Idiopathic Idiopathic Dermatomyositis pulmonary fibrosis Fibrosis Any pathological condition where fibrous connective tissue invades any organ, usually as a consequence of inflammation or other injury. Bronchiolitis Obliterans is a specific entity of the major idiopathic Idiopathic Dermatomyositis interstitial pneumonia Pneumonia Pneumonia or pulmonary inflammation is an acute or chronic inflammation of lung tissue. Causes include infection with bacteria, viruses, or fungi. In more rare cases, pneumonia can also be caused through toxic triggers through inhalation of toxic substances, immunological processes, or in the course of radiotherapy. Pneumonia classification of interstitial lung diseases Interstitial Lung Diseases Interstitial lung diseases are a heterogeneous group of disorders characterized by the inflammation and fibrosis of lung parenchyma, especially the pulmonary connective tissue in the alveolar walls. It may be idiopathic (e.g., idiopathic pulmonary fibrosis) or secondary to connective tissue diseases, medications, malignancies, occupational exposure, or allergens. Interstitial Lung Diseases. As implied by the name, the exact causes are poorly understood. Patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship often present in the moderate to advanced stage with progressive dyspnea Dyspnea Dyspnea is the subjective sensation of breathing discomfort. Dyspnea is a normal manifestation of heavy physical or psychological exertion, but also may be caused by underlying conditions (both pulmonary and extrapulmonary). Dyspnea and nonproductive cough. The diagnosis is made by characteristic imaging findings, pulmonary function testing Pulmonary Function Testing Pulmonary Function Tests that indicates restrictive lung disease, and (if necessary) lung biopsy Lung Biopsy Antineutrophil Cytoplasmic Antibody (ANCA)-Associated Vasculitis. Options are limited for therapies to slow progression. Lung transplantation Lung transplantation The transference of either one or both of the lungs from one human or animal to another. Organ Transplantation is the only curative intervention if the patient is a candidate for one.
Last updated: May 17, 2024
Idiopathic Idiopathic Dermatomyositis pulmonary fibrosis Fibrosis Any pathological condition where fibrous connective tissue invades any organ, usually as a consequence of inflammation or other injury. Bronchiolitis Obliterans (IPF) is the most common type of interstitial lung disease ( ILD ILD Interstitial lung diseases are a heterogeneous group of disorders characterized by the inflammation and fibrosis of lung parenchyma, especially the pulmonary connective tissue in the alveolar walls. It may be idiopathic (e.g., idiopathic pulmonary fibrosis) or secondary to connective tissue diseases, medications, malignancies, occupational exposure, or allergens. Interstitial Lung Diseases) and is characterized by chronic, progressive, irreversible fibrosis Fibrosis Any pathological condition where fibrous connective tissue invades any organ, usually as a consequence of inflammation or other injury. Bronchiolitis Obliterans of the lung parenchyma.
IPF has been difficult to study because of its rarity and evolution in diagnostic practices.
The cause of IPF remains largely unclear. However, in the current hypothesis Hypothesis A hypothesis is a preliminary answer to a research question (i.e., a “guess” about what the results will be). There are 2 types of hypotheses: the null hypothesis and the alternative hypothesis. Statistical Tests and Data Representation regarding the pathogenesis of IPF, the following exposures may lead to the initial alveolar epithelial injury:
The underlying mechanism is poorly understood.
Patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship with IPF can have variable Variable Variables represent information about something that can change. The design of the measurement scales, or of the methods for obtaining information, will determine the data gathered and the characteristics of that data. As a result, a variable can be qualitative or quantitative, and may be further classified into subgroups. Types of Variables presentations, and early in its course, IPF can be asymptomatic.
General findings:
Patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship can present with pulmonary hypertension Pulmonary Hypertension Pulmonary hypertension (PH) or pulmonary arterial hypertension (PAH) is characterized by elevated pulmonary arterial pressure, which can lead to chronic progressive right heart failure. Pulmonary hypertension is grouped into 5 categories based on etiology, which include primary PAH, and PH due to cardiac disease, lung or hypoxic disease, chronic thromboembolic disease, and multifactorial or unclear etiologies. Pulmonary Hypertension ( PH pH The quantitative measurement of the acidity or basicity of a solution. Acid-Base Balance) and cor pulmonale Cor Pulmonale Cor pulmonale is right ventricular (RV) dysfunction caused by lung disease that results in pulmonary artery hypertension. The most common cause of cor pulmonale is chronic obstructive pulmonary disease. Dyspnea is the usual presenting symptom. Cor Pulmonale:

Nail clubbing:
Clubbed nails are abnormal, rounded nail beds often seen in association with conditions causing chronic hypoxemia, such as cystic fibrosis or interstitial lung disease.
Idiopathic Idiopathic Dermatomyositis pulmonary fibrosis Fibrosis Any pathological condition where fibrous connective tissue invades any organ, usually as a consequence of inflammation or other injury. Bronchiolitis Obliterans is diagnosed by a combination of radiologic, pathologic, and clinical investigations.
It is critical to obtain the following on top of a complete medical history to ensure that other causes of ILD ILD Interstitial lung diseases are a heterogeneous group of disorders characterized by the inflammation and fibrosis of lung parenchyma, especially the pulmonary connective tissue in the alveolar walls. It may be idiopathic (e.g., idiopathic pulmonary fibrosis) or secondary to connective tissue diseases, medications, malignancies, occupational exposure, or allergens. Interstitial Lung Diseases are excluded:
Typical findings:
Measurements:
Chest X-ray X-ray Penetrating electromagnetic radiation emitted when the inner orbital electrons of an atom are excited and release radiant energy. X-ray wavelengths range from 1 pm to 10 nm. Hard x-rays are the higher energy, shorter wavelength x-rays. Soft x-rays or grenz rays are less energetic and longer in wavelength. The short wavelength end of the x-ray spectrum overlaps the gamma rays wavelength range. The distinction between gamma rays and x-rays is based on their radiation source. Pulmonary Function Tests:
High-resolution CT High-resolution CT Imaging of the Lungs and Pleura ( HRCT HRCT Pulmonary Function Tests) scan:
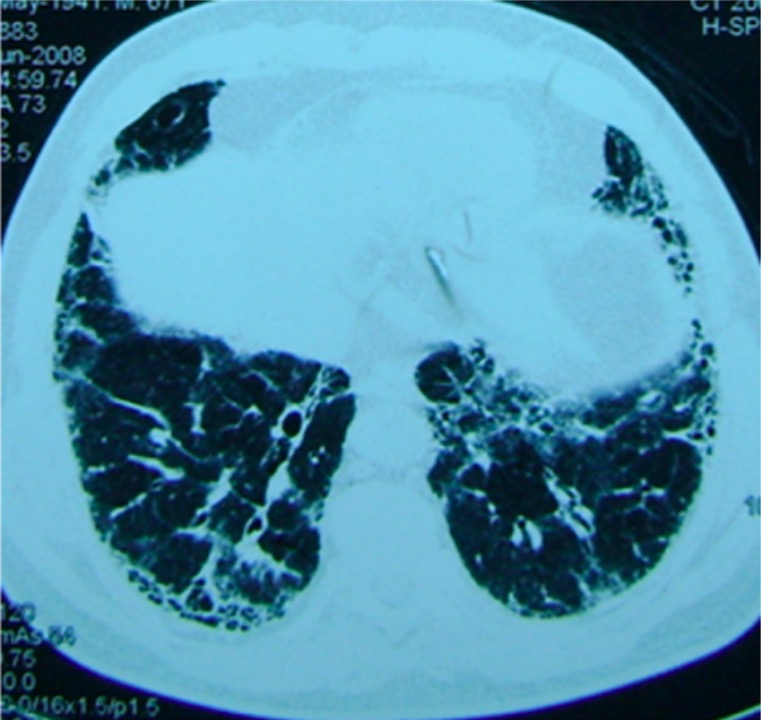
CT image from a patient with pulmonary fibrosis:
A basilar reticular pattern is seen.
Surgical specimens can be obtained using video-assisted thoracoscopic surgery (VATS). Patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship with IPF may show a pattern of usual interstitial pneumonia Pneumonia Pneumonia or pulmonary inflammation is an acute or chronic inflammation of lung tissue. Causes include infection with bacteria, viruses, or fungi. In more rare cases, pneumonia can also be caused through toxic triggers through inhalation of toxic substances, immunological processes, or in the course of radiotherapy. Pneumonia:
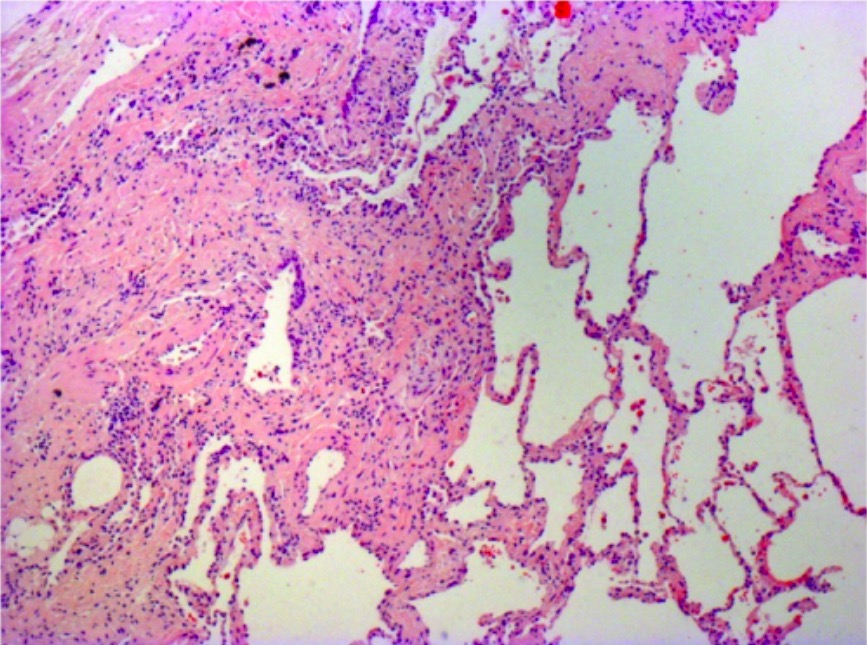
Photomicrograph of biopsy from a patient with idiopathic pulmonary fibrosis:
The typical histopathologic features of usual interstitial pneumonia are seen, characterized by spatial heterogeneity with areas of subpleural and paraseptal fibrosis and honeycombing changes (cystic airspaces lined by bronchiolar epithelium) alternating with areas of relatively spared lung parenchyma, temporal heterogeneity with admixed areas of active fibrosis with fibroblast foci, extracellular matrix deposition (mainly collagen), and relative mild or absent inflammatory cell infiltrate together with regions of histologically normal lung tissue.
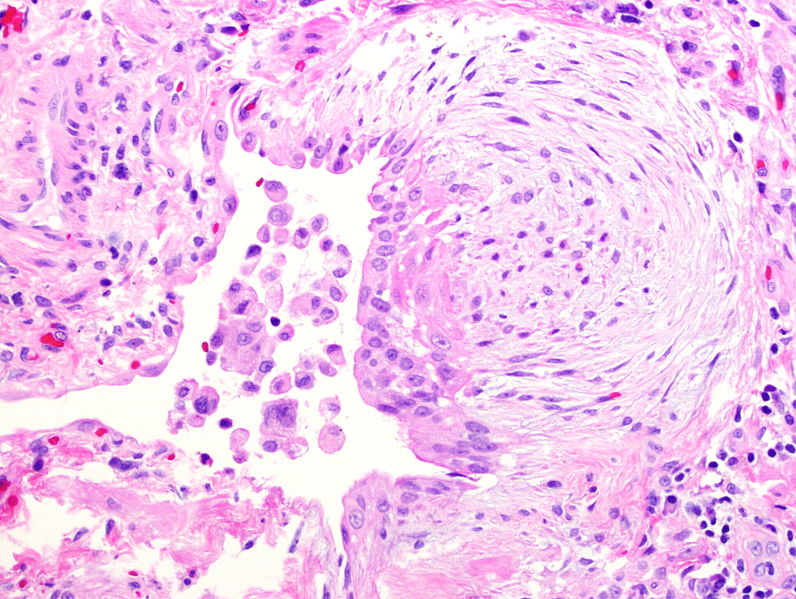
Fibroblast focus seen in idiopathic pulmonary fibrosis due to migration and proliferation of fibroblasts and myofibroblasts
Image: “Fibroblast focus” by Mutleysmith. License: Public DomainThe following can be performed to exclude other causes of ILD ILD Interstitial lung diseases are a heterogeneous group of disorders characterized by the inflammation and fibrosis of lung parenchyma, especially the pulmonary connective tissue in the alveolar walls. It may be idiopathic (e.g., idiopathic pulmonary fibrosis) or secondary to connective tissue diseases, medications, malignancies, occupational exposure, or allergens. Interstitial Lung Diseases and will be guided by clinical suspicion:
There are limited options for pharmacologic treatment in patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship with IPF, and none provide a cure.
Antifibrotic agents:
PH pH The quantitative measurement of the acidity or basicity of a solution. Acid-Base Balance management:
GERD GERD Gastroesophageal reflux disease (GERD) occurs when the stomach acid frequently flows back into the esophagus. This backwash (acid reflux) can irritate the lining of the esophagus, causing symptoms such as retrosternal burning pain (heartburn). Gastroesophageal Reflux Disease (GERD) management:
IPF progression is associated with an estimated median survival time of up to 5 years following the diagnosis.