Playlist
Show Playlist
Hide Playlist
Acne: Diagnosis and Management
-
Reference List Pathology.pdf
-
Slides Acne Diagnosis Management Dermatopathology.pdf
-
Download Lecture Overview
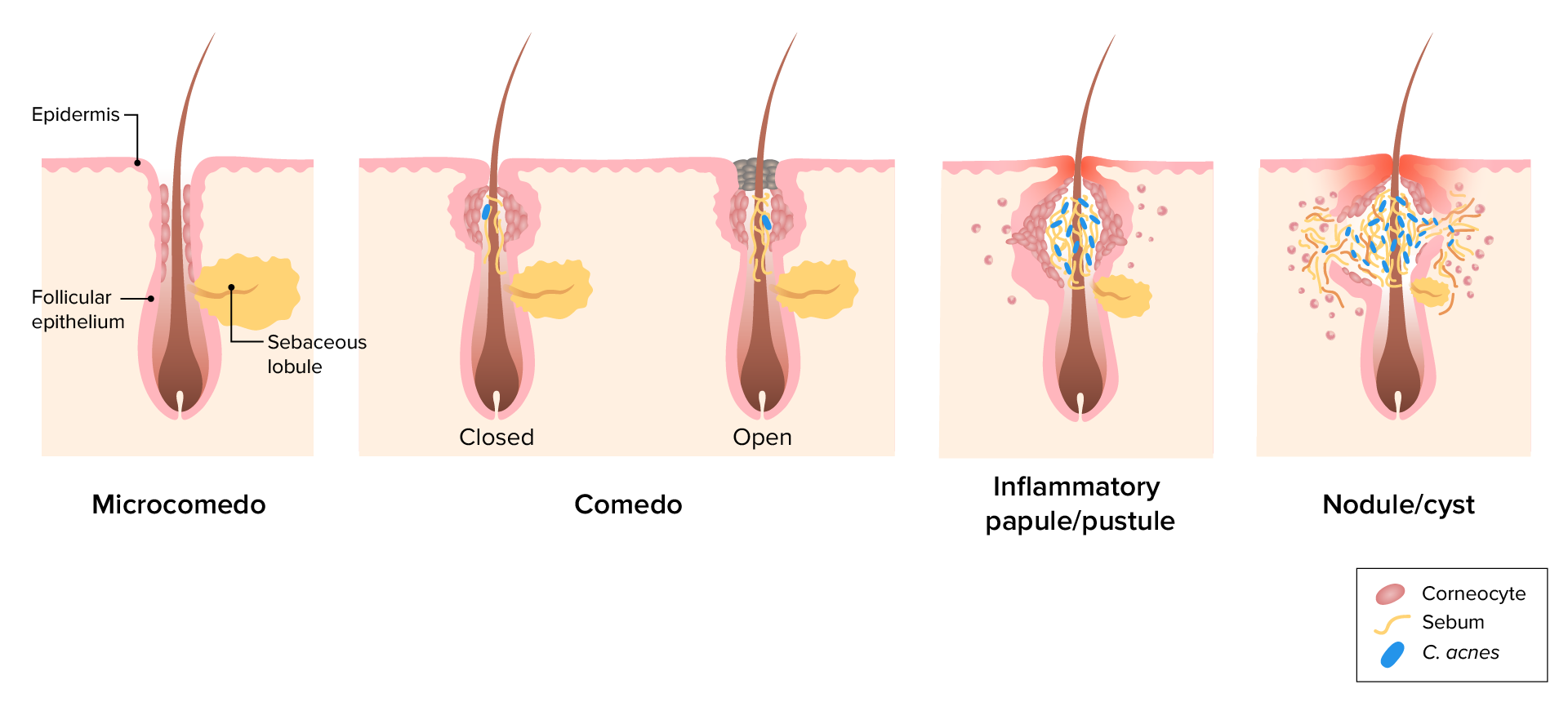
00:01 The clinical manifestations. Well you're probably well aware of these having gone through puberty yourself. 00:07 So there're very early noninflammatory acne. 00:10 Those are the comedones. 00:12 They're the hyperkeratotic plug that is black or darkened because of the oxidation of the lipids. 00:18 It's in the kind of the lower portion of the follicular infundibulum. 00:22 So basically right there at the neck as the hair shaft comes out. 00:25 There are open comedones and closed comedones. 00:27 The open comedones you still get drainage, the closed ones you don't. 00:32 Once you don't, then you have inflammatory acne. 00:35 That's going to give rise to those other manifestations with increasing bacterial burden and increasing innate inflammatory response. 00:43 So noninflammatory acne, the comedones that are the open ones, those are the ones called blackheads. 00:49 There's dilation and plugging at the follicular orifice. 00:52 We still have drainage. 00:54 And you'll see black or brown keratotic material. 00:57 And again that's the oxidation of the fatty acids. 00:59 The closed comedones. Now we're not getting anything out. 01:03 Those are frequently called whiteheads. 01:05 And it looks white because not so much lipid is there. 01:09 But we have keratin debris. 01:11 We have the sloughed cells coming from the superficial layer around the hair shaft and also from the skin proper. 01:20 So those will be papules that you will be able to be identified. 01:23 And this is going to now be the immediate precursor to the inflammatory acne. 01:28 Oops. Here we have inflammatory acne. 01:31 There will be these superficial papules and pustules. 01:35 And you already can in your mind's eye visualize what's going on deep. 01:38 So there's going to be basically neutrophils, macrophages and bugs waging a war and all the normal inflammatory mediators being elicited. 01:48 So we're going to get increased vascular permeability. 01:52 So there will be a little bit of edema. 01:54 We're going to see increased vascular engorgement. 01:56 So it will be red and all those inflammatory mediators may make it painful, may make it itchy. It's going to be inflamed. 02:05 Inflammatory acne is much more extensive. 02:09 And this is the nodular acne. 02:11 It's so we have had extension into the surrounding tissues. 02:15 It's not confined right around the hair follicle but in fact is more into the skin. And this can be much deeper abscesses and may require antibiotics. So the common locations for acne overall is going to be on the face, the neck, the upper chest back and shoulders. 02:33 In fact, those are going to be areas where we have the most sebaceous glands. 02:38 And therefore the more likely the location of the acne. 02:43 There will be some post-inflammatory hyperpigmentation. 02:46 This is due to a combination of bleeding that's associated with severe damage, and so that bleeding leaves behind hemosiderin. 02:55 So there will be some pigment associated with that. 02:58 In addition, there will be some increased activity of the melanocytes, so there will be some melanin. 03:04 This can persist for months, but typically does resolve as opposed to other lesions that we've seen, for example in lichen planus which typically don't resolve. There may be scarring. 03:15 Obviously we've had damage, significant damage down in the dermis. 03:20 And we can have varieties that range from atrophic looks like little depressed atrophic scars to very hypertrophic or even frank keloids. 03:28 And it all depends on the genetic underpinnings of the individual who has the more extensive damage. 03:35 The diagnosis is one of physical examination, Management overall. So now that you understand what's driving this. 03:41 Skin cleansers to reduce the bacterial burden overall, use cosmetics that tend not to clog the pores, the area around the hair shaft. 03:53 In mild disease you can use topical retinoids. 03:56 And these normalize the follicular hyperproliferation. 03:59 And they also tend to minimize inflammation. 04:02 You would also, could use topical antibiotics for mild disease. 04:06 This is not going to be for severe pustular disease. 04:10 Salicylic acids. These are keratolytic. 04:13 So they tend to cause the sloughing of the dead keratinocytes and therefore prevent the clogging. 04:21 You can use that as an alternative to the topical retinoids and azelaic acid also is has a similar effect to the retinoids. 04:30 For more moderate or severe disease we can we can get a little bit more aggressive. 04:35 So we may use oral contraceptives in women or spironolactone to modulate the hormonal environment and therefore minimize sebum production. 04:45 We can also give oral antibiotics to reduce the bacterial burden overall. 04:50 And you can use isotretinoin. 04:54 And that will help in all four of the pathogenic factors, including sebum production, keratinocyte maturation, bacterial proliferation, and inflammation. 05:05 When discussing acne complications with patients, it's important to emphasize not manipulating acne lesions. 05:14 Never squeeze or picket pimples, as this can force bacteria, sebum, and debris deeper into the skin, increasing inflammation and the risk of permanent scarring. 05:25 And additionally, manipulating lesions can spread bacteria leading to more breakouts. 05:31 The complications. So we don't normally talk about complications, but they are, they can be severe. 05:37 There's extensive psychosocial impacts due to the appearance of the affected skin, giving low self-esteem, anxiety and depression. 05:45 All of us who have had acne, you know, certainly before we went to the prom, just felt like we were going to die. 05:53 Um, there you can develop a more severe bacterial infections, secondary bacterial infection called folliculitis. 05:59 Um, with topical antibiotics, you may change the kind of microbiome and which bugs are prevalent and may have an overgrowth of those that are resistant to the topical antibiotic, and that can give rise to inflammation associated with the follicles hair follicles overall. Acne is a long-term condition, although it will spontaneously resolve. 06:27 Thankfully, in the majority of us, as our hormones kind of stabilize and we we learn good skincare. And in fact, there's maturation of the keratinocytes in some patients. However, acne may persist throughout adulthood. 06:44 But overall, we do have fairly good treatments now, and there's no reason to be walking around with terrible acne. 06:52 And with that, we've covered zits in all of their glory and splendor. 06:57 Thank you.
About the Lecture
The lecture Acne: Diagnosis and Management by Richard Mitchell, MD, PhD is from the course Inflammatory Lesions of the Skin.
Included Quiz Questions
What distinguishes blackheads from whiteheads in acne?
- Blackheads have open drainage with oxidized lipids, while whiteheads are closed with trapped keratin debris
- Blackheads are deep lesions, while whiteheads are superficial
- Blackheads contain bacteria, while whiteheads are sterile
- Blackheads are inflammatory, while whiteheads are non-inflammatory
- Blackheads occur on the face, while whiteheads occur on the trunk
Which finding indicates inflammatory rather than non-inflammatory acne?
- Pustules with surrounding erythema and edema
- Open comedones with black oxidized material
- Closed comedones with white appearance
- Surface plugging of hair follicles
- Hyperkeratotic plugs at follicular openings
Which medication addresses all four pathogenic factors of acne, including sebum production and inflammation?
- Isotretinoin
- Topical antibiotics
- Oral contraceptives
- Salicylic acid
- Spironolactone
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |