Playlist
Show Playlist
Hide Playlist
Diuretics – Drugs in Hypertension
-
Slides Diuretics Drugs Hypertension.pdf
-
Reference List Pharmacology.pdf
-
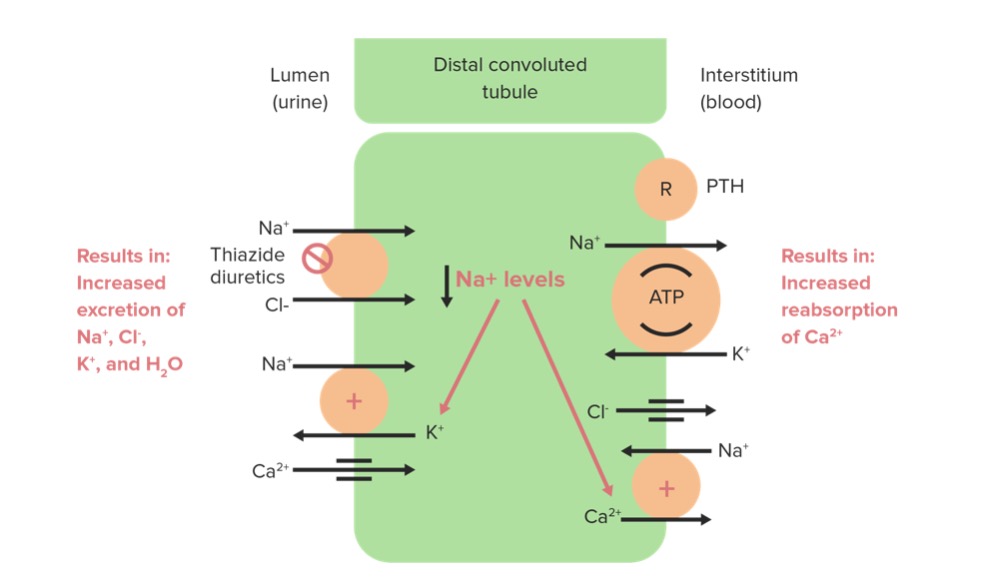
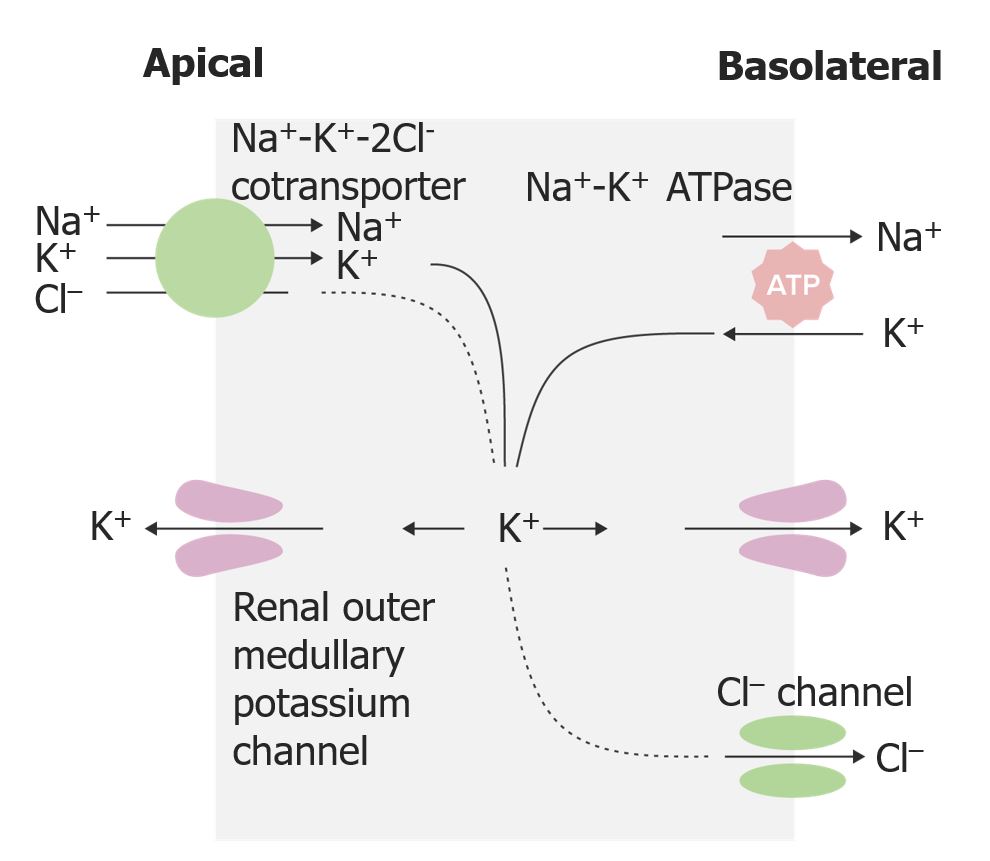
Download Lecture Overview
00:01 Let’s start off with osmotic diuretics. 00:03 This is the most simple of mechanisms. 00:05 Mannitol is a prototypical osmotic diuretic. 00:09 It acts as an osmotic agent within the glomerulus. 00:12 Water is being pulled because of the osmotic forces that are being generated. 00:19 It also works in intracranial hypertension and in fact, that’s one of the main areas that we use it in is to try and reduce the pressure within the brain. 00:29 Acetazolamide is another diuretic. It is in the category of carbonic anhydrase inhibitors and it inhibits this enzyme, carbonic anhydrase so that you end up having more sodium trapped in the proximal convoluted tubule. 00:46 There is more sodium bicarbonate and chloride ion left in that tubule because you’ve inhibited this enzyme. 00:54 This also ends up causing a bit of a metabolic acidosis. 00:57 So, you have to be aware of this particular problem in your patients but we can take advantage of this because we can actually use a metabolic acidosis in the treatment of certain types of altitude sicknesses. 01:10 When you have a metabolic acidosis, it triggers your respiratory system to blow off carbon dioxide. 01:17 Well, you blow off carbon dioxide but because you’re high up in altitude, you’re also pulling in more oxygen out of the rarified air. 01:24 That’s how we use - that’s how we use acetazolamide in altitude sickness. 01:30 It’s quite effective as well. 01:32 Side effects include hypokalemia, hyponatremia or low sodium and hyperchloremia. 01:41 The next category of drugs in the diuretic class are the loop diuretics. 01:46 Now, these are the most powerful of the diuretic class. 01:50 The prototypical drug and the oldest of the drug class is furosemide. 01:55 If patients are allergic to furosemide, we sometimes will use ethacrynic acid which is sold as Edecrin and bumetanide. 02:04 Now, these drugs reduce sodium reabsorption in the thick ascending loop of Henle. 02:12 I really want you to memorize that because that is on your exam. 02:16 Hands down, it’s going to be the question that you’re going to be asked and in fact, I have some questions here in the Lecturio question bag that also specifically ask you this, so, it’s really important that you know that it reduces sodium reabsorption in the thick ascending loop of Henle. 02:33 It again is the most powerful diuretic. 02:36 It may cause hypokalemia and it may cause hyponatremia or low sodium. 02:43 Now, I just wanna really emphasize something here. In the physiology lectures, you will see that the professor is talking about the countercurrent mechanism. 02:53 Lasix is using the countercurrent mechanism to its advantage to exert a particularly powerful effect but Lasix is not affecting the countercurrent mechanism, so, one of the questions that we have, some of our students have had real problems answering the question. 03:12 So, I wanna be very clear that it uses the countercurrent mechanism but it’s not actually affecting it. 03:18 The countercurrent mechanism may be affected in the long run when people have severe electrolyte abnormalities. 03:25 Hydrochlorothiazide is in the category of thiazide diuretics. 03:31 As you can tell, I’m going down the nephron and that’s how I’m listing the drugs but in terms of importance, even though this is fourth on my list, it is the most important class of drugs in the diuretics and the reason why is because it is usually the first line agent that we use in the treatment of hypertension and these are often first line agents in the treatment of hypervolemia. 03:54 They’re generally a milder form of diuretics, so, they’re not as strong as the loops. 04:00 They’re often used as a combination to ACE inhibitors and the angiotensin receptor blockers and they’re actually given as a combination pill. 04:08 Indapamide is purported to be better tolerate then say hydrochlorothiazide. 04:14 I’m not entirely sure that that’s true but there are a lot of people who are suggesting that. 04:20 There are other drugs as well, so, Metolazone for example can be given in acute situations and we have something called the metolazone mix. 04:28 The metolazone mix is when you take say five milligrams of metolazone, you give it to the patient, and then, about a half hour later, you give Lasix and you get a profound diuresis because you get super loading of the nephron so there’s a very powerful synergistic effect between the two agents. 04:48 Amiloride is another type of diuretic. It comes in the category of the potassium sparing diuretics. 04:55 So, you can see that instead of working in the distal convoluted tubule, you’re actually going to have effects in the collecting ducts or in the high collecting duct. 05:05 It inhibits sodium reabsorption in that collecting tubule, allowing sodium, and other - and water and other solutes to be excreted. 05:16 Now, there are several channels that we have to be aware of in the collecting duct. 05:20 There’s the ENAC or the Epithelial Sodium Channel. 05:25 There the NHE1 or the Sodium Hydrogen antiporter. 05:30 This is important in heart failure and we will be talking about that later. 05:35 And there is the ASIC or the Acid-sensing ion channel. 05:40 And, so, when you talk about Amiloride, you’re seeing an effect on all three of these different types of ports. 05:46 So, it’s important to recognize that the complex mechanism of Amiloride will allow us to treat patients who are prone to low potassium with this diuretic. 05:55 We achieve diuresis without losing too much potassium. 06:00 Amiloride has a low risk of hyperkalemia but the risk isn’t zero. 06:04 Now, the mechanism behind causing hyperkalemia with the use of Amiloride is a bit beyond the level of this course and it is not going to be relevant for your exams. 06:13 But just from a practice point of view, be aware that sometimes, that can occur in very rare and unusual circumstances. 06:20 Amiloride can cause a metabolic acidosis. 06:24 A metabolic acidosis is occurring because you’re losing basic ions through the urine because of its action. 06:32 The next drug within this category is spironolactone but it is a little bit different from Amiloride. 06:38 Now, we know that it acts as an aldosterone blocker and it inhibits the reabsorption of sodium. 06:44 It also is shown to reduce the mortality of patients with significant heart failure and it’s interesting because it’s the only one that has shown this. 06:54 So, it’s a - it’s a staple or a mainstay of heart failure therapy. 06:59 The unique thing about spironolactone versus say, Amiloride is that is also has a strong antiandrogen effect. 07:05 The antiandrogen effect is used for that reason in some patients. 07:10 It works as that blocker of the androgen and sometimes, we use it in association with testosterone-related skin problems, the most common of which is hirsutism in women. It’s a very effective treatment. 07:23 The doses are a little bit different. In terms of the Antiandrogen effect, we use relatively low doses, 25, 50, sometimes 100 milligrams. 07:33 In terms of the diuretic effect, we’re using 50, 100, 200, 300, 400 milligrams so that it’s different dosing having different effects. 07:44 Triamterene is another potassium-sparing diuretic. 07:47 It also inhibits sodium reabsorption in the collecting tubule which allows more of the sodium and the water to be excreted. 07:55 It works almost exclusively through the epithelial sodium channel or ENaC. 08:02 There’s a very low risk of low potassium in these patients. 08:04 It can cause elevated potassium or hyperkalemia in some patients. 08:09 So, you have to use it with care. It will cause a metabolic acidosis for the same reason as the others and you can also get a nephrolithiasis and specifically, it’s with the calcium oxalate stones. 08:23 So, be aware that if patients develop nephrolithiasis and they’re on triamterene, stop the triamterene and treat the nephrolithiasis appropriately. 08:33 Okay, that’s it, I’m glad that you made it through that lecture. 08:37 You’re going to do very well on your exams. Go out there, go to your exams, and show them what you know.
About the Lecture
The lecture Diuretics – Drugs in Hypertension by Pravin Shukle, MD is from the course Cardiovascular Pharmacology. It contains the following chapters:
- Osmotic Diuretics
- Carbonic Anhydrase Inhibitors
- Loop Diuretics
- Thiazide Diuretics
- Potassium Sparing Diuretics
Included Quiz Questions
Triamterene is most likely to cause which type of renal stone?
- Calcium oxalate
- Uric acid
- Struvite
- Cysteine
- Calcium phosphate
Acetazolamide primarily affects which part of the nephron?
- The proximal convoluted tubule
- The distal convoluted tubule
- The ascending loop of Henle
- The descending loop of Henle
- The collecting duct
Ethacrynic acid primarily affects which part of the nephron?
- The thick ascending loop of Henle
- The thin ascending loop of Henle
- The proximal convoluted tubule
- The distal convoluted tubule
- The collecting duct
Indapamide primarily affects which part of the nephron?
- Distal convoluted tubule
- Proximal convoluted tubule
- Thick ascending loop of Henle
- Thin ascending loop of Henle
- Collecting duct
Which medications are most likely to raise serum potassium?
- Amiloride, spironolactone, triamterene
- Acetazolamide, spironolactone, furosemide
- Amiloride, hydrochlorothiazide, indapamide
- Furosemide, acetazolamide, atenolol
- Abciximab, hydrochlorothiazide, spironolactone
Customer reviews
4,7 of 5 stars
| 5 Stars |
|
8 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
1 |
| 1 Star |
|
0 |
easily explained .well organized . Mentioned what we need to know with explanations .
Very complicated topic that it's not explain with enough clarity
It's always useful to see a good review of hard subjects like this.
Very knowledgeable and soothing voice. Helps with remembering things more efficiently