. 04:43 This slide represents the fact that the esophagus, like other tubular organs, can form diverticula. 04:53 There are three main diverticular sites. The first one is at this level. This is occurring at the junction between the pharynx and the esophagus itself. And you can see the fact that there is a diverticulum or an outpouching of mucosa and submucosa at this superior point. 05:12 This is referred to as a pharyngo-esophageal diverticulum also known by the eponym Zenker’s diverticulum. Another area of the esophagus that can develop diverticula is the mid-esophagus. 05:29 And here you have a diverticulum within the mid-esophagus. And then the third most frequent site is a formation of a diverticulum just above the level of the diaphragm. That will be termed an epiphrenic diverticulum. 05:48 This slide of the esophagus is demonstrating two triangles that are located at the level of the proximal esophagus. Those two triangles are Killian’s triangle and Laimer’s triangle. 06:04 And Killian’s triangle is represented in this particular area. The apex of Killian’s triangle is projecting superiorly. The base is inferiorly directed. And then the Laimer’s triangle is shown right below. So, its base is superior and its apex is directed inferiorly. 06:29 The borders of Killian’s triangle will be the cricopharyngeus muscle. And we have the transverse muscle fibres of the cricopharyngeus muscle. This is the inferiormost component of the inferior pharyngeal constrictor. It also represents the upper esophageal sphincter. 06:51 And then, this portion of the inferior constrictor, where we have these oblique fibres, this represents the thyropharyngeus part of your inferior constrictor. And so, the area between those oblique fibres in the transverse fibres represents Killian’s triangle. This is a potential site of weakness and when a Zenker’s diverticulum or a pharyngo-esophageal diverticulum forms, it is within Killian’s triangle. 07:21 Laimer’s triangle is going to be bordered by the transverse fibres of the cricopharyngeus at its base. And then this oblique orientation here coming to a convergence at the apex represents a structural defect within the muscularis externa of the esophagus. This area just has the circular fibres of that muscularis externa and the longitudinal fibres are very poorly developed here. This is another potential site of weakness and less frequently it too can provide for the formation of a diverticulum. 08:04 Here we have a normal endoscopic view of the esophagus. Here, you can appreciate the whitish nature of the mucosa. This is imparted by the fact you have a thick epithelial stratified squamous epithelium here, so it’s difficult for the blood vessels to shine through. 08:26 Now, the next slide is another endoscopic view, but this is a pathologic view of the esophagus. Here the esophagus looks very, very angry and you can see that there are bulges underneath the mucosal components. And these bulges represent dilated esophageal varices. And esophageal varices can form when you have hepatic portal hypertension. And the causative factor for hepatic portal hypertension is cirrhosis of the liver. In severe cases, these esophageal varices can rupture and as a result, the patient will vomit blood as a result of that rupture. 09:23 That now brings us to the key take-home messages from this presentation. 09:30 The lungs are contained in pleural cavities limited by visceral pleura and parietal pleura. 09:35 A thoracentesis may be performed to remove excess fluid from the pleural recesses. 09:44 The trachea begins at vertebral level C6 and bifurcates into primary bronchi at T4/T5. 09:53 The wall of the trachea consists of the mucosa, then moving outwards, submucosa, the cartilage fibromuscular layer and then, the externalmost layer’s your adventitia. 10:07 Primary, secondary and tertiary bronchi respectively supply the entire lung, lobes and bronchopulmonary segments. 10:18 The esophagus is divided into three parts: cervical, the thoracic part, which is its longest part, and then a short abdominal part. 10:30 The esophagus is anatomically constricted at three main points and is subject to formation of diverticula. 10:39 The esophageal wall consists of four layers: mucosa, submucosa, muscularis externa and throughout most of its extent, an adventitia except for the short abdominal segment which is limited by a serosa. 10:57 Thank you for joining me on this lecture about the pulmonary structures and the esophagus.
About the Lecture
The lecture Esophagus – Pulmonary Structures and Esophagus by Craig Canby, PhD is from the course Thoracic Viscera with Dr. Canby.
Included Quiz Questions
What term describes the most superior position of the esophagus?
- Cervical
- Thoracic
- Axial
- Abdominal
- Peptic
What are the layers of the esophageal wall? Select all that apply.
- Submucosa
- Pseudostratified epithelium
- Adventitia
- Muscularis externa
- Tunica mucosa
What is contained in the tunica adventitia?
- Loose connective tissue
- Stratified squamous epithelium
- Circular muscle layer
- Mucous glands
- Cilia
The 3 constrictions of the esophagus for geriatric patients are clinically important because pills may get lodged during swallowing. Why would this occur?
- Poor salivary flow
- Poor mechanical control
- Poor muscle strength
- Reduced elasticity of muscles
- Poor elasticity of the esophagus
During an endoscopic procedure, the physician finds it difficult to advance the scope beyond the second of 3 constrictions. What structure(s) are responsible for this constriction?
- Aorta and right bronchus
- Junction of the pharynx and the esophagus
- Diaphragm
- Left bronchus
What is the location of the esophageal diverticulum through Killian's triangle?
- At the junction of the pharynx and the esophagus
- Mid-esophagus
- Immediately superior to the diaphragm
- Through the diaphragmatic hiatus
- Immediately inferior to the diaphragm
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |