Playlist
Show Playlist
Hide Playlist
Acne: Pathophysiology
-
Reference List Pathology.pdf
-
Slides Acne Pathophysiology Dermatopathology.pdf
-
Download Lecture Overview
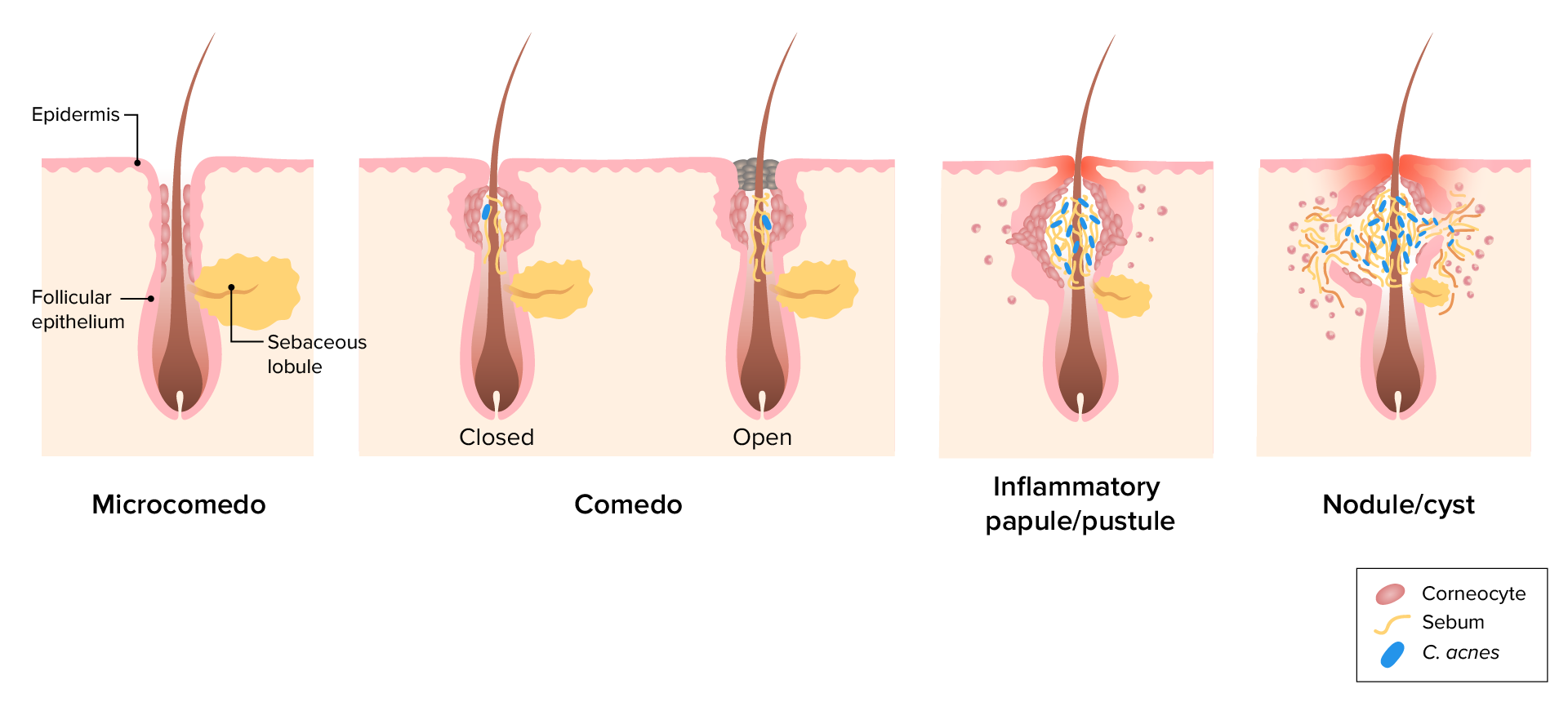
00:01 Welcome. In this talk, we're going to discuss the bane of every teenager's existence, that is to say, acne, otherwise known as pimples or the medically accurate term zits. 00:15 So acne, the definition that's provided here sounds a lot more erudite than what it is, but it really is inflammation of the skin. 00:22 Yep. Caused by follicular hyperkeratinization. 00:25 So we're actually going to plug up the pores around hair shafts with too much keratin or too many cells. 00:32 Behind that we're going to make too much sebum production by the sebaceous glands. And then the follicles have become or will become colonized by a specific form of bacteria on the skin, a normal commensal called Cutibacterium acnes. 00:49 And that's going to give us the constellation known as zits or acne. 00:53 So let's talk about the epidemiology of acne. 00:58 It is far and away the most common skin disease. 01:02 And in fact, statistics say that 80% of people in life will experience this at one point or another. 01:09 I actually think it's probably higher than that, and wonder how 20% of people got away without having ever having an acne pimple. Boys are more commonly affected in adolescence. 01:19 That's because as they enter through puberty, the testosterone and especially dihydrotestosterone metabolites will increase the sebaceous gland proliferation and also the production of sebum, so that's why they are more prone. 01:35 Women tend to be more affected as adults, and some of the mechanisms for that may include um, estrogen, estrogenic effects, as well as makeup or other occlusive sorts of factors. In terms of the etiology, we know quite a bit about how this happens. 01:56 So there is a genetic predisposition that um is listed here as a heritability of 50 to 90%. 02:04 I actually think because it is so common overall, that just being a human being and walking on the planet is your genetic risk of developing acne. The other important component of this is the bacterium that's responsible for driving this. 02:19 And this is Cutibacterium acnes. 02:22 This is a normal skin commensal that is going to be a very important player in the pathogenesis. 02:31 It was formerly called a Propionibacterium acnes. 02:35 But we've changed the name. 02:37 That whoever changed it was above my pay grade. 02:40 But it's also easier for us to say Cutibacterium acnes. 02:44 Aggravating factors. Overall, there is hormonal variation. 02:47 We've already talked about young men going through puberty where we're going to activate the sebaceous glands. Similar things will happen depending on the hormonal milieu during the menstrual cycle or during pregnancy. 02:59 And there's definitely hormonal variations that occur as a result of polycystic ovarian syndrome. 03:06 Mechanical occlusions over focal areas of the skin will also give rise to this. 03:11 So if you wear an underwire bra, headbands, shoulder pads, cosmetics, even stress. 03:17 And that's not a mechanical occlusion, but can be an aggravating factor. 03:22 Certain medications because they drive the production of sebum or they change, they change the differentiation, the maturation of keratinocytes within the skin will have an effect. 03:34 And diet in dairy is mentioned here because there can be hormonal components in the milk, although that more and more that is not the case. And high glycemic index foods, because that changes the local metabolic milieu and makes it better for the bacterium to grow. So the pathophysiology of this overall we're looking at semi-normal skin. 04:01 This actually identified on this slide as a microcomedo . 04:05 So this is the beginning lesion that happens kind of at the nascent stages of acne. So we have our hair shaft with our follicular epithelium around it. 04:14 And the sebaceous gland that is dumping its contents onto the hair shaft to get out to the skin. 04:21 Okay. That's all normal. 04:22 You will note that just north just above the sebaceous gland, there are some kind of indentations that are identified as corneocytes, that in fact is an early accummulation of corneocytes You can't see this, particularly extrinsically, but this is the earliest microcomedo stage in driving acne. So we're beginning to get a abnormal accumulation. 04:46 And you can imagine that if those keratinocytes that are above the spacious lobule proliferate too much, we're going to block the outflow of the sebaceous gland. All of that sebum is not going to be able to get out to the surface. 05:00 That's the next stage. 05:02 A full comedo stage now, which we can see on the surface of the skin. 05:07 And we'll see that in examples of that in a moment. 05:10 But this now we've had so much proliferation, we have effectively blocked the outflow of the sebum from the sebaceous gland at the same time as we're kind of blocking that outflow, we have trapped surface cutibacterium that are now in that environment where it's very rich, nutritionally speaking, and they're going to be able to kind of grow and have a very happy life. 05:35 And so with a complete blockage, training along the hair shaft, the comedo, then we have an environment that is ripe for developing the pustular phase of acne. 05:48 In that environment, there is no outflow of the sebaceous content to the sebum and the bacteria in there having a great time proliferating and eating all of the nutrients that are there. This leads us to the inflammatory papule or pustule. 06:06 So we have had a massive expansion of the bacterial population. 06:10 Those bacteria are making a variety of proteases that are going to break down basement membrane and other collagenous extracellular matrix structures. 06:19 They are also going to be eliciting an inflammatory response, appropriately, they are bacteria. 06:25 And who would respond. 06:26 Neutrophils. And so we're going to have now a battle of the bacteria expanding and the host innate immune response neutrophils and macrophages attacking back. 06:38 That battle between the two the bacteria and the innate inflammatory response is going to give rise to the acne lesions that are so traumatizing to young adults. 06:50 So here we've had now further erosion of the because of the activity not only of the bacteria proteases, but also the proteases and the reactive oxygen species derived from the inflammatory response. And we're into an inflammatory nodule and even vocally, a cyst. So the pathogenic kind of stages is that we're going to initially have follicular hyperkeratinization, okay. That's those are the early microcomedo stage where we're starting to have proliferation of the epithelium that's around the hair shaft, but it's not yet occlusive. 07:27 And we're also going to have the sebaceous glands doing their job sometimes in response to inflammation or stress or whatever. 07:35 But they're going to be making sebum. 07:37 Provided that we have open access, we're okay. 07:41 But as we have increasing amount of keratinization and then we develop that comedo that blocks the outflow, trapping the bacteria underneath, we're going to give rise to inflammation. So that's kind of the process.
About the Lecture
The lecture Acne: Pathophysiology by Richard Mitchell, MD, PhD is from the course Inflammatory Lesions of the Skin.
Included Quiz Questions
What percentage of people will experience acne during their lifetime?
- 80%
- 50%
- 30%
- 65%
- 95%
What is the earliest stage in acne development?
- Microcomedo formation
- Bacterial colonization
- Pustule formation
- Inflammatory nodule
- Cyst development
Which bacterium plays a key role in acne pathogenesis?
- Cutibacterium acnes
- Staphylococcus aureus
- Streptococcus pyogenes
- Malassezia furfur
- Pseudomonas aeruginosa
Which pathologic condition can aggravate acne in adults?
- Polycystic ovarian syndrome
- Hypothyroidism
- Addison's disease
- Type 1 diabetes
- Graves' disease
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |