Playlist
Show Playlist
Hide Playlist
Abscesses – Staphylococcus Aureus
-
Slides 02 BacterialDiseases MicrobiologyAdvanced.pdf
-
Download Lecture Overview
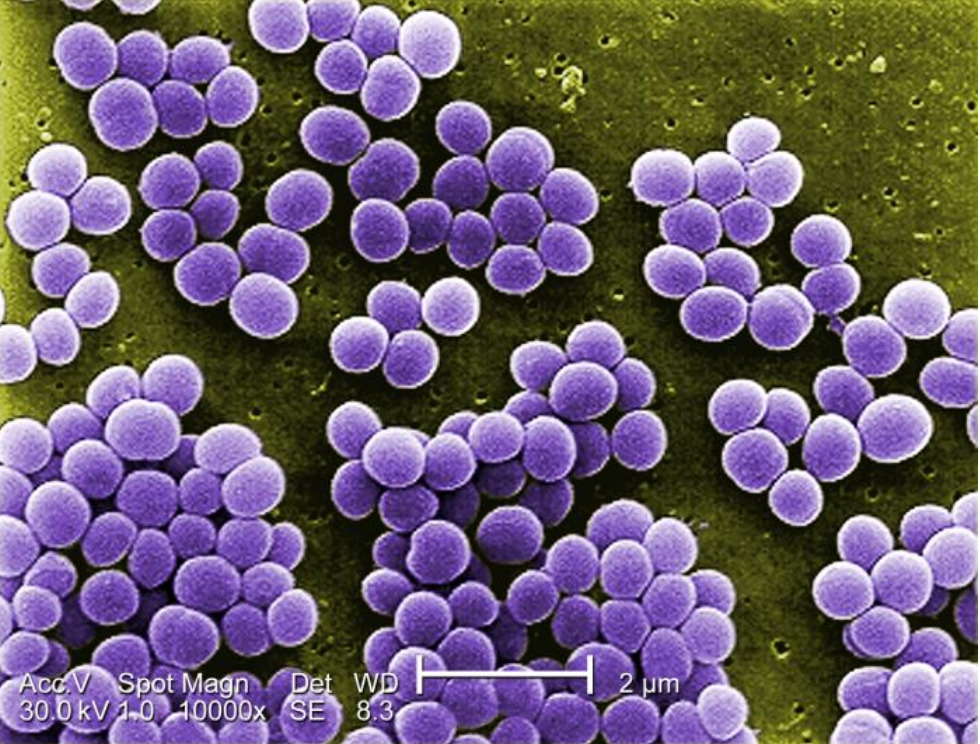
00:01 Now as I said before, they're on a certain percentage of humans on the skin and they remain there harmlessly typically. 00:08 And they don't penetrate unless there's damage to the skin, you have a cut that pushes the Staph aureus deeper and it can then cause an infection. 00:17 Or in a mucous membrane as well if you have a cut in the inside of your mouth, it may introduce the bacteria into deeper tissues where it can then cause a problem. 00:26 So if they're left in their normal places, they're okay and problems arise when there are damages occurring. 00:33 So things like burns, wounds of various sorts, lacerations, even an insect bite, certainly surgery, variety of skin diseases, all these conditions can let Staph aureus come in. 00:46 When you have surgery, one of the first things they do is to extensively wash the skin where you're going to be cut with a preparation to sterilize the area or reduce the number of bacteria. 00:59 If that's not done properly, the Staph aureus will be introduced into the wound and you can have serious infections of the sort that we're gonna talk about. 01:07 So let's look an abscess. Here's a photograph of a man. 01:10 You may think that this is infected nipple, but it's not. 01:14 It's in abscess caused by a staphylococcal infection. 01:18 The nipple is a little bit south of this boil on his chest. 01:23 So, this is an example of a boil caused by a staphylococcal infection. 01:28 Many people have had these. Here, the infection remains localized. 01:32 It is in this boil and it doesn't go beyond that. 01:36 This boil contains puss and that's called an abscess or a furuncle. Interesting word. 01:45 Furuncle is one boil like this. 01:48 A carbuncle is when you have several boils together, makes a larger structure. 01:52 Furuncle, carbuncle. So this is the – this is a typical boil, we call them colloquially or an abscess. 02:00 When the bacteria spread beyond the initial boil in subcutaneous or submucosal tissues, this is called cellulitis. 02:09 So the staphylococcal infection when it spreads beneath the skin cellulitis. 02:16 As you might predict one of the main immune defense cells important for regulating Staphylococcus replication and spread are neutrophils. 02:27 These maintain a balance of the bacteria in normal people and if you're neutropenic that can be a problem in controlling staphylococcal infections. 02:38 Very early in infection, let's say you have a cut and that introduces the staphylococci which you happen to have on your skin into deeper tissues, there's a battle between the bacteria and your immune system involving neutrophils and other cells. 02:53 Early in the infectious process, many neutrophils are killed by the bacteria and these release lysosomal enzymes, and neutrophils are full of them, i'ts part of their armamentarium for killing bacteria. 03:08 When the neutrophil dies, they're released into the tissue and those enzymes then damage your tissue and they contribute to the formation of a boil. 03:16 Let's take a little bit of a deeper look at what this boil actually is or abscess in more precise terminology. 03:25 So here is a diagram of the abscess on this slide. 03:30 An abscess is walled off with a capsule made of fibrin. 03:36 This is a host reaction to the bacteria. 03:39 The host makes a fibrin capsule to try and restrict the bacteria to this one place. 03:48 Now, the consequence of this is that the bacteria are also isolated from the immune response. 03:54 So it's actually a consequence both of host and bacterial action. 03:59 Within this boil or abscess, we have dead neutrophils which are killed by the bacteria and this produces the puss. 04:10 We have epithelial cells. 04:12 We have bacteria and fluid. And so this grows to a certain size. 04:17 It’s painful to a certain extent and that's what an abscess looks like. 04:22 Staph aureus makes a number of what we call virulence factors. 04:28 These are toxins and other proteins that are made that help it to spread and overcome host defenses. 04:36 And there are number of them in the center of that slide. 04:38 There are the staphylococci and you can see elaborating a variety of proteins like leucocidins, hemolysins, protein A, coagulases and proteins that help make fibrin clots dissolved. 04:53 Let's look at some of these in some detail. 04:56 Let's take a look at some of the virulence factors produced by staphylococci. 05:02 These are gram-positive bacteria's with a thick outer wall of peptidoglycan. 05:07 And surrounding that is a capsule which you may remember from our basic discussion of bacteria. 05:12 The capsule is important for inhibiting phagocytosis. 05:15 In this picture, we have a macrophage trying to take up the Staphylococcus and the capsule will inhibit that reaction, will resist it. 05:25 Because of course once the bacteria is inside of the cell, it could be destroyed. 05:29 The outer surface of the bacteria just below the capsule consists of peptidoglycan which you may remember is alternating change of carbohydrates cross-linked with short peptides. 05:43 This product of the Staphylococcus activates compliment. 05:47 This is a host defense against infection and compliment will have various inflammatory procedures that will cause lysis of the bacteria and production of cytokines. 05:59 And so this is part of the inflammatory reaction that goes on inside the carbuncle. 06:06 The bacteria also make a protein called protein A. 06:09 This is quite an interesting protein. 06:11 In the diagram, you can see the protein A is on the surface of the bacterium. It's shown in that little green box. 06:19 What this protein does is bind the Fc portion of antibody molecules. 06:24 So, you know, antibody molecules are Y-shaped molecules. 06:27 The Fc is down at the bottom and the antigen binding sites are at the top. 06:32 Normally, your antibodies would bind the Staphylococcus, but the Staphylococcus is binding the antibody the other way so it can't bind the bacterium. 06:43 And this reduces the ability of the bacterium to be taken up into macrophages by opsonization, very clever strategy for avoiding that process. 06:55 The capsule – the catalase is produced by staphylococci. 07:00 This is an enzyme that cleaves hydrogen peroxide. 07:04 That's hydrogen peroxide, H2O2 shown right there. 07:08 Hydrogen peroxide is produced by cells like macrophages. Its product is to destroy bacteria. 07:15 Bacteria in turn make an enzyme called catalase and this will cleave the hydrogen peroxide to evade destruction, very clever. 07:25 The bacteria also produce an enzyme called coagulase which converts fibrinogen to fibrin and that helps to make a clot that surrounds the boil and isolates the bacteria from the immune response. 07:38 And staphylococci also makes poor forming toxins like hemolsins, glucosidins and hyaluronidases that digest the extracellular matrix. 07:48 All of these in an effort for the bacteria to spread and avoid host defenses. 07:54 And we've talked about many of those before. 07:57 Staphylococcal infections are very difficult to treat. 08:01 Antibiotic resistance has become widespread among the staphylococcal strains that colonize us. 08:08 There are many beta-lactamases in these as we discussed in another lecture on general bacteria. 08:16 And those beta-lactamases include resistance to the penicillin type antibiotics. 08:22 This what – this resistance is widespread. 08:25 In addition, the bacteria make a penicillin binding protein 2A which further makes them resistant to penicillin class antibiotics. 08:33 And you may have heard the term MRSA or Mersa to describe these bacteria. 08:40 This stands for methicillin resistant Staph Aureus. 08:43 And this is very popular in the press to talk about MRSA as a superbug because they're extremely difficult to treat, almost impossible to treat with antibiotics. 08:53 So MRSA describes the most resistant of these strains of Staph aureus. 08:57 So these are serious infections.
About the Lecture
The lecture Abscesses – Staphylococcus Aureus by Vincent Racaniello, PhD is from the course Bacteria.
Included Quiz Questions
Which of the following is characteristic of MRSA?
- It makes a penicillin-binding protein 2a, creating penicillin resistance.
- It can be treated with higher doses of antibiotics if paired with exfoliative toxin A.
- If it carries the mecA gene, it has a high sensitivity to cephalosporins.
- MRSA stands for "methicillin-resistant Streptococcus aureus."
- Infections with this bacteria usually self-resolve with no intervention.
Which of the following terms describes a diffuse infection of the subcutaneous tissue often seen with S. aureus?
- Cellulitis
- Abscess
- Carbuncle
- Furuncle
- Scalded skin syndrome
A patient with recurrent Staphylococcus infections may be deficient in which of the following white blood cell types?
- Neutrophils
- Macrophages
- Lymphocytes
- NK cells
- Plasma cells
Which of the following represents a host response to a bacterial infection designed to isolate the invading pathogens?
- Formation of a fibrin capsule
- Pus formation
- Neutrophilic proliferation
- Cytokine release
Which of the following S. aureus virulence factors is correctly paired with the host response it interferes with or activates?
- Catalase - inactivates hydrogen peroxide
- Cell wall - inhibits complement activation
- Peptidoglycan - binds Fc portion of IgG
- Coagulase - inhibits respiratory burst
- Hemolysin - activates fibrin
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
Dr. Racaniello is a very good professor. He takes all his time to ensure that his students understand the concepts of the topics. All his feedbacks and examples are very relevant.