Acute rheumatic fever Fever Fever is defined as a measured body temperature of at least 38°C (100.4°F). Fever is caused by circulating endogenous and/or exogenous pyrogens that increase levels of prostaglandin E2 in the hypothalamus. Fever is commonly associated with chills, rigors, sweating, and flushing of the skin. Fever (ARF) is an autoimmune inflammatory process that usually follows Streptococcal pharyngitis Pharyngitis Pharyngitis is an inflammation of the back of the throat (pharynx). Pharyngitis is usually caused by an upper respiratory tract infection, which is viral in most cases. It typically results in a sore throat and fever. Other symptoms may include a runny nose, cough, headache, and hoarseness. Pharyngitis. Acute rheumatic fever Fever Fever is defined as a measured body temperature of at least 38°C (100.4°F). Fever is caused by circulating endogenous and/or exogenous pyrogens that increase levels of prostaglandin E2 in the hypothalamus. Fever is commonly associated with chills, rigors, sweating, and flushing of the skin. Fever usually occurs 2–4 weeks after an untreated infection and affects the heart, skin Skin The skin, also referred to as the integumentary system, is the largest organ of the body. The skin is primarily composed of the epidermis (outer layer) and dermis (deep layer). The epidermis is primarily composed of keratinocytes that undergo rapid turnover, while the dermis contains dense layers of connective tissue. Skin: Structure and Functions, joints, and nervous system Nervous system The nervous system is a small and complex system that consists of an intricate network of neural cells (or neurons) and even more glial cells (for support and insulation). It is divided according to its anatomical components as well as its functional characteristics. The brain and spinal cord are referred to as the central nervous system, and the branches of nerves from these structures are referred to as the peripheral nervous system. Nervous System: Anatomy, Structure, and Classification. This condition commonly presents with fever Fever Fever is defined as a measured body temperature of at least 38°C (100.4°F). Fever is caused by circulating endogenous and/or exogenous pyrogens that increase levels of prostaglandin E2 in the hypothalamus. Fever is commonly associated with chills, rigors, sweating, and flushing of the skin. Fever, arthritis Arthritis Acute or chronic inflammation of joints. Osteoarthritis of the large joints, pancarditis and sometimes rash Rash Rocky Mountain Spotted Fever and neurologic manifestations. The diagnosis is made clinically based on the Jones criteria, and confirmed with serologic tests. Prevention of ARF is the key treatment strategy, and is based on timely antibiotic treatment of the primary infection Primary infection Herpes Simplex Virus 1 and 2 as well as antibiotic prophylaxis Prophylaxis Cephalosporins of recurrent episodes. Management of acute episodes is largely supportive and includes anti-inflammatory medications. The most serious complication of ARF is development of rheumatic heart disease, which most commonly manifests as mitral valve Mitral valve The valve between the left atrium and left ventricle of the heart. Heart: Anatomy stenosis Stenosis Hypoplastic Left Heart Syndrome (HLHS).
Last updated: Dec 15, 2025
Acute rheumatic fever Fever Fever is defined as a measured body temperature of at least 38°C (100.4°F). Fever is caused by circulating endogenous and/or exogenous pyrogens that increase levels of prostaglandin E2 in the hypothalamus. Fever is commonly associated with chills, rigors, sweating, and flushing of the skin. Fever (ARF) is an autoimmune condition that develops as a complication of streptococcal infection.
The pathogenesis is not completely understood.
Genetic predisposition is likely, as rheumatic fever Fever Fever is defined as a measured body temperature of at least 38°C (100.4°F). Fever is caused by circulating endogenous and/or exogenous pyrogens that increase levels of prostaglandin E2 in the hypothalamus. Fever is commonly associated with chills, rigors, sweating, and flushing of the skin. Fever tends to be familial:
The major implied mechanism is molecular mimicry:
Acute phase Acute phase Short Bowel Syndrome
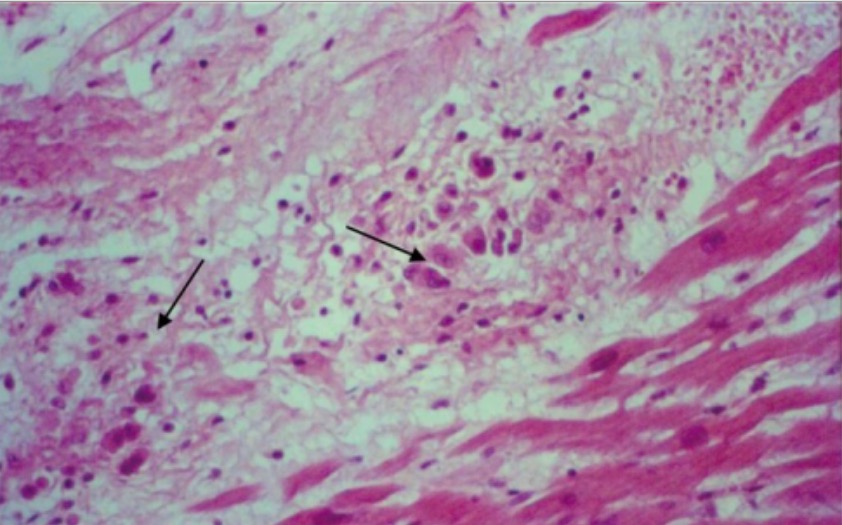
Aschoff bodies (arrows) in the papillary muscle of the mitral valve
Image: “Histopathological findings” by Valvular Heart Disease Department, Heart Institute (InCor), University of São Paulo Medical School, São Paulo, Brazil. License: CC BY 4.0Chronic phase Chronic phase HIV Infection and AIDS
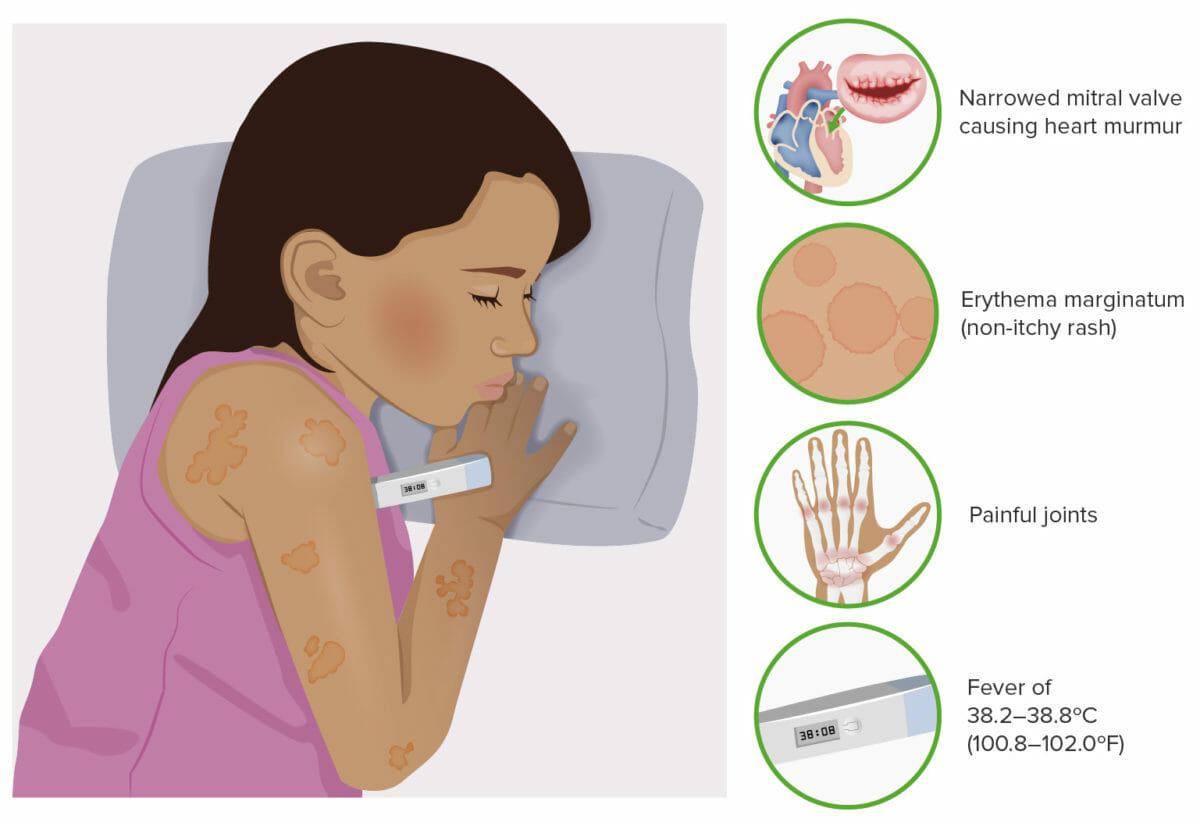
Typical symptoms of rheumatic fever
Image by Lecturio.To recall the main clinical manifestations in acute rheumatic fever Fever Fever is defined as a measured body temperature of at least 38°C (100.4°F). Fever is caused by circulating endogenous and/or exogenous pyrogens that increase levels of prostaglandin E2 in the hypothalamus. Fever is commonly associated with chills, rigors, sweating, and flushing of the skin. Fever, remember the Jones criteria (written as J❤NES):

A throat swab sample needs to be obtained for suspected streptococcal pharyngitis.
Image: “10190” by CDC/ Dr. M. Moody. License: Public Domain
Chest X-ray showing marked cardiomegaly associated with rheumatic mitral valve stenosis
Image: “Chest radiography” by Institut de Cardiologie d’Abidjan, BP V 206 Abidjan, Cote d’Ivoire ; Thorax and Vessels Department, Université de Cocody, 01 BP 166 Abidjan, Cote d’Ivoire. License: CC BY 3.0
Echocardiographic frames in the parasternal long-axis (A) and apical 4-chamber (B) views from a 13-year-old girl with severe mitral stenosis and mild regurgitation, showing giant left atrium
MV: mitral valve
LV: left ventricle
RV: right ventricle
RA: right atrium
Goals:
Eradication of streptococcal infection:
Arthritis Arthritis Acute or chronic inflammation of joints. Osteoarthritis:
Severe carditis:
Sydenham chorea Chorea Involuntary, forcible, rapid, jerky movements that may be subtle or become confluent, markedly altering normal patterns of movement. Hypotonia and pendular reflexes are often associated. Conditions which feature recurrent or persistent episodes of chorea as a primary manifestation of disease are referred to as choreatic disorders. Chorea is also a frequent manifestation of basal ganglia diseases. Huntington Disease is usually self-limited and does not require specific treatment.
| Rheumatic fever Fever Fever is defined as a measured body temperature of at least 38°C (100.4°F). Fever is caused by circulating endogenous and/or exogenous pyrogens that increase levels of prostaglandin E2 in the hypothalamus. Fever is commonly associated with chills, rigors, sweating, and flushing of the skin. Fever presentation | Duration of prophylaxis Prophylaxis Cephalosporins |
|---|---|
| Rheumatic fever Fever Fever is defined as a measured body temperature of at least 38°C (100.4°F). Fever is caused by circulating endogenous and/or exogenous pyrogens that increase levels of prostaglandin E2 in the hypothalamus. Fever is commonly associated with chills, rigors, sweating, and flushing of the skin. Fever with carditis and residual heart disease (persistent valvular disease) | 10 years or until age 40 years (whichever is longer); lifetime prophylaxis Prophylaxis Cephalosporins may be needed |
| Rheumatic fever Fever Fever is defined as a measured body temperature of at least 38°C (100.4°F). Fever is caused by circulating endogenous and/or exogenous pyrogens that increase levels of prostaglandin E2 in the hypothalamus. Fever is commonly associated with chills, rigors, sweating, and flushing of the skin. Fever with carditis but no residual heart disease (no valvular disease) | 10 years or until age 21 years (whichever is longer) |
| Rheumatic fever Fever Fever is defined as a measured body temperature of at least 38°C (100.4°F). Fever is caused by circulating endogenous and/or exogenous pyrogens that increase levels of prostaglandin E2 in the hypothalamus. Fever is commonly associated with chills, rigors, sweating, and flushing of the skin. Fever without carditis | 5 years or until age 21 years (whichever is longer) |