Playlist
Show Playlist
Hide Playlist
Dermatitis Herpetitiformis: Pathophysiology
-
Reference List Pathology.pdf
-
Slides Dermatitis Herpetitiformis Pathophysiology.pdf
-
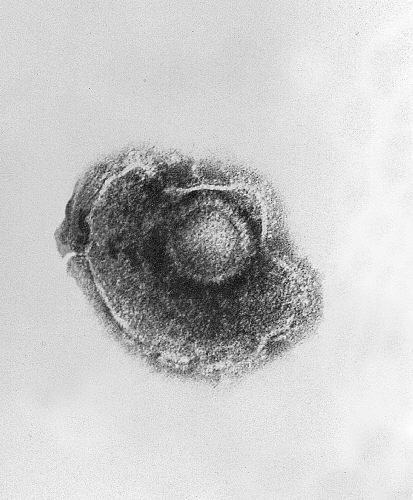
Download Lecture Overview
00:01 Welcome. In this talk, we're going to discuss yet another blistering disease. This one is dermatitis herpetiformis, although not as common as some other blistering disorders. 00:13 This one is interesting because of its association with gluten sensitive enteropathy, otherwise known as celiac disease. 00:21 So dermatitis herpetiformis is uncommon. 00:24 It is autoimmune, it's blistering, and characteristically the lesions are intensely pruritic. Patients will just scratch themselves crazy. 00:36 So the epidemiology of this as I say, it's pretty uncommon. 00:39 It is mostly seen in northern European heritage. 00:43 That's probably because of the association with certain HLA haplotypes. 00:48 The prevalence is not high. 00:52 One to, you know, 1 to 75 per 100,000 people. 00:56 It also depends on people's attention to their diet, as we'll see, occurs more frequently in males than females. 01:03 Interestingly enough, since most autoimmune diseases tend to predominate in women, it is, as I've already said, it's associated with gluten sensitive enteropathy and with chronic disease that isn't well controlled. 01:18 There is a potential there's an associated risk for developing lymphoma, probably as a result of chronic T cell activation. 01:27 Okay. Let's get into some of the pathophysiology because this is where it gets interesting. So there are a variety of genetic factors. 01:34 As I've already intimated, the majority of patients will have a particular HLA haplotype DQ2 or DQ8. 01:42 Do you need to memorize that? No probably not. 01:45 Um, there is certainly an increased risk among first degree relatives who have the same disease, in part because of the HLA haplotype, but probably also other associated inflammatory, genes. The immune response is specifically targeted. 02:04 It's an antibody-mediated response. 02:06 Although there is an element of CD4, um, Th1 driven pro-inflammatory disease as well, but it's primarily the deposition of IGA. 02:17 So as opposed to other blistering lesions that we've talked about in other places, pemphigus and pemphigoid, this is not IgG but rather IgA. 02:27 And we get binding with the secondary neutrophilic infiltrate into the area where this binds at the dermal epidermal junction. 02:36 Now let's discuss the pathophysiology of dermatitis herpetiformis. 02:40 To truly understand this condition we need to start with its close relative celiac disease. 02:47 Grasping the underlying mechanisms of celiac disease is essential to appreciating the immunological connections that also drive dermatitis herpetiformis. 02:56 So let's begin with a with a brief overview of celiac disease pathophysiology. 03:02 First. Gluten from wheat and other grains is partially broken down by human proteases in the gastrointestinal tract. 03:10 However, certain gluten fragments, often called peptides, are resistant to complete digestion. 03:17 Tissue transglutaminase, or tTG comes into play next. 03:22 It catalyzes the deamidation of these gluten peptides by modifying these peptides. 03:28 Ttg makes them bind more effectively to specific molecules called HLA-DQ2 or HLA-DQ8, on antigen-presenting cells or APCs. 03:39 Once the delimitated gluten peptides bind to HLA-DQ2 or HLA-DQ8 on APCs, gluten-specific CD4 T cells recognize these peptides. 03:52 In response, these T cells become activated and start producing pro-inflammatory cytokines such as interferon-gamma , IFN gamma, and interleukin 21, IL- 21. 04:05 The inflammatory environment in the intestine, also triggers the production of IL -15. 04:11 This potent cytokine not only activates intraepithelial lymphocytes or IELs, but it also makes effector T cells resistant to suppression by regulatory T cells. 04:23 This dampens the usual checks and balances that might otherwise limit inflammation. 04:28 As IELs become activated, they transform into cytolytic natural killer NK like cells. These IELs recognize stress signals on enterocytes the intestinal lining cells and destroy them, leading to the characteristic damage seen in celiac disease. Simultaneously, activated B cells develop into plasma cells. 04:50 These plasma cells produce immunoglobulin A IGA antibodies that target both gluten and tissue. Transglutaminase. 04:59 Ttg. These antibodies are important markers used in diagnosing celiac disease. 05:05 All of these events persistent gluten peptides, their deamidation by TTG, the activation of gluten specific T and B cells, the production of pro-inflammatory cytokines, and the transformation of IELs into cytotoxic NK like cells collectively drive the hallmark intestinal damage of celiac disease. 05:25 This damage manifests as villous atrophy, crypt hyperplasia, and increased inflammation in the small intestine. 05:34 But celiac disease doesn't just affect the gut. 05:37 Some individuals with CED develop the topic of today's conversation dermatitis herpetiformis. This occurs when the immune system's response to gluten also generates antibodies that can cross-react with an enzyme in the skin called epidermal transglutaminase or ETG. 06:01 As previously mentioned in celiac disease, plasma cells produce IgA antibodies against tissue transglutaminase TTG. 06:12 In some individuals, these antibodies also cross-react with epidermal transglutaminase, eTG. When these cross-reactive IgA antibodies circulate to the skin, they can deposit in areas of high eTG concentration, such as the dermal papillae. 06:30 This deposition, coupled with the activation of the complement system by the immune complexes, amplifies neutrophil recruitment and promotes local inflammation. 06:41 So in the skin, macrophages bind the IgA- eTG complexes via their receptors, triggering their activation. 06:50 This activation leads to the secretion of interleukin eight, IL-8 , which recruits neutrophils to the area. 07:01 The accumulation of neutrophils in the superficial dermis ultimately results in blister formation and the intensely itchy lesions characteristic of dermatitis herpetiformis. Neutrophil byproducts and cytokines alongside IL 31 further drive the local inflammation and itching, completing the cycle of rash formation. 07:28 The clinical presentation then based on this pathophysiology. 07:33 It is grouped pruritic. 07:36 Again, I can't emphasize how itchy this particular disease is. 07:40 Little papules and vesicles. 07:42 The blister is above the dermal epidermal junction. 07:45 So it is right. It is subepithelial. 07:49 It will occur typically on flexor surfaces, but it also can occur on the trunk and buttocks. They can be very localized. 07:56 They can be very widespread. 07:59 With chronic disease that is poorly controlled. 08:02 You may see oral manifestations, but they tend overall to be rare. 08:07 And there may be, again with chronic disease, even tooth or enamel defects with grooves, pits and discoloration really uncommon, but with poorly controlled disease that starts early in life, this can occur. The gastrointestinal manifestations, on the other hand, are because of the gluten sensitive enteropathy. 08:25 You have a basically a delayed type hypersensitivity response with T cells that are reacting to modified gliadin. 08:34 That's being seen in the environment because you keep eating all that wheat-based diet. 08:41 So you get bloating and cramping and pain and diarrhea and constipation. If you want to learn about celiac disease, Lecturio has a lecture on that that I happen to know who gave. That was me. 08:52 All right, the clinical course. 08:54 It's usually a lifelong condition if you are prone to developing these antibodies, if you have a gluten sensitive kind of genetic makeup, you're going to have it for your entire life. Um, depending on your diet and dietary indiscretion, symptoms can range from every now and then to continuous. 09:14 If you live on pasta every day, you have beer every day, whatever. You will have the manifestations on a daily basis. 09:23 Some patients, the lucky ones, can have a spontaneous remission. 09:26 This is probably because of the development of T regulatory cells or other counter-regulatory mechanisms that turn off that particular response to the gliadin. 09:37 How do we make the diagnosis? Well, in fact, this is one where biopsy is really important. 09:41 So the pathologist plays a role. 09:43 You can do a direct immunofluorescence analysis looking at the lesions and looking for the type of immunoglobulin you want to see IgA bound to the dermal epidermal junction. You can also look in the peripheral blood using an Elisa, an enzyme linked immunosorbent assay for IgA that is specific for epidermal transglutaminase. How do we manage this? So the first line is to stop eating gluten. 10:15 And then usually the disease is going to go away. 10:18 If that's not entirely possible or for for disease that for whatever reason continues despite having taken gliadins out of the diet, you can reduce neutrophil recruitment and activation with various drugs like dapsone or sulfonamide. And then always because it's autoimmune inflammatory corticosteroids can be administered. And with that we've covered another one of the blistering diseases. 10:45 Dermatitis herpetiformis.
About the Lecture
The lecture Dermatitis Herpetitiformis: Pathophysiology by Richard Mitchell, MD, PhD is from the course Blistering Skin Disorders.
Included Quiz Questions
Which population shows the highest prevalence of dermatitis herpetiformis?
- People of northern European heritage
- Mediterranean populations
- Asian populations
- African populations
- South American populations
Which type of antibody is characteristically involved in dermatitis herpetiformis?
- IgA
- IgG
- IgM
- IgE
- IgD
Where do the lesions of dermatitis herpetiformis typically appear?
- Flexor surfaces
- Palms and soles
- Oral mucosa
- Scalp
- Nail beds
What protein complex triggers the autoimmune response in dermatitis herpetiformis?
- Deamidated gliadin with transglutaminase
- Desmosomes
- Hemidesmosomes
- Keratin
- Collagen VII
What is the first-line treatment for dermatitis herpetiformis?
- Gluten-free diet
- Systemic corticosteroids
- Topical steroids
- Antibiotics
- UV light therapy
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |