Whipple's disease is a rare malabsorption syndrome with systemic manifestations (neurologic, cardiac, and musculoskeletal) caused by the bacterium Tropheryma whipplei. Patients often present with weight loss, diarrhea/steatorrhea, and arthralgias, as well as neurologic and cardiac manifestations. Whipple's disease is diagnosed with biopsy after the visualization of periodic acid–Schiff (PAS)-positive foamy macrophages Macrophages The relatively long-lived phagocytic cell of mammalian tissues that are derived from blood monocytes. Main types are peritoneal macrophages; alveolar macrophages; histiocytes; kupffer cells of the liver; and osteoclasts. They may further differentiate within chronic inflammatory lesions to epithelioid cells or may fuse to form foreign body giant cells or langhans giant cells. Innate Immunity: Phagocytes and Antigen Presentation in the involved tissues or with PCR PCR Polymerase chain reaction (PCR) is a technique that amplifies DNA fragments exponentially for analysis. The process is highly specific, allowing for the targeting of specific genomic sequences, even with minuscule sample amounts. The PCR cycles multiple times through 3 phases: denaturation of the template DNA, annealing of a specific primer to the individual DNA strands, and synthesis/elongation of new DNA molecules. Polymerase Chain Reaction (PCR) for the bacterial DNA DNA A deoxyribonucleotide polymer that is the primary genetic material of all cells. Eukaryotic and prokaryotic organisms normally contain DNA in a double-stranded state, yet several important biological processes transiently involve single-stranded regions. DNA, which consists of a polysugar-phosphate backbone possessing projections of purines (adenine and guanine) and pyrimidines (thymine and cytosine), forms a double helix that is held together by hydrogen bonds between these purines and pyrimidines (adenine to thymine and guanine to cytosine). DNA Types and Structure. It is managed with antibiotics, namely ceftriaxone Ceftriaxone A broad-spectrum cephalosporin antibiotic and cefotaxime derivative with a very long half-life and high penetrability to meninges, eyes and inner ears. Cephalosporins or penicillin Penicillin Rheumatic Fever G and sulfamethoxazole Sulfamethoxazole A bacteriostatic antibacterial agent that interferes with folic acid synthesis in susceptible bacteria. Its broad spectrum of activity has been limited by the development of resistance. Sulfonamides and Trimethoprim.
Last updated: Jan 10, 2024
Whipple’s disease is a malabsorption Malabsorption General term for a group of malnutrition syndromes caused by failure of normal intestinal absorption of nutrients. Malabsorption and Maldigestion syndrome with systemic manifestations that is caused by infection with Tropheryma whipplei.
Causative agent is T. whipplei:
Host immunodeficiency Immunodeficiency Chédiak-Higashi Syndrome has been implicated in symptomatic infections Infections Invasion of the host organism by microorganisms or their toxins or by parasites that can cause pathological conditions or diseases. Chronic Granulomatous Disease.

Endoscopic view of the jejunal mucosa in Whipple’s disease:
white lesions compatible with diffuse intestinal lymphangiectasia

T. whipplei–infected native mitral valve specimen:
transverse section of valve harboring voluminous bright yellow vegetations (arrowheads), up to 6 mm
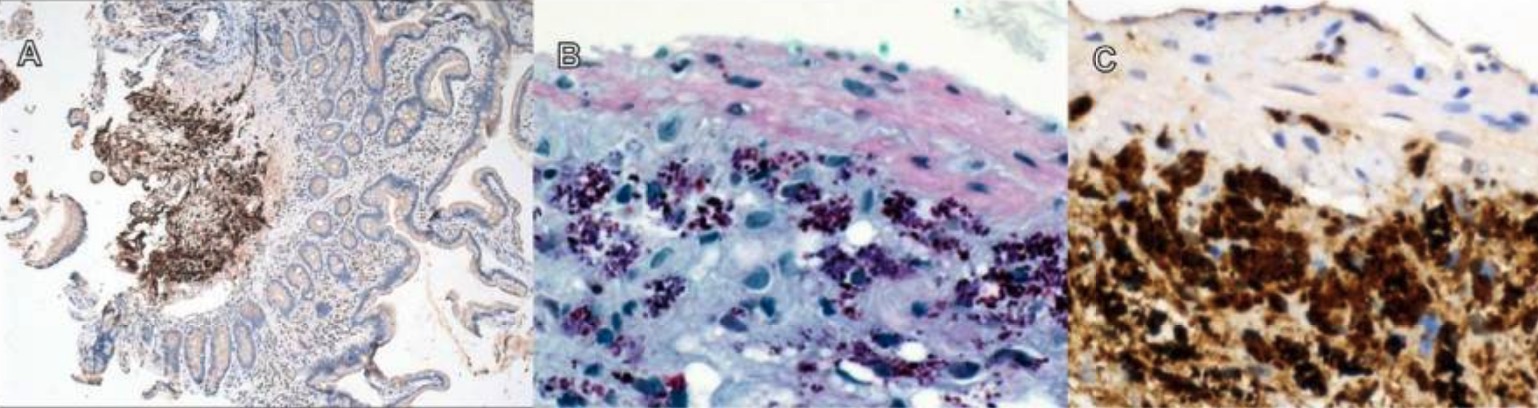
T. whipplei intestinal infection:
A: 40x magnification, T. whipplei immunostain visualized with hematoxylin
B: 400x magnification, PAS + macrophages
C: 400x magnification, dense submucosal aggregation of T. whipplei
The mainstay of treatment is antibiotics: