Playlist
Show Playlist
Hide Playlist
Abdominal Aortic Aneurysm (AAA): Management
-
Emergency Medicine Bord AAA.pdf
-
Download Lecture Overview
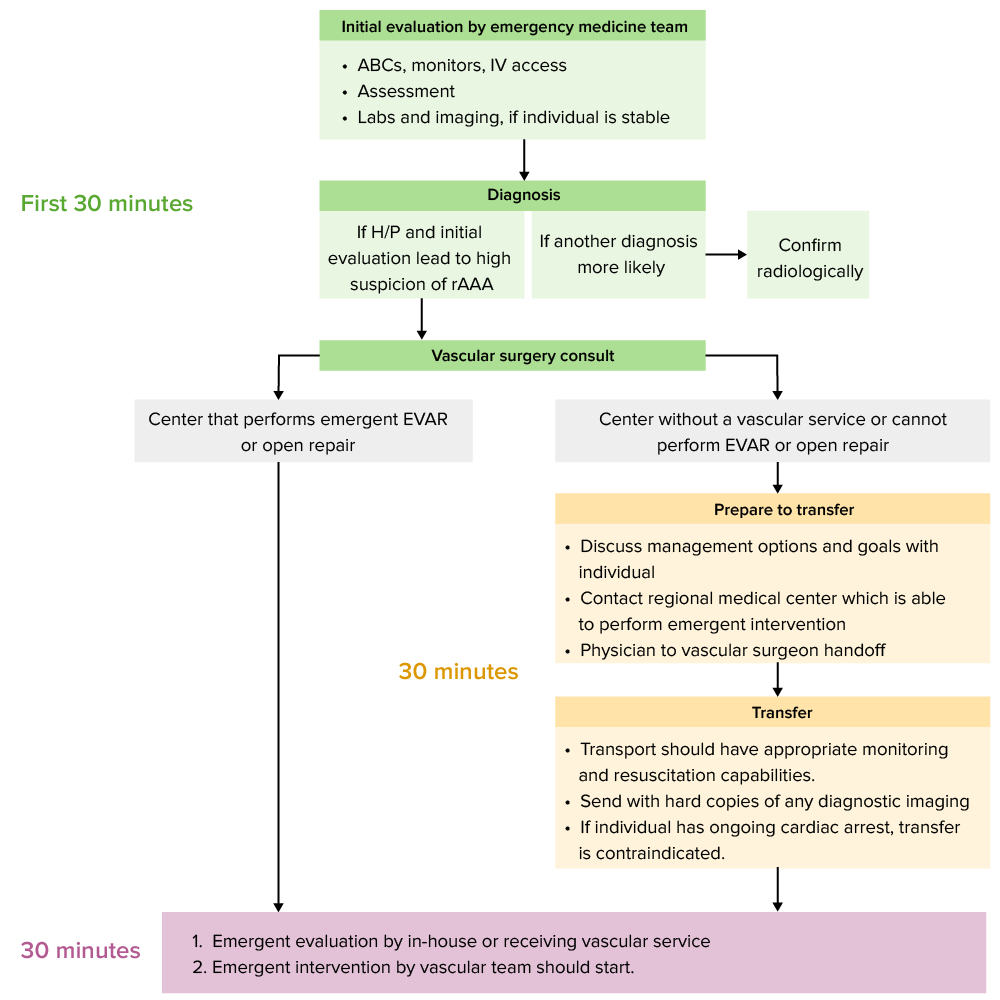
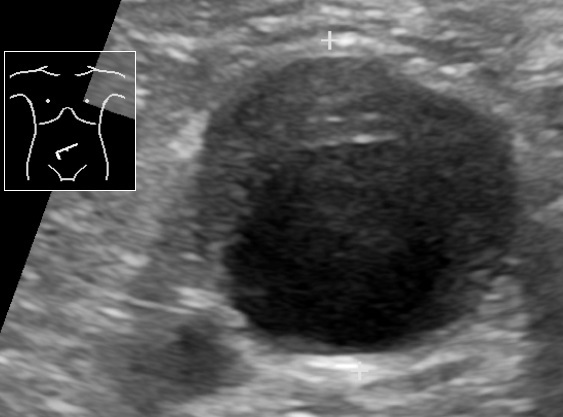
00:01 So our first steps here, the surgical consultation. 00:05 You wanna get that as soon as the diagnosis is suspected. 00:08 Never delay in a patient with hypotension or while awaiting imaging. 00:13 I can’t stress this enough. 00:15 If you are worried about this diagnosis, you call a surgeon. 00:18 This isn’t something you can fix in the emergency department. 00:22 This is something that will need emergent surgery. 00:24 One thing you can do is you can ensure that your patient gets adequate resuscitation. 00:30 What you wanna do in that situation is you wanna put in two large bore IVs. 00:35 You wanna send a type and cross match for your patient. 00:38 You wanna potentially give early blood. 00:41 So you wanna start volume resuscitating the patient nice and early. 00:46 Two large bore IVs just for clarification, generally, you want something that’s an 18 gauge IV or bigger, so an 18, a 16, or a 14. 00:56 I always like to remind students that volume resuscitating with a triple lumen catheter is not ideal. 01:02 The lumens actually on a triple lumen catheter are really quite small and long, and you don’t get a lot of great flow through that. 01:09 If you’re worried about your patient not having good peripheral IV access, you can also put in an intraosseous catheter or a Cordis which is basically a large central line and that would be how you would get a better volume resuscitation. 01:24 The other thing that’s important to note is that permissive hypotension actually may have a better outcome, so just maintaining the person’s systolic blood pressure of around 90 may be okay. 01:35 So we wanna make sure that we’re not resuscitating the patients too early necessarily but it’s okay if their blood pressure is around 90. 01:43 Other testing to get would be potentially other EKGs or labs, looking for other causes of presenting symptoms. 01:50 So although we’re talking about AAA here, it’s possible that the patient’s symptoms may not be due to AAA. 01:56 It’s possible they’re due to other concerning findings. 01:59 So you wanna make sure that you’re again, keeping your differential broad and not coming upon it really closure for this diagnosis. 02:06 Size matter when we’re talking about AAA. 02:09 Three to five centimeter triple As are less likely to rupture so if you get your imaging and that’s the size that you see, you can advise that your patient has outpatient follow-up. 02:18 Sometimes that’s easier said than done, but really try and get that patient plugged in to see a vascular surgeon. 02:24 Greater than 5 cm requires urgent follow-up with a surgeon, and what that means is generally, surgery follow-up within 3 to 5 days. 02:34 These patients are actually a pretty high risk of rupture or greater risk of rupture than the smaller sizes, so you wanna make sure that you go ahead and you stress to the patient the importance that they go see someone and also that when they’re discharged that you give them good return precautions. 02:50 Now, always keep in mind that if your patient doesn’t have the resources or doesn’t have health insurance, or the ability to see a doctor, that you make sure that they have some ability to kind of get in with an individual. 03:02 And then for a patient in whom you are – has asymptomatic or ruptured AAA, you wanna get that emergent surgical consultation. 03:11 You wanna involve that surgeon again nice and early but definitely if you’re worried that someone is symptomatic or the imaging shows that there is rupture, go ahead and call your surgeon who’s on call. 03:22 If you’re at a facility where there’s not the ability to repair the AAA, go ahead and work on getting that patient emergently transferred to another facility. 03:32 There are a few options for repair. 03:34 We’re not gonna go into them in too much detail here because we’re not talking about a vascular surgery course but basically, endovascular versus open repair are the two options. 03:43 In the most recent years, the endovascular or the less invasive treatment has become more readily available or more commonly used for patients versus the open repair and obviously, that has the advantage of it just being less invasive and potentially better for a patient. 04:01 Now, the vascular surgeon will discuss that and select the appropriate treatment with the patient. 04:06 So going back to our case here, so what are the best tests for this gentleman? So, first of all, first and foremost, we wanna maintain a high level of suspicion for this diagnosis. 04:16 While we may be thinking about other things, could he have a kidney stone? Could he have pancreatitis? Could he have muscular back pain? For the most part, you wanna think about in the ED, the differential of consequence. 04:27 What is highest on your differential of consequence? And here, what we’re talking about is the AAA, so you’re talking about an aortic aneurysm and potentially, a ruptured aortic aneurysm. 04:36 Involve your surgeon early. 04:38 For the most part, the surgeons wanna know about this early so they can start planning and if you have that high level of suspicion, get them on the phone, get them involved in the case. 04:47 For patients who have hemodynamic compromise like this gentleman, doing a bedside ultrasound to take a look at the aorta is gonna be a key initial study, so it’s gonna be a key thing that you can go ahead and take a look at, and see whether or not there’s further concern. 05:03 Definitely if you’re still worried and your ultrasound looks reassuring, potentially, you wanna move on to get that CAT scan when your patient is more stable. 05:10 So, the conclusion here is remember to keep this on your differential: can masquerade as it will a lot more benign conditions, so always make sure that you’re thinking about it. 05:21 You wanna assess hemodynamic stability when thinking about the imaging modality. 05:25 For a less stable patient, go ahead and get that ultrasound first. 05:29 For a patient who’s a little bit more stable, a CT scan with IV contrast may be a good first choice test. 05:36 You also wanna involve your surgeon early especially when you have a high level of suspicion for the diagnosis. 05:42 Sometimes there is no need to wait for that imaging test to come back. 05:45 Bedside ultrasound patient, for patients though who are unstable, has a pretty high sensitivity for triple A if you get a good study, if you are able to get a good look at the aorta, and it’s also important to remember that size matters, so that’s gonna affect what ultimately you’re gonna do for your patient. 06:01 If the aneurysm is small, the patient can have outpatient follow-up in a non-emergent way. 06:07 Somewhere in the middle, you wanna get them urgent follow-up and then for those symptomatic patients, so for patients who are having pain related to their AAA or definitely for those patients who are ruptured, that’s something that requires emergent treatment. 06:20 That’s the one who requires a trip to the operating room.
About the Lecture
The lecture Abdominal Aortic Aneurysm (AAA): Management by Sharon Bord, MD is from the course Abdominal and Genitourinary Emergencies.
Included Quiz Questions
What is the next best step to take as soon as an abdominal aortic aneurysm is suspected?
- Refer for surgical consultation
- Transfuse properly typed and cross-matched blood
- Allow permissive hypotension
- Assess for other causes of symptoms
- Hydrate the patient
In preparation for a possible blood transfusion, large-bore IVs must be placed in the patient. What is the ideal size of catheter that must be used?
- 18G
- 20G
- 21G
- 22G
- 24G
What is the ideal turnaround time for the surgical follow-up of a patient with a non-symptomatic abdominal aortic aneurysm measuring more than 5cm?
- Within 3–5 days
- Within 5–7 days
- After a week
- After two weeks
- Within a month
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
Thorough, objective and yet rich with practical details. I feel Dr. Bord has led us through the pathway of how to correctly approach this diagnosis and its management. It is filled with little tidbits and potential traps that she interspersed there for us. A great job!