Playlist
Show Playlist
Hide Playlist
Deep Venous Thrombosis
-
06 CVP Vein and Lymphatic Pathology.pdf
-
Reference List Pathology.pdf
-
Download Lecture Overview
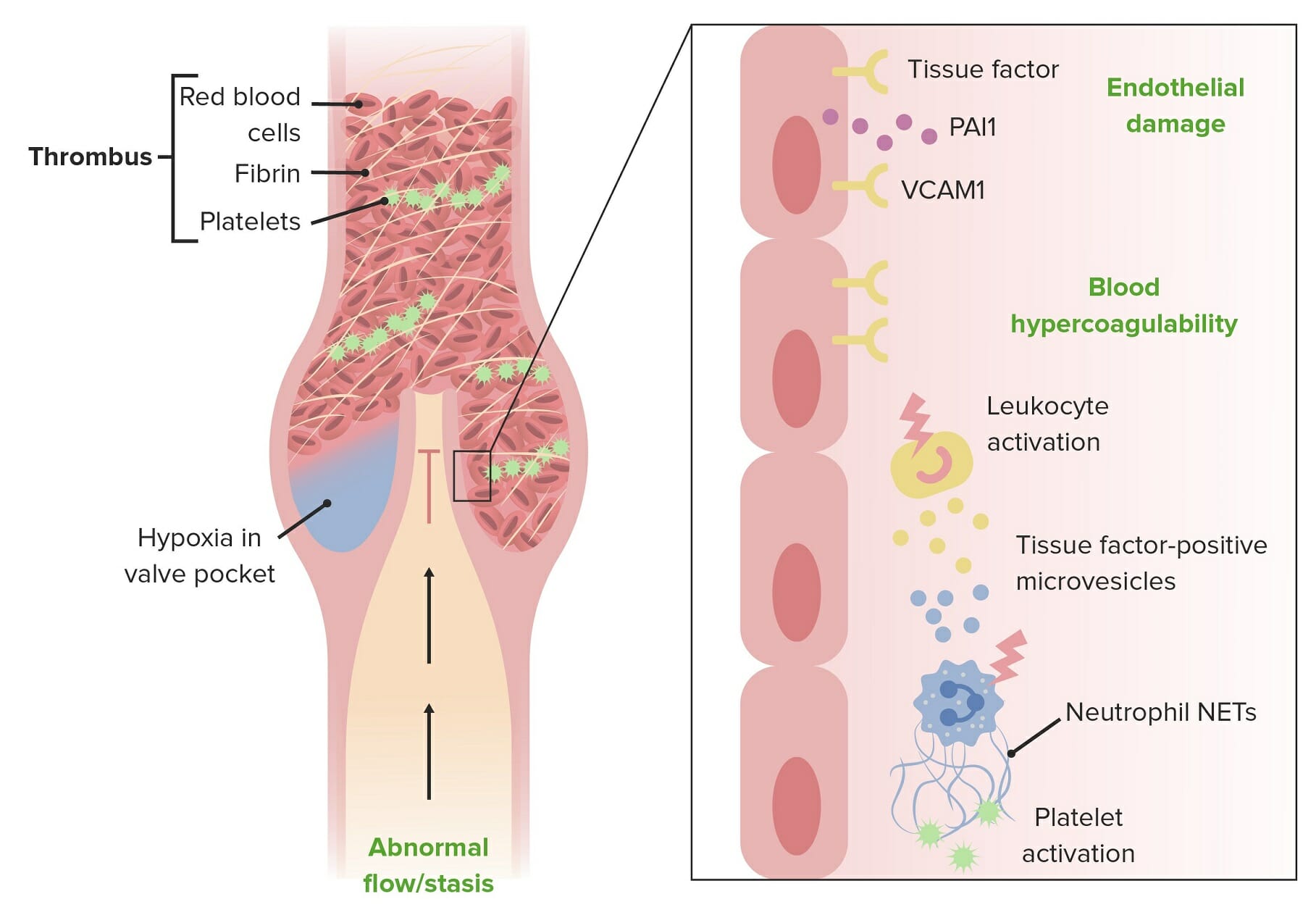
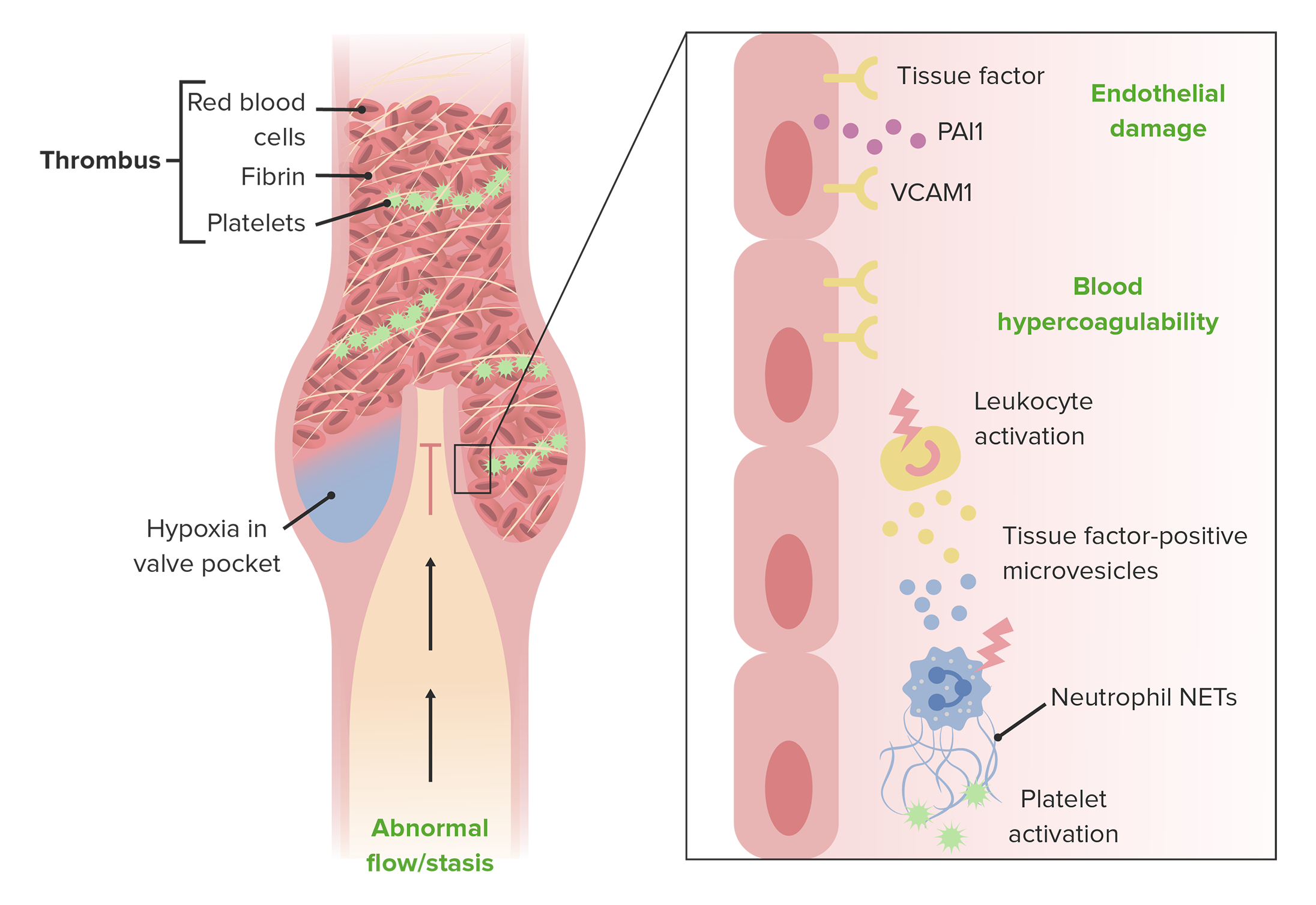
00:01 Okay. 00:02 So, that is varicose veins and a superficial lesion, now, we're talking about something deeper. 00:09 So, this is thrombophlebitis or phlebothrombosis. 00:13 You can use the terms pretty much interchangeably, thrombophlebitis means thrombosis with secondary, venous inflammation, thrombo-phlebitis. 00:24 Phlebothrombosis, basically means, venous thrombus, but if you do that, you're going to get inflammation. 00:31 So, you can use either one, really. 00:33 More than 90% of cases are caused by a deep leg vein thrombosis, so, this is not the superficial veins causing varicosities, these are deep leg veins. 00:44 There are other sites, besides the deep leg veins that are responsible or can have thrombophlebitis/phlebothrombosis. 00:51 The periprostatic venous plexus in males around the prostate, the pelvic venous plexus in females, or large veins in the skull, and in the dural sinuses, and also, you can have upper extremities, that are also involved in the same way that deep leg veins, can be involved. 01:08 So, you can have multiple sites where this occurs, but the vast, vast, vast majority, are going to be deep leg veins. 01:15 So, who's at risk men, moi, over the age of 50, moi, prolonged immobilization, no, I'm moving around, except I've been standing here now for about a half hour, and I'm at risk just by doing that. 01:30 But if you're bedridden, that will put you at risk of a deep venous thrombosis. 01:35 The post-operative state, where you also prolong demobilization, but post-operative, where you have, caused tissue injury, because of the surgical intervention, which activates a lot of tissue factor, which makes you hyper coagulable, so, the post-operative state is kind of a double whammy. 01:53 Congestive heart failure, because you are not getting good venous return, because the heart is not pumping effectively, and is therefore, not sucking blood through the venous circulation effectively, congestive heart failure, puts you at risk for a deep venous thrombosis. 02:07 Pregnancy. 02:09 Pregnancy because of a hypercoagulable state associated with pregnancy, but also, because there is a fetus that's lying on top of the inferior vena cava, and can potentially cause a relative stasis of the blood flow, coming out of the deep leg veins. 02:23 Obesity. 02:24 Kind of the same way that pregnancy does it, so, obesity can also be associated with a hypercoagulable state, but now you have this big body pannus, of adipose tissue, sitting on top of the inferior vena cava. 02:36 Oral contraceptive use, will cause a hypercoagulable state and we've discussed this in other talks, where we talked about thrombosis and hypercoagulability. 02:46 Malignancy because the elaboration of tissue factor and other factors made by tumors, metastatic tumor puts you at risk for hypercoagulability. 02:55 And then there are hereditary coagulopathies, where you have defects in some of the anticoagulant factors, or you overproduce some of the pro-coagulant factors. 03:04 So, all these put you at risk potentially for a deep venous thrombosis. 03:09 How does it manifest? So, there are some very classic, I say "Classic" signs and symptoms, the last line that's going to be on the slide is, “Most patients don't have the classic signs and symptoms.” So, you have to be thinking very carefully, in order to make the diagnosis in many cases. 03:26 So clearly, if I am not getting good blood flow out of an extremity, I’m going to have distal edema, makes sense right. 03:35 Because I’m now getting relative stasis, it loses more and more of its oxygen, so, you will see relative cyanosis, the skin the tissue looks bluer. 03:47 You can get superficial vein dilation, so, as the central vein becomes occluded, the peripheral veins then can become secondarily static. 03:56 You may have heat and redness as the blood settles and becomes and causes increased amount of venous occlusion. 04:06 You can have swelling of the extremity, mainly related to edema and tenderness, so, these are all kinds of features that you can see in deep venous thrombosis. 04:18 Finally, another variation on tenderness is “Frank pain,” it hurts. 04:23 Okay, so the final thing as I promised on this slide, many DVTs are asymptomatic, particularly if the patient is bedridden. 04:34 So, you have to think, very carefully, about the possibility this is occurring in your patient. 04:41 Roughly 50% of them have none of the classic findings. 04:46 So, how do we make the diagnosis? Well, if you're on physical exam, we can make the diagnosis by eliciting pain by pressing over the affected vein, that vein will be have a lot of static blood in it, may be dilated and it's going to be relatively hypoxic around it, by pressing on it, we will then activate the nerves, so, you can get pain by pressing on the affected area. 05:09 If you squeeze the calf muscles and you feel an engorged or distended cord, that's basically a deep vein, that has been filled up with blood, that's a good sign of a deep venous thrombosis, Again, these kind of signs, Again, these kind of signs, that you can elicit as a clinician, occur in less than 50% of patients, who have honest-to-goodness deep venous thrombosis. 05:34 So, what's the complication of not recognizing that it's there? Well, deep venous thrombosis, can lead to pulmonary embolism. 05:41 So, if that thrombus in a deep leg vein breaks off, and then it's carried by venous flow, the last big vessel that it will impinge on, impact into, is going to be the pulmonary artery. 05:55 So, you can have as a very serious and a very common complication, deep venous thrombosis is a PE, pulmonary embolism. 06:05 Results as shown there, from fragmentation detachment of the venous thrombus, and then it goes to the chest, and this gentleman is showing that, now you won't have pain per se, but you will have acute onset dyspnea, shortness of breath. 06:22 So, the very first manifestation of thrombophlebitis, may be that patient presenting with a pulmonary embolism, and you didn't suspect anything going on in the legs at all. 06:33 Depending on the size of the blood clot that goes, and the number of emboli, the outcome can range from nothing, it resolves spontaneously and there are no symptoms to death. 06:45 You can have a major saddle pulmonary embolism, that goes up to the main pulmonary artery, and catches into the bifurcation, into the right and left pulmonary arteries, no blood flow is getting through, and that can be a cause of death within minutes. 07:03 This is just showing you angiography, of a deep leg vein that has embolized into the pulmonary circulation. 07:11 So, the big circle in the middle of the top of the field, represents the aorta. 07:18 The kind of brighter image that's coming down to the right-hand side, into the green circle is a pulmonary artery, that is in fact the left pulmonary artery, and that should have contrast material, that goes out completely into the lungs. 07:35 Well, you can see on this particular image, in the middle of the green circle is that, all of that contrast abruptly stops right in the middle of the green circle, that is a pulmonary embolism, that has impacted into that vessel and no blood flow is getting distally, this patient is at risk of dying rather precipitously.
About the Lecture
The lecture Deep Venous Thrombosis by Richard Mitchell, MD, PhD is from the course Vein and Lymphatic Pathology.
Included Quiz Questions
Which of the following statements is correct concerning the risk factors of deep venous thrombosis?
- A postoperative state increases the risk.
- Obesity is not a risk factor.
- The risk decreases with advanced age.
- Pregnancy decreases the risk.
- Physical activity increases the risk.
Which of the following anatomic structures is most susceptible to deep vein thrombosis?
- Femoral vein
- Cephalic vein
- Basilic vein
- Superficial circumflex vein
Which of the following medications is associated with an increased risk of deep vein thrombosis?
- Oral contraceptive pills
- Beta-blockers
- Blood thinners
- Aspirin
- Erythromycin
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |