Playlist
Show Playlist
Hide Playlist
Cataracts
-
Slides OP Diseases of Lens Vitreous Body.pdf
-
Reference List Pathology.pdf
-
Download Lecture Overview
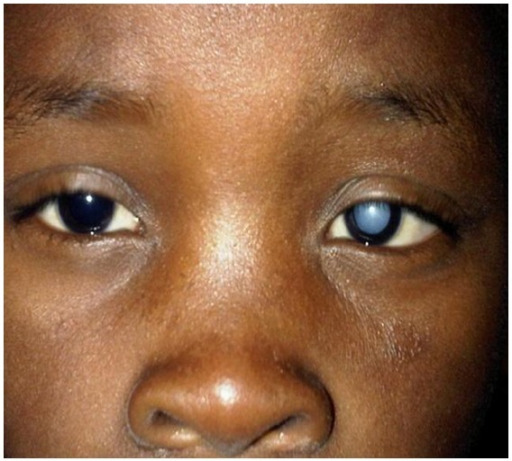
00:00 Welcome back. We're going to look now at some additional pathology specifically involving the lens. This is going to be mostly about cataracts. And then also diseases of the vitreous body and that's mostly infection, endophthalmitis. So with that preface, let's go. Again, just to orient you, here are the structures we're going to be looking at; the lens and the vitreous body for the most part. And the major pathology involving just the lens structure itself are cataracts. So, what is a cataract? And basically this is an opacity of the lens itself that disrupts the light projecting on to the retina. And if you can imagine this, if you had a lens in front of your eye that was not entirely translucent, had some opacity to it, you would be seeing kind of blurred vision or obscured vision. Remember that the lens is composed of, on the anterior surface which is relatively flat relative to the more concave posterior surface of the lens, there are a single layer of cuboidal epithelial cells that are going to continue to grow throughout life and then they kick out their nuclei and they kick out their organelles and those cells become oriented fibrils that form the lens. So it's basically the remnants of what used to be the epithelial cells on the surface. They need to be perfectly aligned so that they get appropriate refraction of the light that's coming through, but they also need to be perfectly clear. And if there are any changes that occur in there, protein coagulation, cross-linking, deposition of materials, that's going to make it opaque, and that's going to be a cataract. Pretty straightforward except it can be pretty devastating. Cataracts will affect all age groups, but is going to be mostly in the more geriatric population. Yes, we'll talk about some pediatric causes in a minute, but mostly this is going to be an age-related accumulation of opacity and very common in the older population. What are the signs and symptoms? Again, we have this lens and now it's become cloudy. So the vision is going to be blurry. 02:28 We're going to get abnormal defraction of light, so it won't be as sharp. There will be nocturnal glare sensitivity. Again because of the abnormal defraction of light, light coming in instead of being a nice pinpoint light, say from that light in streetlight that's on the picture, that ends up being defracted into bunch of different directions so it looks like it's a starburst. 02:52 There will frequently also, because of the abnormal defraction, be a colored halo around lights. And because of the abnormal defraction things will look double, triple vision, look fuzzy overall. So, diplopia, double vision; polyopia which is going to be kind of multiple images, fuzzy. Because of the opacity, we're not getting good light transmission through this, there's going to be reduced perception of color. And because of now the lens is no longer with its normal refractile properties, we're not going to be focusing appropriately on the macula. So there will be diminished visual acuity. And finally, if we're looking at the person, leukocoria occurs. So leukos root word meaning white, korea eye and right here we are seeing the whiteness through the pupil of the lens because it's opaque. So the etiology. Adults, as I said, most of the time most cataracts are going to be age related and with a very high prevalence in those who are older than 80 years of age, greater than 90% of geriatric patients will have some degree of cataract. Systemic disease can also influence this and one of the classic ones is diabetes mellitus. Chronic hyperglycemia bathing the lens will cause nonenzymatic glycation and cross-linking. And that cross-linking basically leads to a precipitation of all those fibrils no longer oriented becomes opaque. Various toxins can also influence the cross-linking and the normal aggregation and orientation of those fibers within the lens and smoking and alcohol, other drugs can potentially impact that. UV light or infrared exposure can also drive this and this is probably because of the energy that comes in is causing cross-linking of proteins. So, for example there is a much higher incidence at much earlier ages of cataracts in people who live in Nepal, for example, on the top of the world because they have much greater exposure to UV light. Inflammation, so if we have inflammation involving the ___ axillary body, the iris, the choroid that can also have consequences related to now degradation in protein, cross-linking within the lens. Trauma or previous surgery will obviously lead to the inflammation that can also affect the lens. And then medications; corticosteroids and miotics, interestingly enough drugs that affect the ability of the iris to open and close. In children, there can be congenital cataracts due to abnormal cellular orientation coming off that anterior cuboidal epithelium and so trisomy such as 13, 18, and 21; Turner syndrome; some of the metabolic disorders can all cause congenital cataracts that are present basically at birth. And then you can have acquired things in children in the same way that you can for adults; inflammation, infections particularly those in the mother, trauma or surgery, type 1 diabetes poorly controlled, or radiation therapy. If kids are getting therapy say for a retinoblastoma, that radiation can affect the ability of those cuboidal epithelium in the lens to appropriately orient. What do we see on fundoscopic exam? It's pretty straightforward. Gee, if I have a lens that completely opaque, if I look in there through the pupil, it's going to look opaque. So the leukocoria that we had seen with that kind of light coming over the whiteness in the pupil, this is the reflection if we look in on a fundoscopic exam. In most cases, the cataracts are typically not this dense. This would be a severe end stage, but this is just, you get the picture. So how do we treat this? It's a surgical intervention. There really isn't a way other than replacing the lens and putting in a new plastic implant and this can be done as a single outpatient procedure, doesn't necessarily require that you'd be admitted. And we remove the old opaque lens and we're demonstrating that in the top 3 panels, and then we put in a new plastic lens that is absolutely clear and it will do much the same thing that the lens did prior. 07:47 There are complications related to this. So, we're in there mocking around, there's always a possibility for infection. So endophthalmitis is a potential complication. We don't always numb most of the time, the ophthalmologist will get it perfectly positioned but if it's not you may have lens that's a little bit off the side, a little bit medial, a little bit up, or a little bit down and there will not be the appropriate refraction of light so it's heating the macula. So there may be slight malposition that may require secondary intervention. And then, because we are changing the intraocular pressure in doing this, there is a little bit of tagging that's going on to pull out the old lens and put in the new lens and in doing that we may induce a tear in the retina. So a rhegmatogenous retinal detachment.
About the Lecture
The lecture Cataracts by Richard Mitchell, MD, PhD is from the course Posterior Segment Eye Diseases.
Included Quiz Questions
What cells are present in the epithelium of the lens?
- Cuboidal
- Columnar
- Squamous
- Polypoid
- Ciliated
What are characteristic signs and symptoms in a patient with cataracts?
- Polyopia and leukocoria
- Myopia and anisocoria
- Hyperopia and leukocoria
- Miosis and anisocoria
- Mydriasis and leukocoria
What syndrome is associated with cataracts?
- Turner syndrome
- Horner syndrome
- Marfan syndrome
- Pierre Robin syndrome
- Treacher Collins syndrome
What can be a postoperative complication of cataract surgery?
- Endophthalmitis
- Sepsis
- Retinitis
- Iritis
- Blepharitis
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |