Playlist
Show Playlist
Hide Playlist
Celiac Disease: Pathophysiology
-
Slides GIP Celiac Disease.pdf
-
Reference List Pathology.pdf
-
Download Lecture Overview
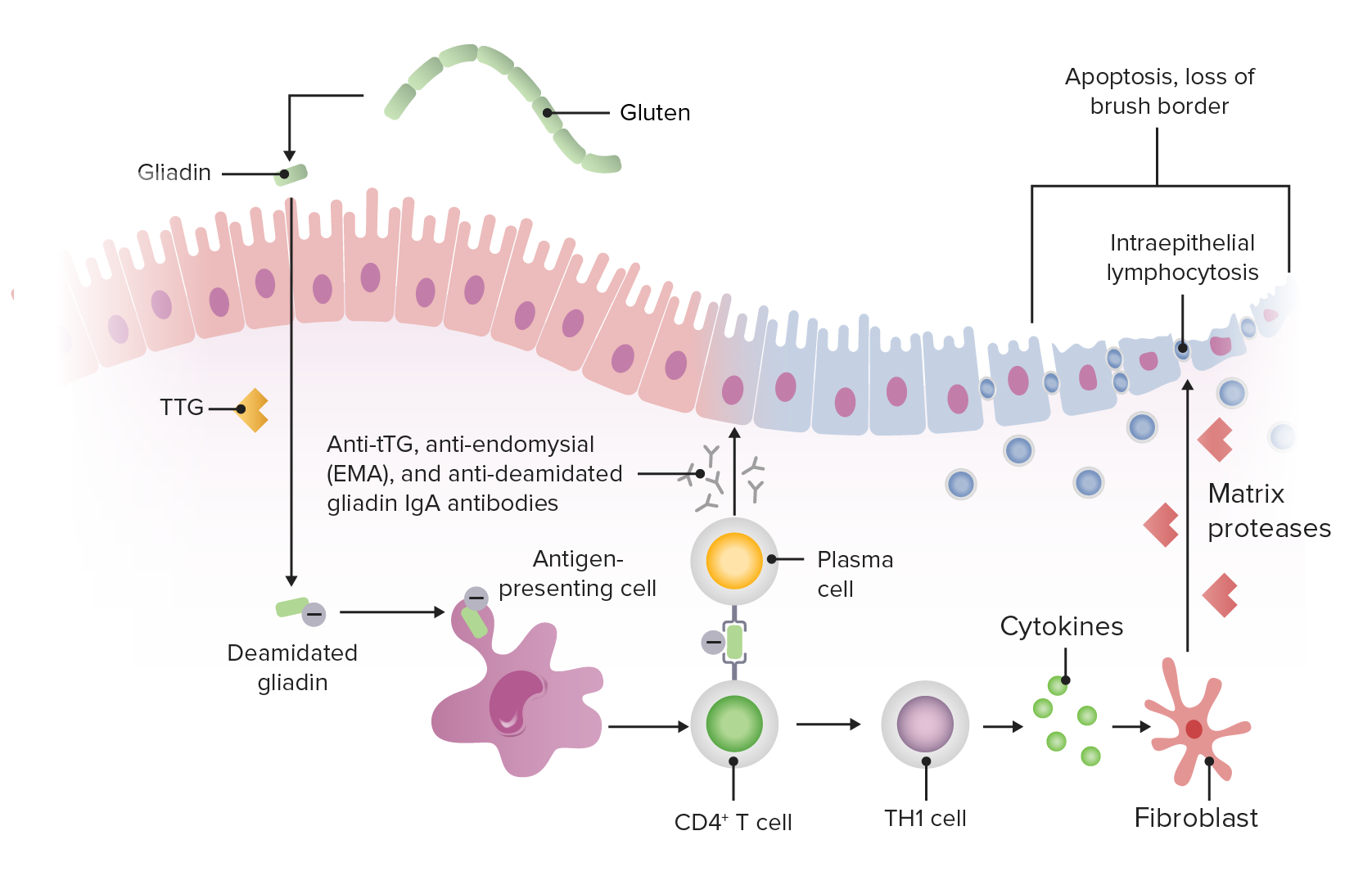
00:01 Welcome. 00:02 With this talk, we're going to cover a very important entity called Celiac Disease, also known as celiac sprue or gluten-sensitive enteropathy. 00:11 This is a malabsorption syndrome. 00:13 And it's associated with certain dietary ingestions that we'll talk about. 00:18 On the left hand side is the normal small bowel epithelium, a representation with very tall villi, relatively short crypts, not much inflammation within the lamina propria. 00:32 All of those tall villi give you a lot of absorptive surface area which is what the small bowel needs. 00:38 On the right hand side, we have celiac disease. 00:41 We still have crypts, but we have lost a lot of the absorptive epithelium on the villi. 00:48 And this is going to obviously then give you malabsorption. 00:53 Let's see how common this is and who gets it, and then we'll get into why they get it. 00:59 For variety of mostly genetic reasons, it is primarily a disease of whites of the Northern European descent. 01:08 The incidence is reasonably high, 1:70 or to 1:300 is the estimated incidence of this disorder. 01:18 Women tend to get it more frequently than men and it may have an hormonal component. 01:24 There is a bimodal age distribution. 01:27 Individuals who are prone to this may experience the first manifestations as early as one year of life. 01:34 But more typically, this presents in the third to fourth decades of life. 01:41 As I've already intimated, this has a relatively strong genetic component, and almost everyone who has celiac disease will have certain histocompatibility molecules in their genome, HLA DR3-DQ2. 01:57 So this is a type 2 major histocompatibility complex molecule or HLA-DR4-DQ8. 02:05 I don't think you need to remember the exact HLA types, but do know that there is an association. 02:13 And clearly with that strong genetic component, there's a very strong positive family history. 02:18 And that's seen in upwards of 10% to 15% of patients. 02:23 Getting into the pathophysiology. 02:26 We know now that this is environmentally triggered, specifically by gliadin, which is a component of gluten found in a variety of grains, wheat, barley and rye. 02:37 So if you are so unfortunate to have this disorder, beer is kind of off your dietary list. 02:44 There are gluten free beers but they are not made with the same barley components that we would normally see in a typical beer, for example. 02:52 And as I've already said, there are certain genetic elements. 02:56 So what this is, is an environmentally driven autoimmune disease. 03:02 Let's try to understand that. 03:04 This is fundamentally an autoimmune disease driven by an external antigen. 03:10 It is the delayed type (type 4) hypersensitivity reaction. 03:13 If you want to review what that was about, you can hear one of my talks earlier in the entire Lecturio files on immune-mediated injury. 03:22 Lecturio files on immune-mediated injury. 03:24 There are autoantibodies that are generated during the course of the immunologic response. 03:30 These are more biomarkers rather than probably pathologic. 03:37 The process by which this happens, so we are talking about gluten in certain grains, this is ingested, the gluten is partially digested to smaller peptides called the gliadins. 03:49 And those gliadin peptides are translocated across the epithelium into the lamina propria. 03:56 In that location, there are tissue transglutaminases abbreviated TTG that will deamidate the gliadin. 04:05 It's that the deamidated form of the gliadin that is then picked up by antigen presenting cells, dendritic cells, or macrophages that will then present it to CD4+ T cells, helper T cells and you see that presentation process. 04:19 This is where that HLA comes in, because you have to have a specific HLA that will bind to the deamidated gliadins and not every HLA that exists in the human population will do so. 04:32 However, now, once we have the antigen presenting cell presenting to the helper T cell, that helper T cell will undergo differentiation into a Th1 type T cell and it will make a variety of inflammatory mediators. 04:46 Those inflammatory mediators will recruit macrophages and themselves will be proinflammatory and we will get an intraepithelial lymphocytosis, a combination of the cytokines and inflammatory cells will cause the epithelium lining the small bowel to become relatively atrophic. 05:08 We will lose those beautiful villi, so we lose absorptive surface area. 05:12 And we may even have frank apoptosis, that occurs as a result of the activity of the macrophages, the T cells and the cytokines. 05:22 So, we have apoptosis, we will lose the brush border, so we'll have major simplification of the epithelium and we lose absorptive surface area. 05:32 Voila, then we have malabsorption. 05:35 And we will not be able to absorb all those nutrients that are sitting in the lumen. 05:40 I will say in a moment, we will get further downstream and the bacteria that are waiting, there are just only too happy to ferment those nutrients that aren't being absorbed. 05:50 At the same time, the T cell and the antigen presenting cell are processing the antigen. 05:56 The T cell will drive B cells into terminal differentiation to make plasma cells that will have a variety of auto antibodies capable of being synthesized. 06:07 So we'll have the anti tissue transglutaminase. 06:10 We will have antiendomysial . 06:12 antibodies specifically against the gliadin components. 06:13 against the gliadin components. 06:15 And in some of the cases, these are IgA, they're not IgG, which are you would typically think of, but they're IgA. 06:22 And the IgA antibodies are going to be important for some of the more systemic manifestations that we'll see associated with celiac disease. 06:31 Celiac disease is associated with a variety of systemic manifestations. 06:36 Dermatitis herpetiformis is one that is actually reasonably common. 06:41 It's a blistering intensely itchy or pruritic rash. 06:44 And what it is associated with is IgA deposition at the dermal epidermal junction. 06:50 And we'll see little tiny microabscesses associated that with blistering. 06:57 Because of the ongoing inflammation in the small bowel, especially with persistent exposure to glutens and then the gliadens. 07:06 You are at increased risk of celiac disease, the developing a small bowel MALT or mucosal associated lymphoid tissue lymphoma. 07:16 And because of the association of the HLA, there may be other autoimmune diseases that can occur side by side with celiac disease not necessarily directly caused by celiac disease. 07:29 But have a epidemiologic association because of the the various HLA and these include some forms of thyroiditis, and even type 1 diabetes.
About the Lecture
The lecture Celiac Disease: Pathophysiology by Richard Mitchell, MD, PhD is from the course Small and Large Intestines Disorders.
Included Quiz Questions
For individuals with celiac disease, what percentage of patients have a positive family history?
- 15%
- 30%
- 50%
- 55%
- 5%
Which of the following is NOT associated with celiac disease?
- Type 2 hypersensitivity reaction
- Gliadin
- HLA-DR4-DQ8
- Type 4 hypersensitivity reaction
- IgA anti-tissue transglutaminase
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
3 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
Thank you doctor for the fasinating lecture I really love your way of teaching,and organization
2 customer reviews without text
2 user review without text