Playlist
Show Playlist
Hide Playlist
Coagulation Cascade
-
Slides Thrombus Formation Coagulation Cascade.pdf
-
Reference List Pathology.pdf
-
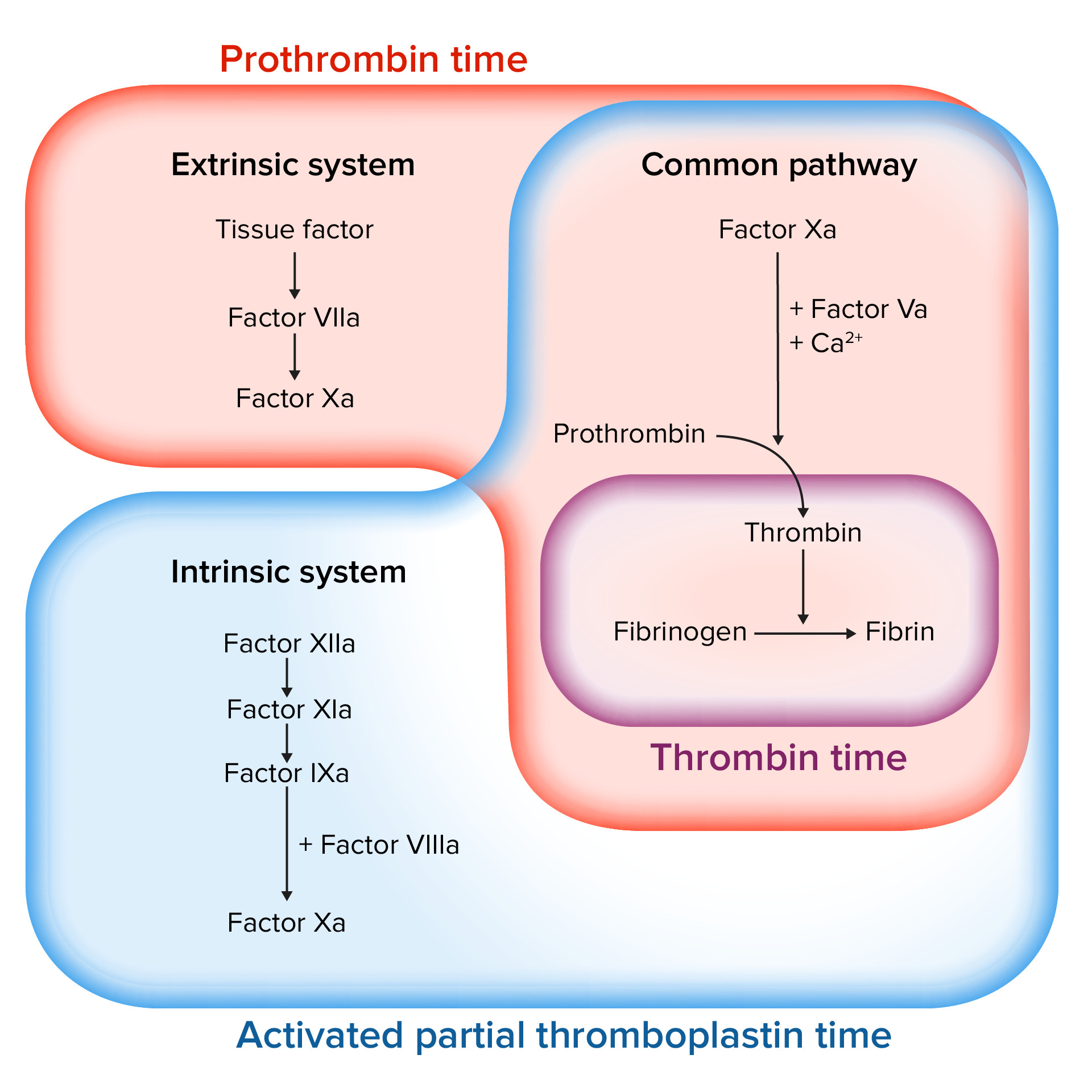
Download Lecture Overview
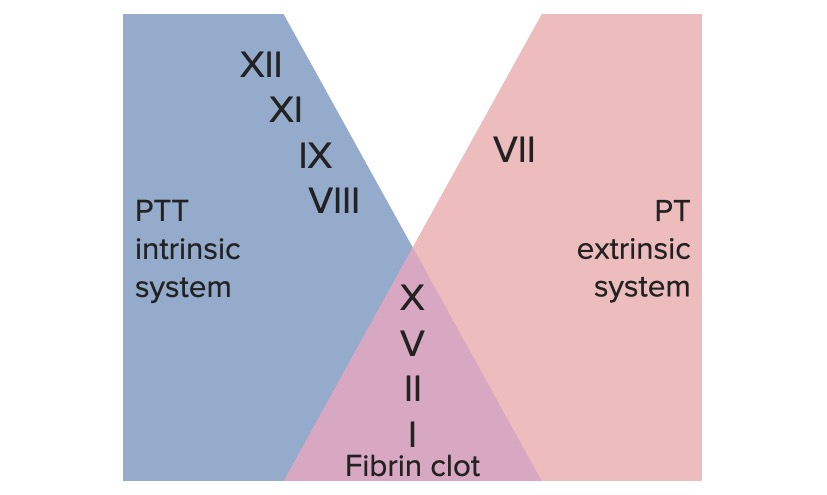
00:00 Welcome to the next session, the next steps in the coagulation process and thrombus formation. We've talked previously in an earlier session about platelets. Today we're going to emphasize the proteins that are synthesized elsewhere mainly in the liver and they are circulating within the bloodstream. They are indicated as little tiny multicolored dots there, the coagulation cascade and there are lots of factors. So all those different colors, it's a different factor. You don't necessarily need to remember all of the details but to get a sense of how this is put together, that's what we're here for. Okay, lots of details again go with the force, feel the big picture. So the coagulation cascade is broken into somewhat arbitrary intrinsic pathway and on the right hand side not yet coming up, the extrinsic pathway. The intrinsic pathway is activated by surfaces. So, remember how we exposed collagen and other extracellular matrix? Well, that's a surface. It turns out that platelets forming the primary and secondary hemostatic plug also provide a surface and that's how we're going to activate the intrinsic pathway factors. The intrinsic pathway factors are shown here. So, by general consensus, when we have an activated factor, they're all roman numerals by the way, but when we have an activated factor it's indicated with a lower case a. So, the initial activation of the intrinsic pathway by exposing surfaces is thru turning 12 into XIIa. It's a conformational change and then subsequently we're going to have a variety of proteolytic changes. And again, I apologize for the complexity of what you're about to see. There are multiple multiple factors that are involved. You're already getting a sense on the intrinsic side. They are numbered, not in the sequence. They are numbered based on when they were discovered. So, it turns out that factor I that's going to be all the way down on the lower right hand corner, was the first one that was discovered. Factor XII is one of the later ones to be discovered. We just have to go with it. 02:28 And they don't go necessarily even in appropriate sequence, although what is shown here XII to XIIa, XI to XIa, so then we missed X. It's IX to IXa. And then somehow we brought in factor VIIIa. Again, don’t get too embroiled in all of the various details. Keep in mind the bigger concepts. Okay. So, we have exposed the surface. We have activated XII to XIIa. 02:58 And then, it's going to, because of its conformational change, start proteolytically cleaving other factors. This allows us to get an amplification of the process because once we made a protease XIIa, it can chew up a lot of different XI to make XIa. And once we made a little bit of XIa, it can chew up a lot of IX to make IXa. So, we get a cascade, we get an amplification. 03:23 That's one of the other kind of features of the coagulation cascade. There is a common pathway. So in the middle here, again, on the right hand side still blacked out, you can't see it, there's going to be the extrinsic pathway. It's also going to fit in to this common pathway. Oh, suddenly, on the common pathway X has appeared. Okay, X becomes Xa and it interacts with a cofactor Va to get the next steps. And the next steps are that we're going to activate prothrombin, it turns out that prothrombin is factor II, also called prothrombin and it goes to IIa or thrombin by that proteolytic cleavage involving Xa and Va acting in concert. As we'll see, thrombin is an incredibly powerful kind of central component of the coagulation cascade. One of the major tricks that it does, one of the major roles that it has is in cleaving fibrinogen which turns out to be factor I. Remember we've said I is going to be in the lower right hand corner, here is I, we're going to convert fibrinogen to fibrin. So I to Ia and Ia is fibrin. And fibrin will polymerize to cement together all of those platelets. That's its main job. Okay, it turns out thrombin also acts on one of the very last factors to have been discovered in this whole cascade factor XIII. Factor XIII gets proteolytically cleaved by thrombin to XIIIa and XIIIa over a period of hours will cross link the fibrin. Why is this important? Well, this means that we've got a really stable plug. Okay, because we've now submitted it altogether with all these polymerized and cross-linked fibrin. The downside is that after 4 to 6 hours of XIIIa doing its thing, that fibrin clot, that fibrin cement holding the platelets together can no longer be degraded or broken down by the antithrombotic pathway such as tissue plasminogen activator. This has therapeutic implications. So that if I have a clot that has been there for 4 to 6 hours, it's no longer amenable to therapeutic clot busting. We can't add tPA and expect it to be effective. So that's what we tell patients, "If you're having a heart attack, get to the hospital as soon as possible because we can't do something for you." So again, just normal features of the coagulation cascade, they have therapeutic implications. Okay, so we've done the intrinsic pathway into the common pathway into the final kind of pathway where we're getting fibrinogen factor I to become factor Ia. Okay and then we crosslink it. Alright, that's the intrinsic pathway. Of course, there is an extrinsic pathway as promised and the extrinsic pathway is activated by exposure to tissue factor. Now tissue factor has a variety of names, I'm going to call it tissue factor for now, but it's also factor III. Hmm, how about that? It's also called thromboplastin. And the reason that I'm going to say those names again it's on later point is because some of the tests that we use use the old fashion names, but anyway, tissue factor. And tissue factor is there underneath the endothelium all the time but we don't see it until we get endothelial injury and now we're going to activate the extrinsic pathway. The extrinsic pathway starts with tissue factor being exposed and then when factor VII sees that tissue factor, factor VII again is in the circulation, it will undergo confirmation change to factor VIIa. And the combination of VIIa and tissue factor together will then get us into the common pathway and we're often running. So, the rest of it is kind of what we've talked about previously. Okay, another important point because this is, well, this is how we drive the coagulation cascade or how we can potentially block the coagulation cascade. So a number of the various steps absolutely critically require phospholipid, so a negatively charged phospholipid on a membrane surface, and calcium. And you can see those. So going from VII to VIIa requires that I have phospholipid and calcium. So merely X to Xa, IX to IXa and prothrombin to thrombin. All require that I have a surface or I can have phospholipid, a negatively charged thing, holding calcium which will then hold those various factors so that I can get the enzymatic catabolism. Okay, so these are very important kind of control checkpoints. Okay, so what's in a name? Why do we call it the intrinsic pathway and the extrinsic pathway? Well, in the intrinsic pathway, it's basically something that's intrinsic within blood that activates factor XII. It turns out that it's probably, again remember it was a surface, it's probably negatively charged polyphosphate that's released on to the surface by activated platelet. Okay, so it's something that was intrinsic to the blood and it turned out to be this polyphosphate from platelet. The extrinsic pathway, so remember it starts with tissue factor. Tissue factor is synthesized by activated endothelial cells, but it's also normally present only on the cells that sit below the endothelium such as fibroblast or smooth muscle cells and it's therefore extrinsic to the blood. Now you know. 09:17 Hopefully that helps clarify in your mind how these various pathways kind of intersect and why they are named. So what's really going on in coagulation.
About the Lecture
The lecture Coagulation Cascade by Richard Mitchell, MD, PhD is from the course Hemostasis.
Included Quiz Questions
Where are the factors of the coagulation cascade produced?
- Liver
- Spleen
- Pancreas
- Thyroid
- Kidneys
How many clotting factors are there?
- 13
- 10
- 6
- 8
- 16
What factor is involved in the common pathway?
- Factor X
- Factor XII
- Factor XIII
- Factor VII
- Factor IV
What factor activates the extrinsic pathway?
- Tissue factor
- Factor I
- Factor II
- Factor IV
- Factor IX
What is the end product of the coagulation cascade?
- Fibrin
- Phospholipid
- Prothrombin
- Fibrinogen
- Thrombin
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
2 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
Good explanation in short time and simple to understand the whole concept
Highlights key points and is super easy to follow - spent hours trying to understand the same concepts when reading the textbook