Transplantation is a procedure that involves the removal of an organ or living tissue and placing it into a different part of the body or into a different person. Organ transplantations have become the therapeutic option of choice for many individuals with end-stage organ failure. Transplantation can offer the individual a definitive treatment for a given disease entity. Over the past half-century, organ transplantation has become a successful and evolving practice which provides benefit to over 100,000 individuals yearly worldwide. Both solid organs and bone marrow Bone marrow The soft tissue filling the cavities of bones. Bone marrow exists in two types, yellow and red. Yellow marrow is found in the large cavities of large bones and consists mostly of fat cells and a few primitive blood cells. Red marrow is a hematopoietic tissue and is the site of production of erythrocytes and granular leukocytes. Bone marrow is made up of a framework of connective tissue containing branching fibers with the frame being filled with marrow cells. Bone Marrow: Composition and Hematopoiesis–derived hematopoietic cells can be successfully transplanted for a number of different indications. Tolerance Tolerance Pharmacokinetics and Pharmacodynamics of the transplanted organ by the immune system Immune system The body's defense mechanism against foreign organisms or substances and deviant native cells. It includes the humoral immune response and the cell-mediated response and consists of a complex of interrelated cellular, molecular, and genetic components. Primary Lymphatic Organs of the host is achieved through the use of immunosuppressive and immunomodulating strategies. The main complications of transplantation are organ rejection or graft failure; however, chronic immunosuppression also carries the risk of serious complications, including potentially life-threatening infections Infections Invasion of the host organism by microorganisms or their toxins or by parasites that can cause pathological conditions or diseases. Chronic Granulomatous Disease.
Last updated: Dec 5, 2024
Transplanted tissue may be cells (e.g., hematopoietic stem cells Hematopoietic stem cells Progenitor cells from which all blood cells derived. They are found primarily in the bone marrow and also in small numbers in the peripheral blood. Bone Marrow: Composition and Hematopoiesis), tissues (e.g., cornea Cornea The transparent anterior portion of the fibrous coat of the eye consisting of five layers: stratified squamous corneal epithelium; bowman membrane; corneal stroma; descemet membrane; and mesenchymal corneal endothelium. It serves as the first refracting medium of the eye. Eye: Anatomy), parts of an organ (e.g., liver Liver The liver is the largest gland in the human body. The liver is found in the superior right quadrant of the abdomen and weighs approximately 1.5 kilograms. Its main functions are detoxification, metabolism, nutrient storage (e.g., iron and vitamins), synthesis of coagulation factors, formation of bile, filtration, and storage of blood. Liver: Anatomy and skin Skin The skin, also referred to as the integumentary system, is the largest organ of the body. The skin is primarily composed of the epidermis (outer layer) and dermis (deep layer). The epidermis is primarily composed of keratinocytes that undergo rapid turnover, while the dermis contains dense layers of connective tissue. Skin: Structure and Functions grafts), or entire organs (e.g., kidney, heart). There are many terms that are important to transplant medicine.
Immunologic matching between an organ donor and an organ recipient is important to improve the success of a transplantation and to reduce the risk of rejection. HLA tissue typing is important for the transplantation of hematopoietic stem cells Hematopoietic stem cells Progenitor cells from which all blood cells derived. They are found primarily in the bone marrow and also in small numbers in the peripheral blood. Bone Marrow: Composition and Hematopoiesis and solid organs, including kidney, heart, liver Liver The liver is the largest gland in the human body. The liver is found in the superior right quadrant of the abdomen and weighs approximately 1.5 kilograms. Its main functions are detoxification, metabolism, nutrient storage (e.g., iron and vitamins), synthesis of coagulation factors, formation of bile, filtration, and storage of blood. Liver: Anatomy, pancreas Pancreas The pancreas lies mostly posterior to the stomach and extends across the posterior abdominal wall from the duodenum on the right to the spleen on the left. This organ has both exocrine and endocrine tissue. Pancreas: Anatomy, and lung transplants.
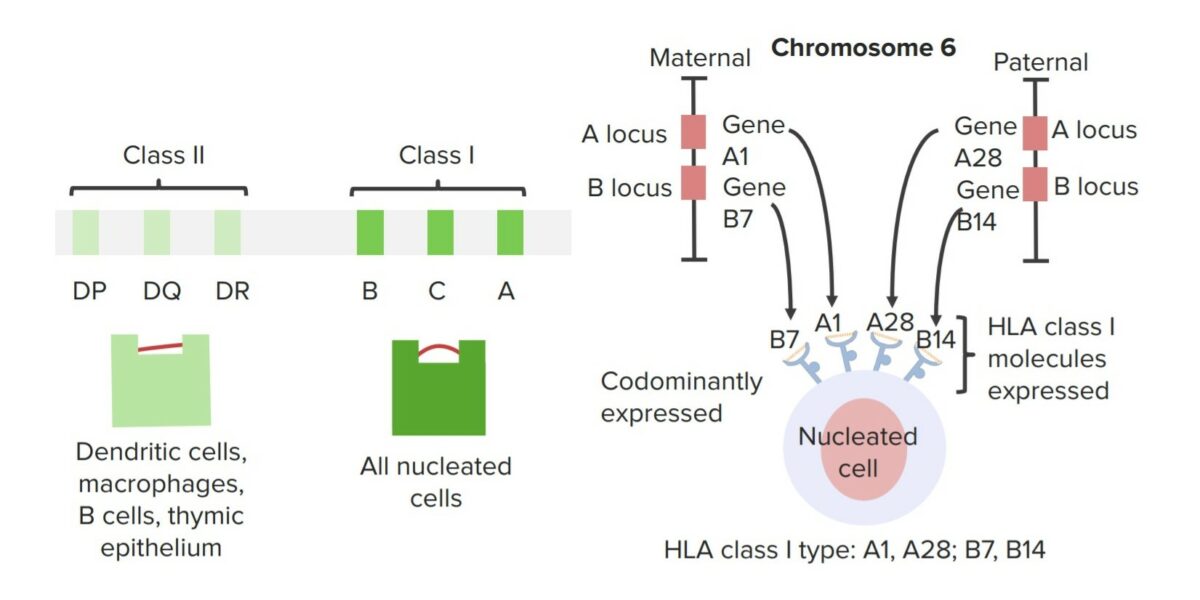
Major histocompatibility complex
Image by Lecturio.Rejection may be acute or chronic, and the symptoms vary by organ system.
| Rejection | Time after transplantation | Characteristics of rejection |
|---|---|---|
| Hyperacute | Within 48 hours |
|
| Accelerated | 3–5 days |
|
| Acute | > 5 days |
|
| Chronic | Months to years |
|
Recipients of solid organ transplants must take immunosuppressive drugs to prevent rejection of the graft. Current immunosuppressive drugs target T-cell activation and cytokine production, clonal expansion Clonal Expansion Seborrheic Keratosis of T cells T cells Lymphocytes responsible for cell-mediated immunity. Two types have been identified – cytotoxic (t-lymphocytes, cytotoxic) and helper T-lymphocytes (t-lymphocytes, helper-inducer). They are formed when lymphocytes circulate through the thymus gland and differentiate to thymocytes. When exposed to an antigen, they divide rapidly and produce large numbers of new T cells sensitized to that antigen. T cells: Types and Functions, or both.
The scarcity of organs from donors is a significant factor in liver transplantation Liver transplantation The transference of a part of or an entire liver from one human or animal to another. Hepatocellular Carcinoma (HCC) and Liver Metastases; many individuals die while waiting for an organ. Living-donor transplants are now used, in which only a portion of the liver Liver The liver is the largest gland in the human body. The liver is found in the superior right quadrant of the abdomen and weighs approximately 1.5 kilograms. Its main functions are detoxification, metabolism, nutrient storage (e.g., iron and vitamins), synthesis of coagulation factors, formation of bile, filtration, and storage of blood. Liver: Anatomy is removed from a healthy donor.
Complications:
Complications of immunosuppression:
Immunizations for posttransplant/immunosuppressed individuals:
Rejection:
Other complications:
Heart transplantation may be offered to individuals who have intolerable symptoms despite optimal medical therapy and who are at risk of death due to cardiac disease.