Playlist
Show Playlist
Hide Playlist
Case: 45-year-old Man Presenting with a Stroke – Management
-
Slides Management of Acute Ischemic Stroke.pdf
-
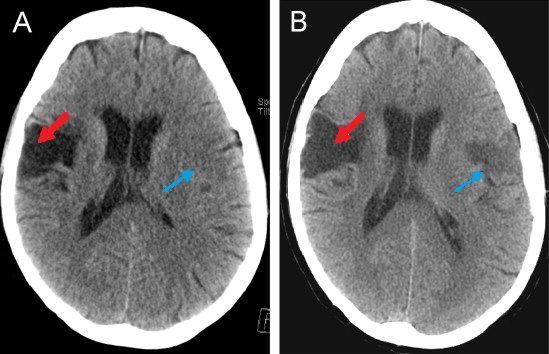
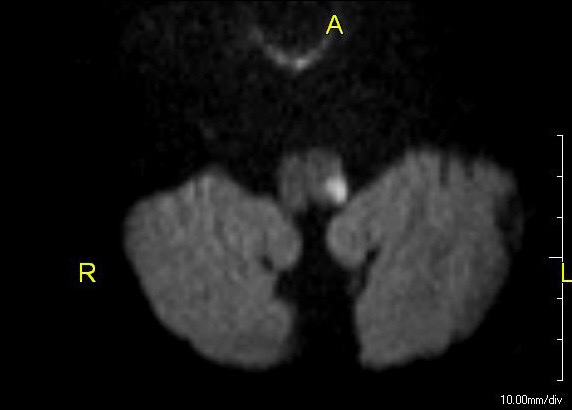
Download Lecture Overview
00:01 In this lecture, we'll talk about the emergent management of an acute ischemic stroke. 00:07 And let's start with a case. 00:09 This is a 45-year old man with a history of hypertension, hyperlipidemia and diabetes who presents for right-sided weakness and speech dysfunction. 00:18 The patient went to bed last night in normal health. 00:21 When he awoke this morning his wife says that he did not have any symptoms and was able to speak normally. 00:27 At around 10:30 AM, he went into his shed to work in a shop. 00:32 At 11:30 AM, his wife found him in the shed on the ground, without the ability to move his right side and mumbling. 00:40 EMS was called and he was brought to the Emergency Department where he remains weak and mumbling. 00:46 On examination, he has right hemiplegia involving the arm/leg as well as a right facial droop. 00:53 He's unable to speak, he mumbles incoherently, and is able to follow a simple command to open and close the eyes. 01:00 So what's the diagnosis? And what's your management? Well, as we've learned with going through stroke cases, the first and most important point is to define the symptom onset. 01:13 When we think about when something started, we may say that this started around 11:30 AM. 01:19 But with stroke, it's important to define the last known normal, so symptom onset was not 11:30 AM. 01:26 The last known normal was 10:30 AM. 01:31 Then we look at how the the symptoms evolved over time. 01:34 We see for this patient, he presents as we would expect a stroke with an acute onset of a fixed deficit or an acute fixed deficit. 01:43 For this patient, he has right hemiplegia involving arm, face and leg. 01:48 And so in terms of localization, this is a stroke that's affecting either the pons or something more proximally, more cranially. 01:59 And in terms of localization, there are two important localizing findings for this patient. 02:04 One is the right hemiplegia, which localizes or lateralizes the symptoms to the left side. 02:10 And then the second is the patient's aphasia, which really points us to the dominant frontotemporal region. 02:19 And then importantly, the wild card point in this case, which cannot be under emphasized is that the last known normal was 10:30 AM. 02:29 This is someone who is presenting with symptoms of an acute ischemic stroke within what sounds like about an hour from his last known normal. 02:37 And this is within a time window for acute and emergent intervention. 02:42 So what is the next step in your management? Would you do an MRI of the brain, evaluate for tPA or tissue plasminogen activator treatment, start aspirin or perform an EKG? Well, EKG is never a bad thing to do, but it's not the next step in management for this patient. 03:03 Paroxysmal AFib is a potential cause of a large vessel occlusion. 03:07 And this patient symptoms, the territory of brain that's involved is quite large. 03:13 He has hemibody symptoms and a dense aphasia. 03:16 So we're worried about a large vessel stroke, and the etiology may be Paroxysmal AFib. 03:21 But that's not the first thing we'll do for this patient. 03:25 We could think about aspirin, and aspirin is a good idea for patients who are suffering a cerebrovascular event. 03:31 But again, it's not the next step or the best next step for managing this patient who presents within a window of time where we can intervene. 03:41 MRI of the brain will be done for this patient. 03:44 We want to evaluate whether he's had a stroke and really define the extent of that stroke. 03:50 But again, this patient has presented within a window of opportunity for an acute intervention. 03:55 And so MRI of the brain is not needed to diagnose the stroke. 03:59 Clinically, this patient meets criteria for an ischemic stroke. 04:02 And so the best intervention and the best next step in management is to evaluate the patient for tPA. 04:09 The patient presents with the last known normal within 1 hour of symptom onset. 04:14 His symptoms are consistent with a left MCA syndrome. 04:17 We need a CT of the head to evaluate for hemorrhagic stroke and rule out a hemorrhagic stroke. 04:23 And then we would consider and proceed with the intervention with tPA administration.
About the Lecture
The lecture Case: 45-year-old Man Presenting with a Stroke – Management by Roy Strowd, MD is from the course Stroke and Intracranial Hemorrhage.
Included Quiz Questions
Which intervention for acute ischemic stroke is the most time-sensitive?
- Non-contrast CT to check for hemorrhage before giving tPA
- MRI to evaluate the extent of the stroke
- Aspirin to decrease platelet adhesion
- ECG to check for atrial fibrillation
- Lab tests to evaluate for coagulopathy
What cerebral blood vessel is likely involved in a patient who presents with right-sided hemiplegia and expressive aphasia?
- Left middle cerebral artery
- Right middle cerebral artery
- Right anterior cerebral artery
- Left anterior cerebral artery
- Left posterior cerebral artery
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |