Portal hypertension Hypertension Hypertension, or high blood pressure, is a common disease that manifests as elevated systemic arterial pressures. Hypertension is most often asymptomatic and is found incidentally as part of a routine physical examination or during triage for an unrelated medical encounter. Hypertension is increased pressure in the portal venous system. This increased pressure can lead to splanchnic vasodilation Vasodilation The physiological widening of blood vessels by relaxing the underlying vascular smooth muscle. Pulmonary Hypertension Drugs, collateral blood flow Blood flow Blood flow refers to the movement of a certain volume of blood through the vasculature over a given unit of time (e.g., mL per minute). Vascular Resistance, Flow, and Mean Arterial Pressure through portosystemic anastomoses Portosystemic anastomoses Systemic and Special Circulations, and increased hydrostatic pressure Hydrostatic pressure The pressure due to the weight of fluid. Edema. There are a number of etiologies, including cirrhosis Cirrhosis Cirrhosis is a late stage of hepatic parenchymal necrosis and scarring (fibrosis) most commonly due to hepatitis C infection and alcoholic liver disease. Patients may present with jaundice, ascites, and hepatosplenomegaly. Cirrhosis can also cause complications such as hepatic encephalopathy, portal hypertension, portal vein thrombosis, and hepatorenal syndrome. Cirrhosis, right-sided heart failure Right-Sided Heart Failure Ebstein’s Anomaly, schistosomiasis Schistosomiasis Infection with flukes (trematodes) of the genus schistosoma. Three species produce the most frequent clinical diseases: Schistosoma haematobium (endemic in Africa and the Middle East), Schistosoma Mansoni (in Egypt, northern and southern Africa, some West Indies islands, northern 2/3 of South america), and Schistosoma japonicum (in Japan, China, the Philippines, Celebes, Thailand, Laos). S. mansoni is often seen in Puerto Ricans living in the United States. Schistosoma/Schistosomiasis, portal vein Portal vein A short thick vein formed by union of the superior mesenteric vein and the splenic vein. Liver: Anatomy thrombosis Thrombosis Formation and development of a thrombus or blood clot in the blood vessel. Epidemic Typhus, hepatitis, and Budd-Chiari syndrome Budd-Chiari syndrome Budd-Chiari syndrome is a condition resulting from the interruption of the normal outflow of blood from the liver. The primary type arises from a venous process (affecting the hepatic veins or inferior vena cava) such as thrombosis, but can also be from a lesion compressing or invading the veins (secondary type). The patient typically presents with hepatomegaly, ascites, and abdominal discomfort. Budd-Chiari Syndrome. Most individuals are asymptomatic until complications arise, including esophageal varices, portal hypertensive gastropathy gastropathy Damage to the epithelial lining with no or minimal associated inflammation and is technically a separate entity from gastritis Gastritis, ascites Ascites Ascites is the pathologic accumulation of fluid within the peritoneal cavity that occurs due to an osmotic and/or hydrostatic pressure imbalance secondary to portal hypertension (cirrhosis, heart failure) or non-portal hypertension (hypoalbuminemia, malignancy, infection). Ascites, and hypersplenism Hypersplenism Condition characterized by splenomegaly, some reduction in the number of circulating blood cells in the presence of a normal or hyperactive bone marrow, and the potential for reversal by splenectomy. Splenomegaly. The diagnosis is clinical, but it can be supported by ultrasound findings (and hepatic venous pressure gradient Pressure gradient Vascular Resistance, Flow, and Mean Arterial Pressure measurement in unclear cases). Management requires treating the underlying etiology and managing the complications. This can include nonselective beta blockers to prevent bleeding from varices, diuretics Diuretics Agents that promote the excretion of urine through their effects on kidney function. Heart Failure and Angina Medication and sodium Sodium A member of the alkali group of metals. It has the atomic symbol na, atomic number 11, and atomic weight 23. Hyponatremia restriction for ascites Ascites Ascites is the pathologic accumulation of fluid within the peritoneal cavity that occurs due to an osmotic and/or hydrostatic pressure imbalance secondary to portal hypertension (cirrhosis, heart failure) or non-portal hypertension (hypoalbuminemia, malignancy, infection). Ascites, and transjugular intrahepatic portosystemic shunt Transjugular intrahepatic portosystemic shunt A type of surgical portosystemic shunt to reduce portal hypertension with associated complications of esophageal varices and ascites. It is performed percutaneously through the jugular vein and involves the creation of an intrahepatic shunt between the hepatic vein and portal vein. The channel is maintained by a metallic stent. The procedure can be performed in patients who have failed sclerotherapy and is an additional option to the surgical techniques of portocaval, mesocaval, and splenorenal shunts. It takes one to three hours to perform. Ascites for refractory complications.
Last updated: May 17, 2024
The etiologies of portal hypertension Hypertension Hypertension, or high blood pressure, is a common disease that manifests as elevated systemic arterial pressures. Hypertension is most often asymptomatic and is found incidentally as part of a routine physical examination or during triage for an unrelated medical encounter. Hypertension can be classified based on the location of increased resistance Resistance Physiologically, the opposition to flow of air caused by the forces of friction. As a part of pulmonary function testing, it is the ratio of driving pressure to the rate of air flow. Ventilation: Mechanics of Breathing to blood flow Blood flow Blood flow refers to the movement of a certain volume of blood through the vasculature over a given unit of time (e.g., mL per minute). Vascular Resistance, Flow, and Mean Arterial Pressure through the liver Liver The liver is the largest gland in the human body. The liver is found in the superior right quadrant of the abdomen and weighs approximately 1.5 kilograms. Its main functions are detoxification, metabolism, nutrient storage (e.g., iron and vitamins), synthesis of coagulation factors, formation of bile, filtration, and storage of blood. Liver: Anatomy.
Prehepatic etiologies:
Hepatic etiologies:
Posthepatic etiologies:
Anatomy:
Portal hypertension Hypertension Hypertension, or high blood pressure, is a common disease that manifests as elevated systemic arterial pressures. Hypertension is most often asymptomatic and is found incidentally as part of a routine physical examination or during triage for an unrelated medical encounter. Hypertension:
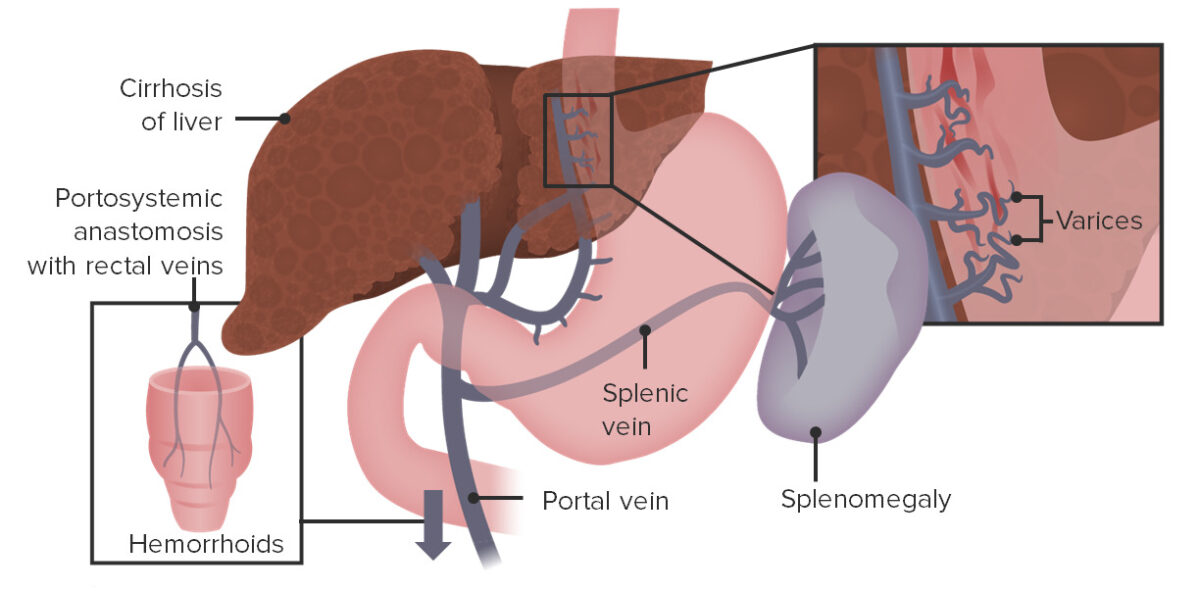
Esophageal varices, splenomegaly, and rectal varices resulting from backup of blood flow due to elevated pressures within the portal vein
Image by Lecturio.Portal hypertension Hypertension Hypertension, or high blood pressure, is a common disease that manifests as elevated systemic arterial pressures. Hypertension is most often asymptomatic and is found incidentally as part of a routine physical examination or during triage for an unrelated medical encounter. Hypertension itself usually has no symptoms. Clinical manifestations arise as a result of the underlying etiology and/or complications.
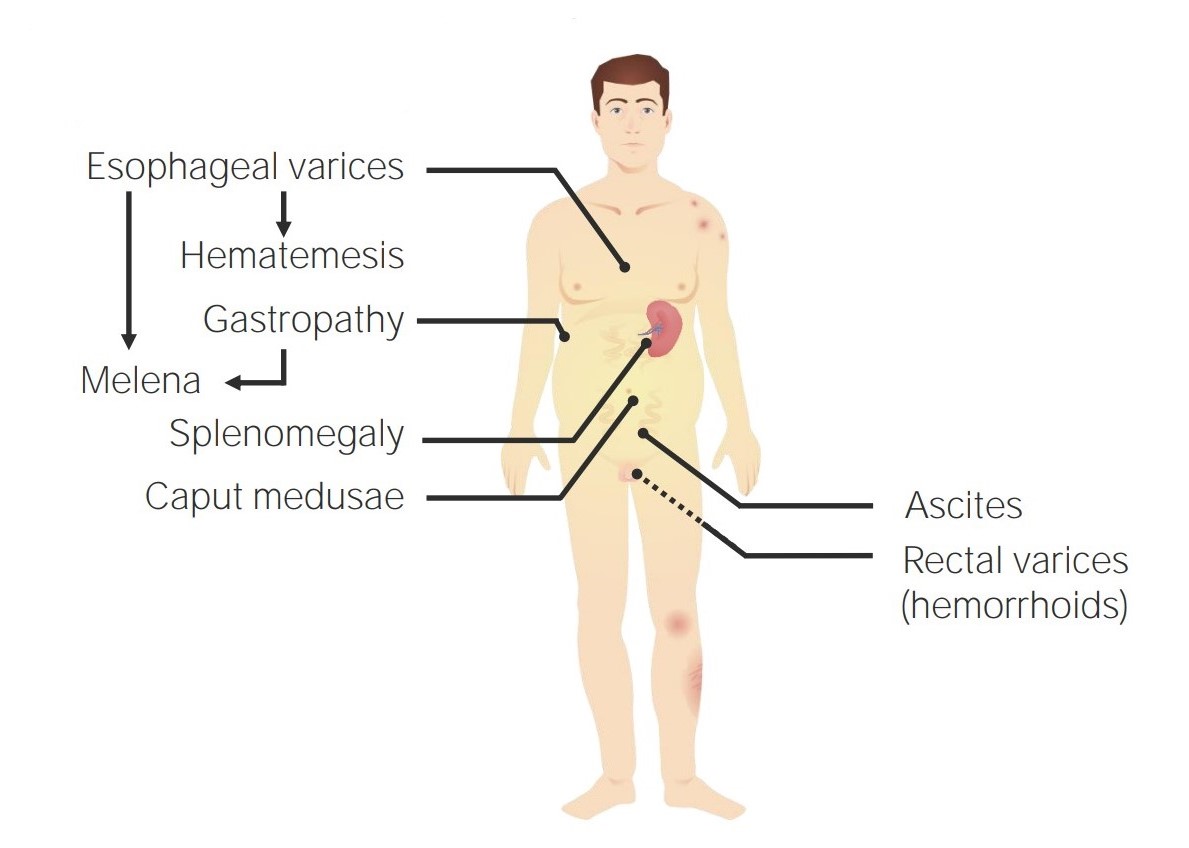
Symptoms resulting from portal hypertension
Image by Lecturio.
Ascites secondary to hepatic cirrhosis
Image: “Draining ascites, secondary to hepatic cirrhosis” by John Campbell. License: Public DomainThe diagnosis of portal hypertension Hypertension Hypertension, or high blood pressure, is a common disease that manifests as elevated systemic arterial pressures. Hypertension is most often asymptomatic and is found incidentally as part of a routine physical examination or during triage for an unrelated medical encounter. Hypertension is generally based on clinical evaluation, but it may be supported by:
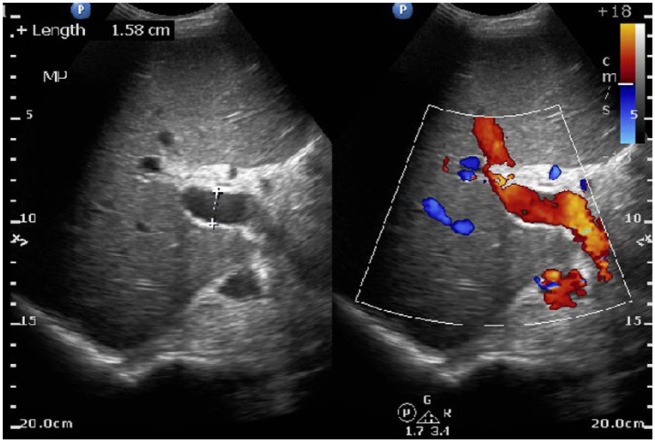
Ultrasound of the liver identifies a large portal vein, consistent with portal hypertension.
Image: “Ultrasound abdomen: ultrasound of liver identifies a patent portal vein, 158 mm in diameter, indicative of portal hypertension in this noncirrhotic patient.” by Ratnayake S. et al. License: CC BY 3.0Additional studies may be performed based on the clinical presentation and presence of complications.

Endoscopic view of the esophageal varices:
The red patches indicate a recent bleed.
The focus of therapy is to prevent and treat the complications of portal vein Portal vein A short thick vein formed by union of the superior mesenteric vein and the splenic vein. Liver: Anatomy thrombosis Thrombosis Formation and development of a thrombus or blood clot in the blood vessel. Epidemic Typhus. It is also important to treat the underlying etiology (when possible).