Peripheral nerve damage affecting the upper extremities is a common occupational injury and also occurs in individuals who participate in recreational sports. Injuries can affect the axillary, musculocutaneous, median, ulnar, or radial nerves. The most common causes of these injuries are overuse, compression Compression Blunt Chest Trauma or entrapment, or nerve trauma; degenerative or demyelinating disorders Demyelinating disorders Conditions characterized by loss or dysfunction of myelin in the brain, spinal cord, or optic nerves secondary to autoimmune mediated processes. This may take the form of a humoral or cellular immune response directed toward myelin or oligodendroglia associated autoantigens. Posterior Cord Syndrome; radiation Radiation Emission or propagation of acoustic waves (sound), electromagnetic energy waves (such as light; radio waves; gamma rays; or x-rays), or a stream of subatomic particles (such as electrons; neutrons; protons; or alpha particles). Osteosarcoma therapy; and mass Mass Three-dimensional lesion that occupies a space within the breast Imaging of the Breast lesions. Clinical presentation is with motor Motor Neurons which send impulses peripherally to activate muscles or secretory cells. Nervous System: Histology and/or sensory Sensory Neurons which conduct nerve impulses to the central nervous system. Nervous System: Histology deficits. Diagnosis is made clinically and based on electrodiagnostic and imaging studies. Treatment in most cases is conservative, although surgical intervention may occasionally be necessary.
Last updated: Jan 15, 2024
The brachial plexus Brachial Plexus The large network of nerve fibers which distributes the innervation of the upper extremity. The brachial plexus extends from the neck into the axilla. In humans, the nerves of the plexus usually originate from the lower cervical and the first thoracic spinal cord segments (c5-c8 and T1), but variations are not uncommon. Peripheral Nerve Injuries in the Cervicothoracic Region is a network of nerves that originates in the posterior triangle Posterior triangle Triangles of the Neck: Anatomy of the neck Neck The part of a human or animal body connecting the head to the rest of the body. Peritonsillar Abscess and passes to the axilla Axilla The axilla is a pyramid-shaped space located between the upper thorax and the arm. The axilla has a base, an apex, and 4 walls (anterior, medial, lateral, posterior). The base of the pyramid is made up of the axillary skin. The apex is the axillary inlet, located between the 1st rib, superior border of the scapula, and clavicle. Axilla and Brachial Plexus: Anatomy. The brachial plexus Brachial Plexus The large network of nerve fibers which distributes the innervation of the upper extremity. The brachial plexus extends from the neck into the axilla. In humans, the nerves of the plexus usually originate from the lower cervical and the first thoracic spinal cord segments (c5-c8 and T1), but variations are not uncommon. Peripheral Nerve Injuries in the Cervicothoracic Region is formed by the spinal nerve roots C5 to T1, which then divides and branches to provide all of the somatic innervation and some sympathetic innervation to the upper extremities.
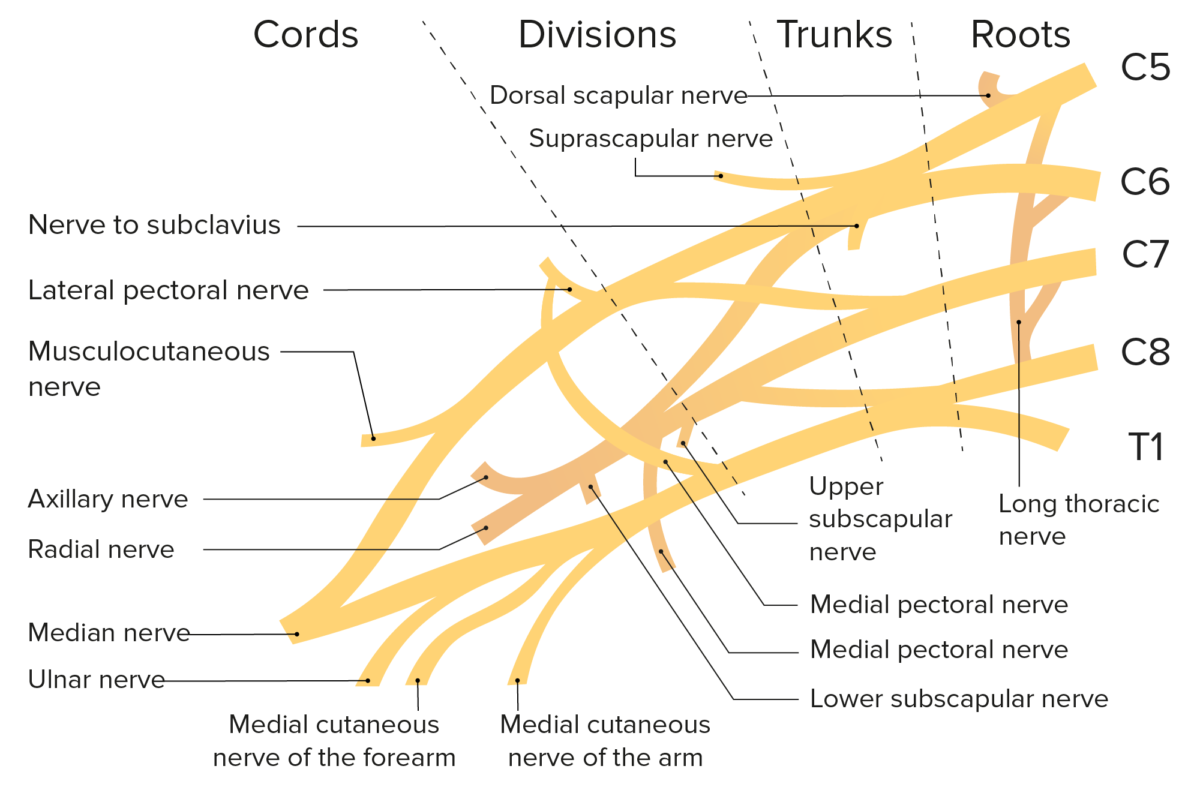
Schematic of the brachial plexus and its branches
Image by BioDigital, edited by Lecturio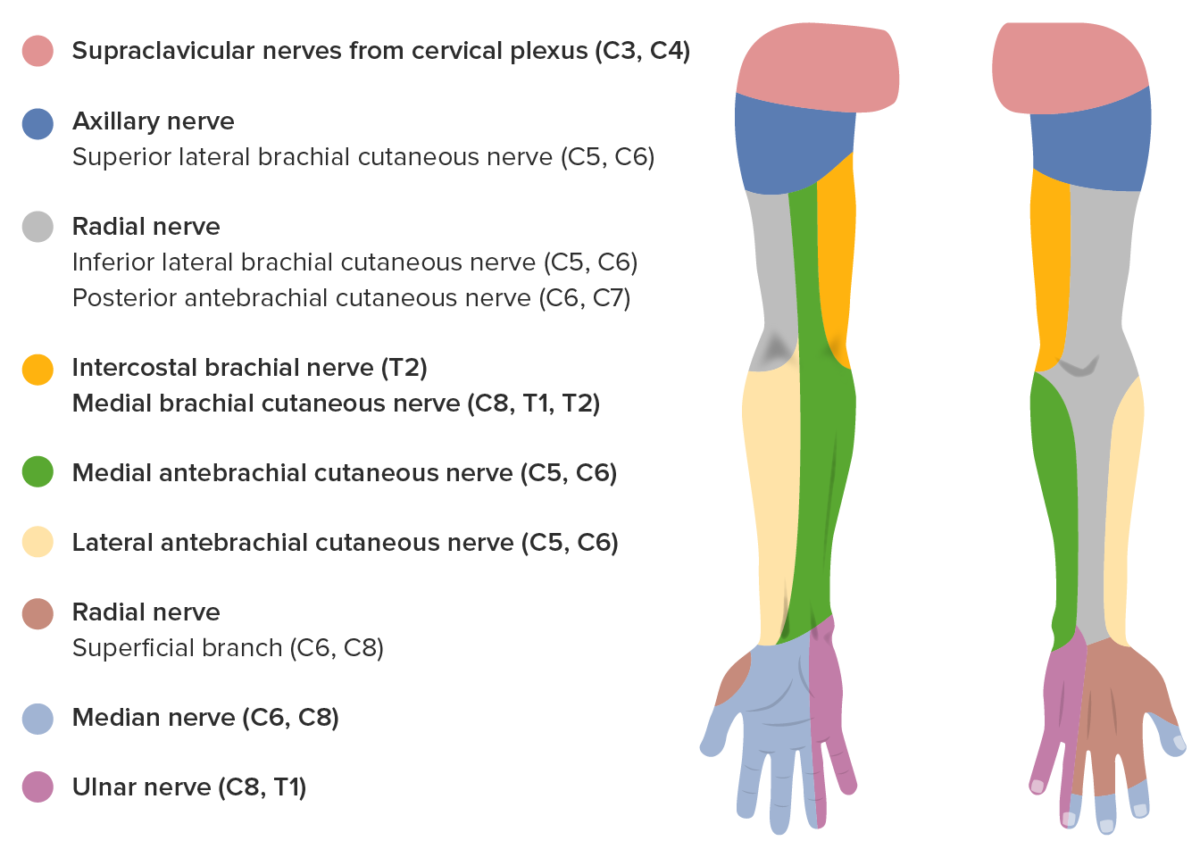
Sensory innervation of the median nerve
Image by Lecturio.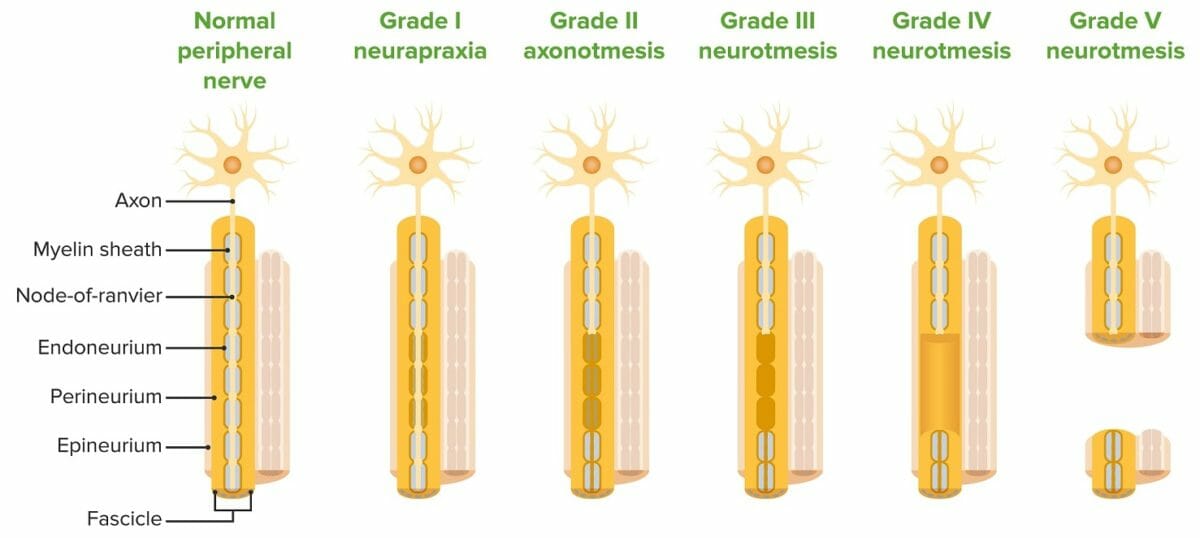
Sunderland classification of nerve injuries
Image by Lecturio.Peripheral nerve damage affecting the upper extremities is a common occupational injury that can also occur in individuals who participate in recreational sports. Several mechanisms are involved in nerve injury Nerve Injury Surgical Complications.
The axillary nerve Axillary nerve Axilla and Brachial Plexus: Anatomy carries cutaneous sensory Sensory Neurons which conduct nerve impulses to the central nervous system. Nervous System: Histology fibers to the area over the lateral shoulder and innervates the deltoid muscle for shoulder abduction Abduction Examination of the Upper Limbs and teres minor for external rotation External Rotation Examination of the Upper Limbs.
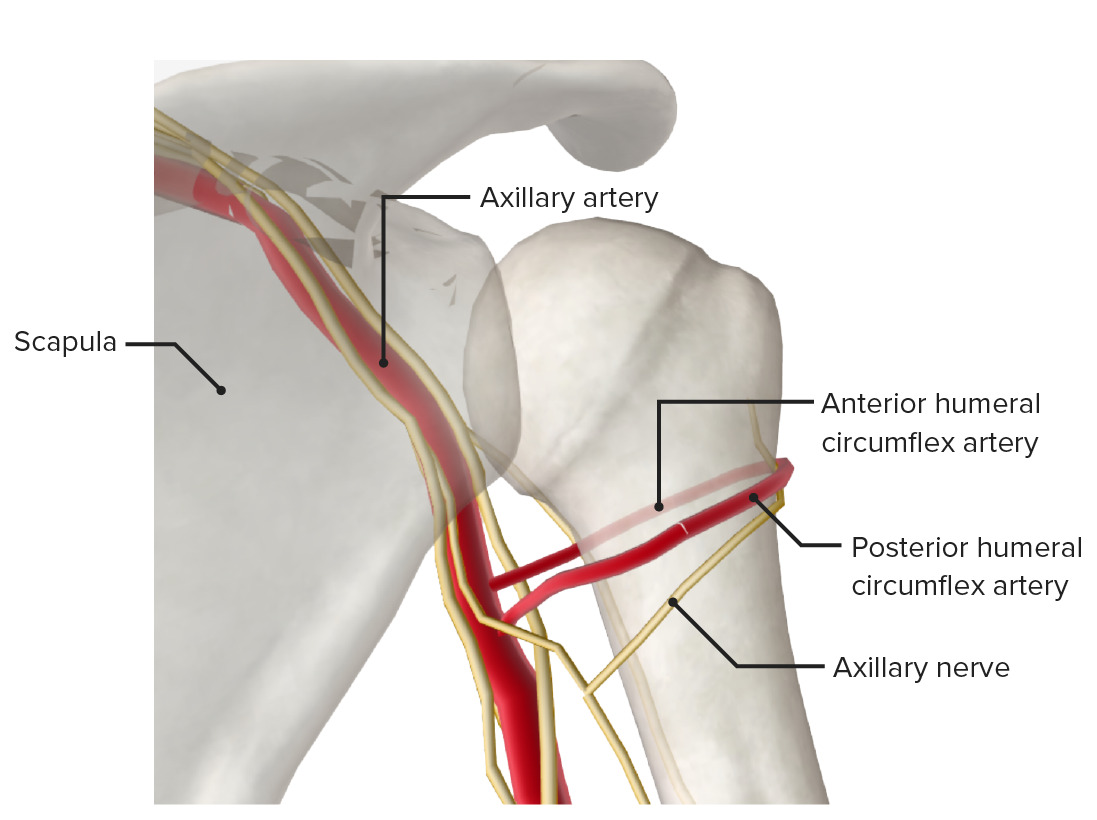
Posterior view of the proximal end of the humerus featuring the surgical neck, a frequent site of fracture:
A fracture at the site may injure the axillary nerve and/or posterior circumflex artery.
The musculocutaneous nerve Musculocutaneous Nerve A major nerve of the upper extremity. The fibers of the musculocutaneous nerve originate in the lower cervical spinal cord (usually C5 to C7), travel via the lateral cord of the brachial plexus, and supply sensory and motor innervation to the upper arm, elbow, and forearm. Axilla and Brachial Plexus: Anatomy arises from the lateral cord of the brachial plexus Brachial Plexus The large network of nerve fibers which distributes the innervation of the upper extremity. The brachial plexus extends from the neck into the axilla. In humans, the nerves of the plexus usually originate from the lower cervical and the first thoracic spinal cord segments (c5-c8 and T1), but variations are not uncommon. Peripheral Nerve Injuries in the Cervicothoracic Region and contains fibers from the C5, C6, and C7 nerve roots. The musculocutaneous nerve Musculocutaneous Nerve A major nerve of the upper extremity. The fibers of the musculocutaneous nerve originate in the lower cervical spinal cord (usually C5 to C7), travel via the lateral cord of the brachial plexus, and supply sensory and motor innervation to the upper arm, elbow, and forearm. Axilla and Brachial Plexus: Anatomy innervates the coracobrachialis Coracobrachialis Arm: Anatomy, biceps Biceps Arm: Anatomy, and brachialis Brachialis Arm: Anatomy muscles and provides sensation to the lateral forearm Forearm The forearm is the region of the upper limb between the elbow and the wrist. The term “forearm” is used in anatomy to distinguish this area from the arm, a term that is commonly used to describe the entire upper limb. The forearm consists of 2 long bones (the radius and the ulna), the interosseous membrane, and multiple arteries, nerves, and muscles. Forearm: Anatomy via the lateral cutaneous nerve.
The median nerve Median Nerve A major nerve of the upper extremity. In humans, the fibers of the median nerve originate in the lower cervical and upper thoracic spinal cord (usually C6 to T1), travel via the brachial plexus, and supply sensory and motor innervation to parts of the forearm and hand. Cubital Fossa: Anatomy innervates the flexor muscles of the forearm Forearm The forearm is the region of the upper limb between the elbow and the wrist. The term “forearm” is used in anatomy to distinguish this area from the arm, a term that is commonly used to describe the entire upper limb. The forearm consists of 2 long bones (the radius and the ulna), the interosseous membrane, and multiple arteries, nerves, and muscles. Forearm: Anatomy (except the flexor carpi ulnaris Flexor carpi ulnaris Forearm: Anatomy and ulnar head of the flexor digitorum profundus Flexor digitorum profundus Forearm: Anatomy (FDP)), the thenar muscles Thenar muscles Hand: Anatomy, and the 2 radial lumbricals Lumbricals Hand: Anatomy in the hand Hand The hand constitutes the distal part of the upper limb and provides the fine, precise movements needed in activities of daily living. It consists of 5 metacarpal bones and 14 phalanges, as well as numerous muscles innervated by the median and ulnar nerves. Hand: Anatomy. The median nerve Median Nerve A major nerve of the upper extremity. In humans, the fibers of the median nerve originate in the lower cervical and upper thoracic spinal cord (usually C6 to T1), travel via the brachial plexus, and supply sensory and motor innervation to parts of the forearm and hand. Cubital Fossa: Anatomy supplies sensation to the thumb, index, middle, and lateral half of the 4th fingers.
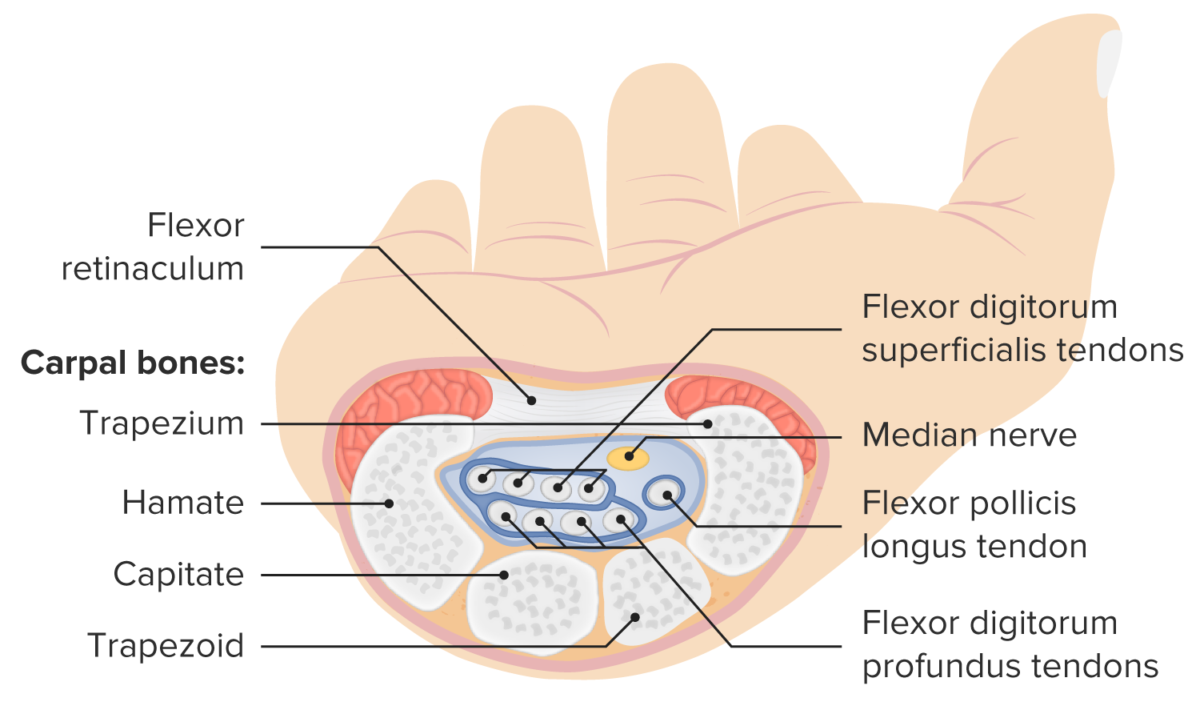
Structure and contents of the carpal tunnel
Image by Lecturio.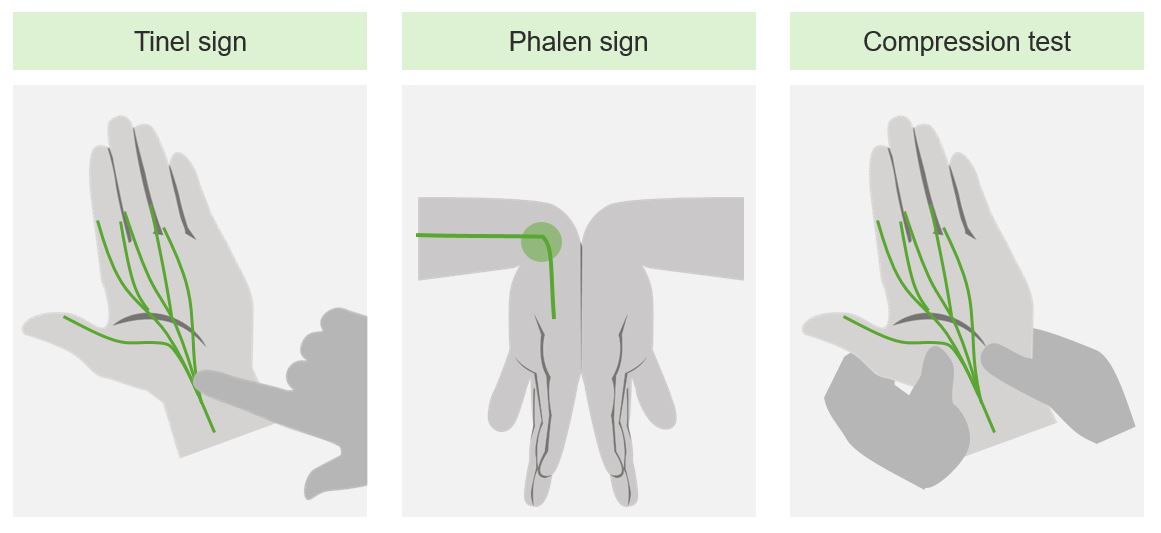
Provocative maneuvers for clinical evaluation of carpal tunnel syndrome
Image by Lecturio.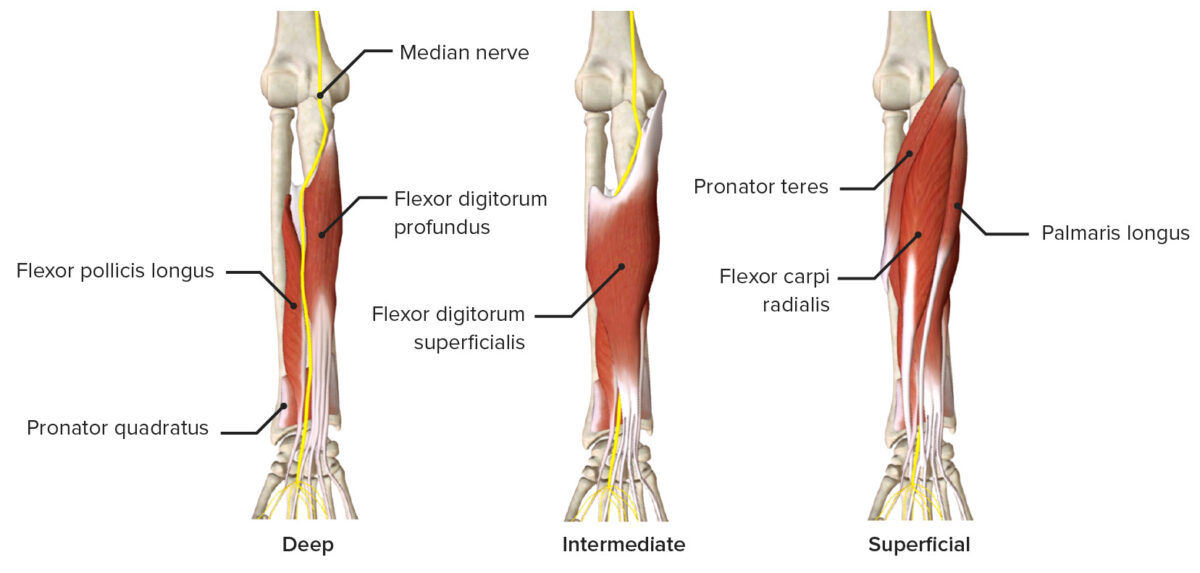
Median nerve passing through the anterior forearm, featuring the innervated muscles
Image by BioDigital, edited by Lecturio.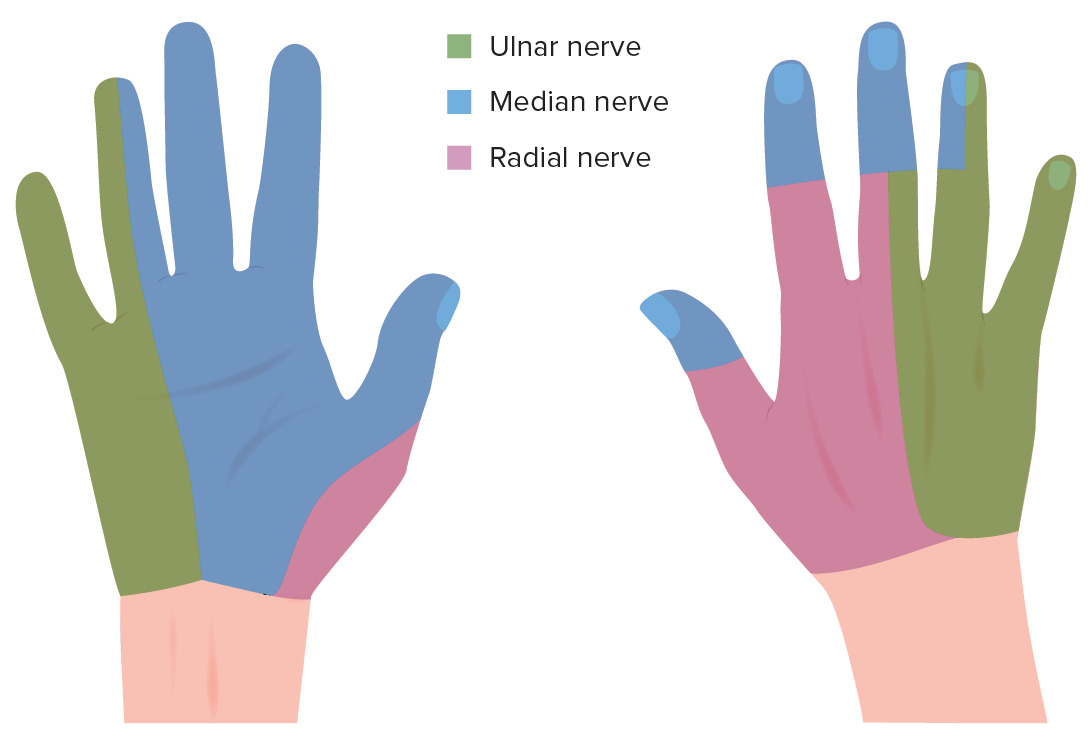
Sensory innervation of the hand
Image by Lecturio.Ulnar neuropathy Neuropathy Leprosy at the elbow is the 2nd-most diagnosed focal neuropathy Neuropathy Leprosy. The incidence Incidence The number of new cases of a given disease during a given period in a specified population. It also is used for the rate at which new events occur in a defined population. It is differentiated from prevalence, which refers to all cases in the population at a given time. Measures of Disease Frequency of ulnar neuropathy Neuropathy Leprosy at the wrist is much lower than that at the elbow, but can be caused by injury at either location.
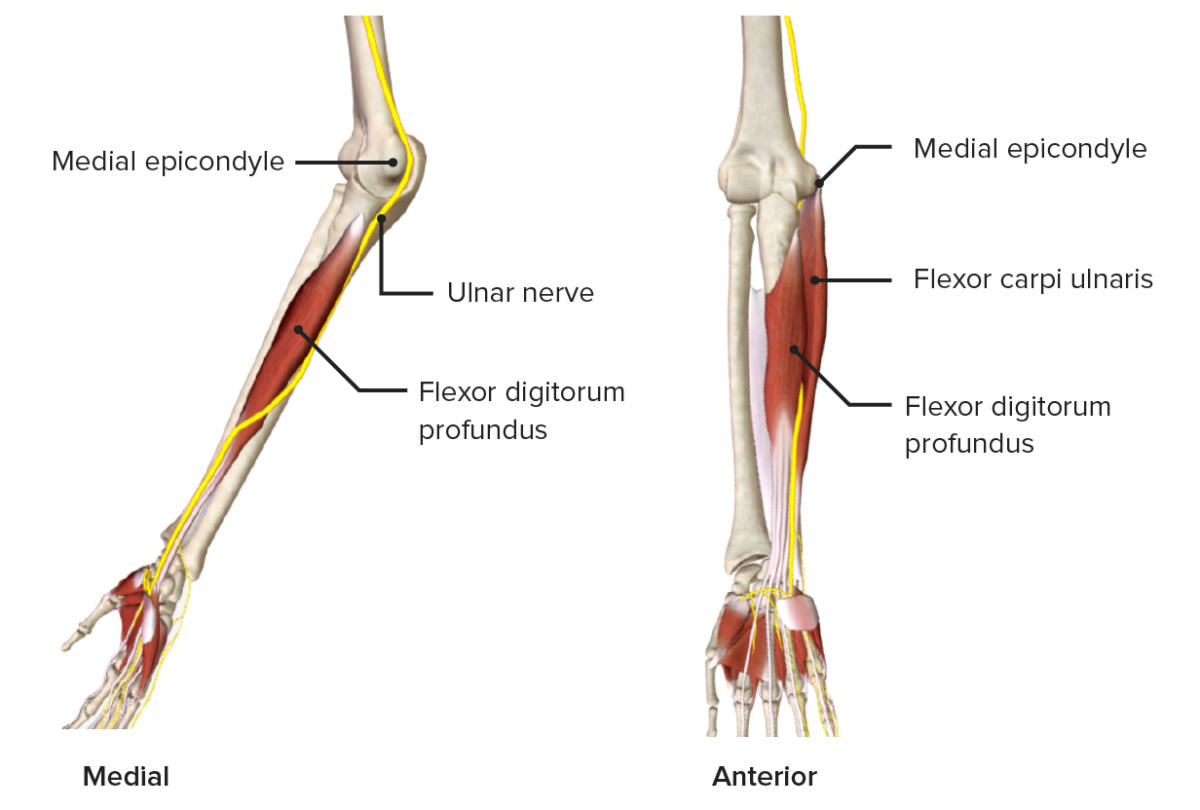
Ulnar nerve passing through the medial aspect of the forearm
Image by BioDigital, edited by Lecturio.
“Claw hand” due to ulnar nerve damage, resulting in atrophy and contractions on the denervated intrinsic hand muscles
Image: “Photograph of a healthy hand imitating an ulnar claw” by Mcstrother. License: CC BY 3.0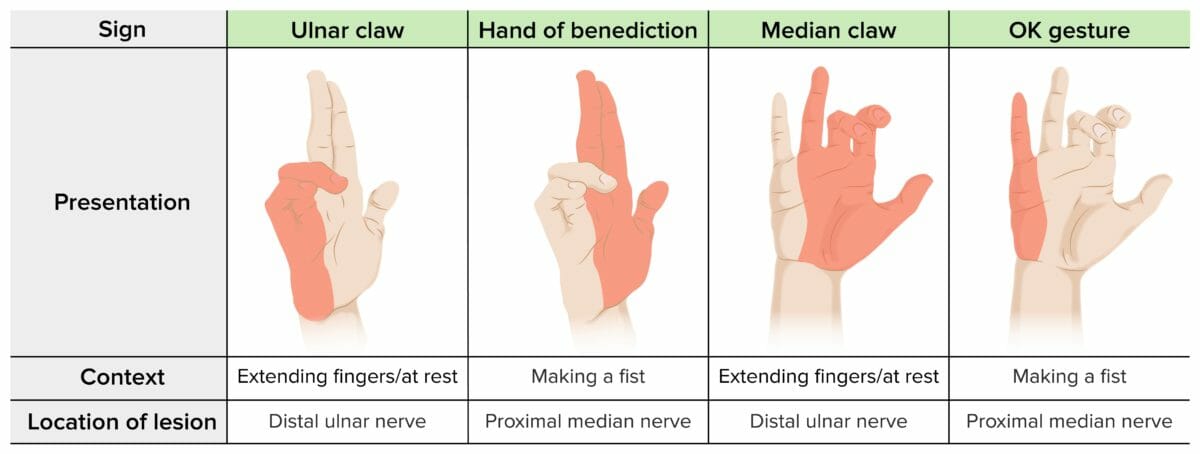
Hand distortions in nerve injuries
Image by Lecturio.The radial nerve Radial Nerve A major nerve of the upper extremity. In humans the fibers of the radial nerve originate in the lower cervical and upper thoracic spinal cord (usually C5 to T1), travel via the posterior cord of the brachial plexus, and supply motor innervation to extensor muscles of the arm and cutaneous sensory fibers to extensor regions of the arm and hand. Axilla and Brachial Plexus: Anatomy is particularly predisposed to compression Compression Blunt Chest Trauma in the spiral groove Spiral groove Arm: Anatomy, where it runs adjacent to the humerus Humerus Bone in humans and primates extending from the shoulder joint to the elbow joint. Arm: Anatomy. The radial nerve Radial Nerve A major nerve of the upper extremity. In humans the fibers of the radial nerve originate in the lower cervical and upper thoracic spinal cord (usually C5 to T1), travel via the posterior cord of the brachial plexus, and supply motor innervation to extensor muscles of the arm and cutaneous sensory fibers to extensor regions of the arm and hand. Axilla and Brachial Plexus: Anatomy provides motor Motor Neurons which send impulses peripherally to activate muscles or secretory cells. Nervous System: Histology innervation to the extensors of the forearm Forearm The forearm is the region of the upper limb between the elbow and the wrist. The term “forearm” is used in anatomy to distinguish this area from the arm, a term that is commonly used to describe the entire upper limb. The forearm consists of 2 long bones (the radius and the ulna), the interosseous membrane, and multiple arteries, nerves, and muscles. Forearm: Anatomy and extrinsic extensors of the wrists and hands, as well as sensation to the lateral half of the back of the hand Hand The hand constitutes the distal part of the upper limb and provides the fine, precise movements needed in activities of daily living. It consists of 5 metacarpal bones and 14 phalanges, as well as numerous muscles innervated by the median and ulnar nerves. Hand: Anatomy.
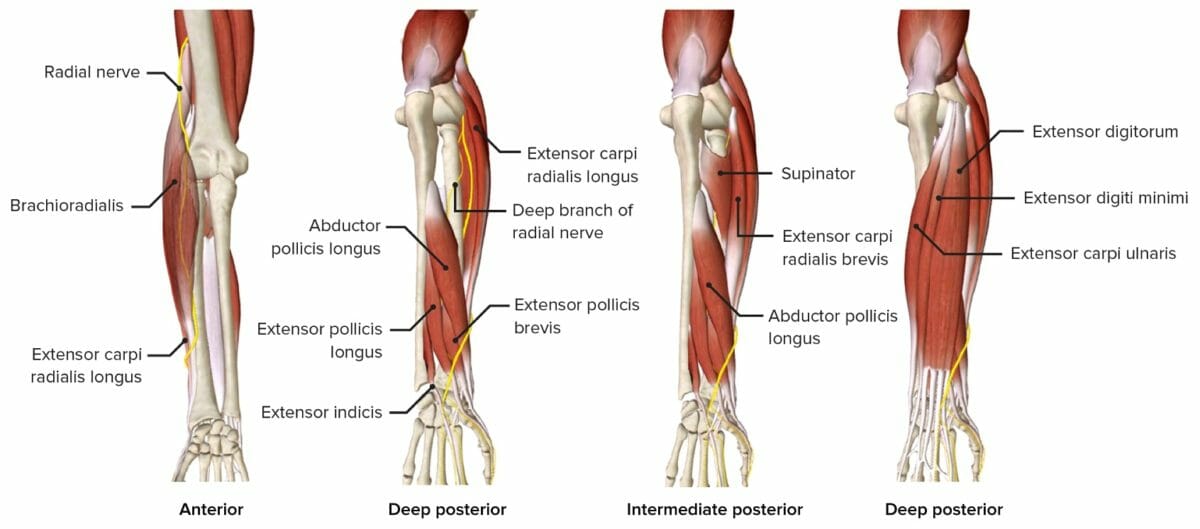
Radial nerve passing through the forearm, featuring the innervated muscles
Image by BioDigital, edited by Lecturio.