An embolus is an intravascular solid, liquid, or gaseous material that is carried by the blood to a site distant from its point of origin. Emboli of all types warrant immediate medical attention Attention Focusing on certain aspects of current experience to the exclusion of others. It is the act of heeding or taking notice or concentrating. Psychiatric Assessment. The majority of emboli dislodge from a thrombus, forming a thromboembolus. Other less common nonthrombotic types of emboli are cholesterol Cholesterol The principal sterol of all higher animals, distributed in body tissues, especially the brain and spinal cord, and in animal fats and oils. Cholesterol Metabolism, fat, air, amniotic fluid Amniotic fluid A clear, yellowish liquid that envelopes the fetus inside the sac of amnion. In the first trimester, it is likely a transudate of maternal or fetal plasma. In the second trimester, amniotic fluid derives primarily from fetal lung and kidney. Cells or substances in this fluid can be removed for prenatal diagnostic tests (amniocentesis). Placenta, Umbilical Cord, and Amniotic Cavity, and tumor Tumor Inflammation emboli. The cause of the embolus depends on the type, as does the clinical presentation, diagnosis, and management of each embolic condition. Due to their effects on circulation Circulation The movement of the blood as it is pumped through the cardiovascular system. ABCDE Assessment, all emboli have the potential to result in end-organ failure and death.
Last updated: Mar 29, 2023
The classic presentation includes skin Skin The skin, also referred to as the integumentary system, is the largest organ of the body. The skin is primarily composed of the epidermis (outer layer) and dermis (deep layer). The epidermis is primarily composed of keratinocytes that undergo rapid turnover, while the dermis contains dense layers of connective tissue. Skin: Structure and Functions findings, abdominal pain Abdominal Pain Acute Abdomen, and progressive renal failure Renal failure Conditions in which the kidneys perform below the normal level in the ability to remove wastes, concentrate urine, and maintain electrolyte balance; blood pressure; and calcium metabolism. Renal insufficiency can be classified by the degree of kidney damage (as measured by the level of proteinuria) and reduction in glomerular filtration rate. Crush Syndrome following a vascular procedure. Neurological and ocular symptoms are also common if the emboli travel superiorly.

Livedo reticularis of left leg
Image: “Livedo reticularis of left leg” by Texas Tech University Health Sciences Center, Lubbock, TX, USA. License: CC BY 3.0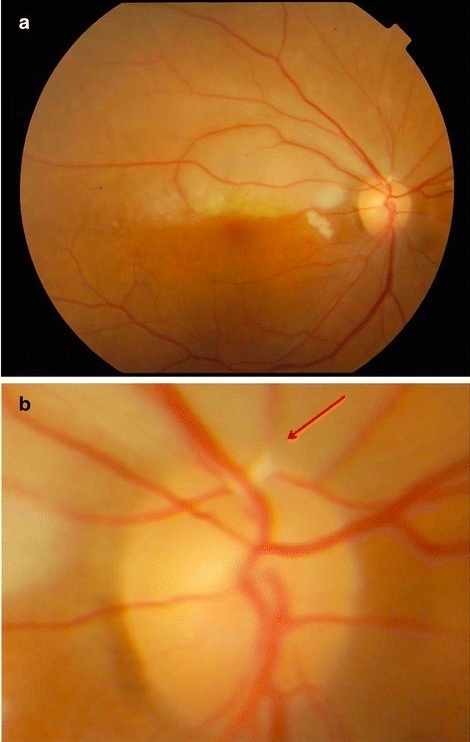
a: photo of the fundus showing a pale retina superiorly
b: close-up view of the optic disc from the above image showing a Hollenhorst plaque in the superotemporal vessel (arrow)
The diagnosis is usually clinical. Definitive diagnosis requires a biopsy Biopsy Removal and pathologic examination of specimens from the living body. Ewing Sarcoma.
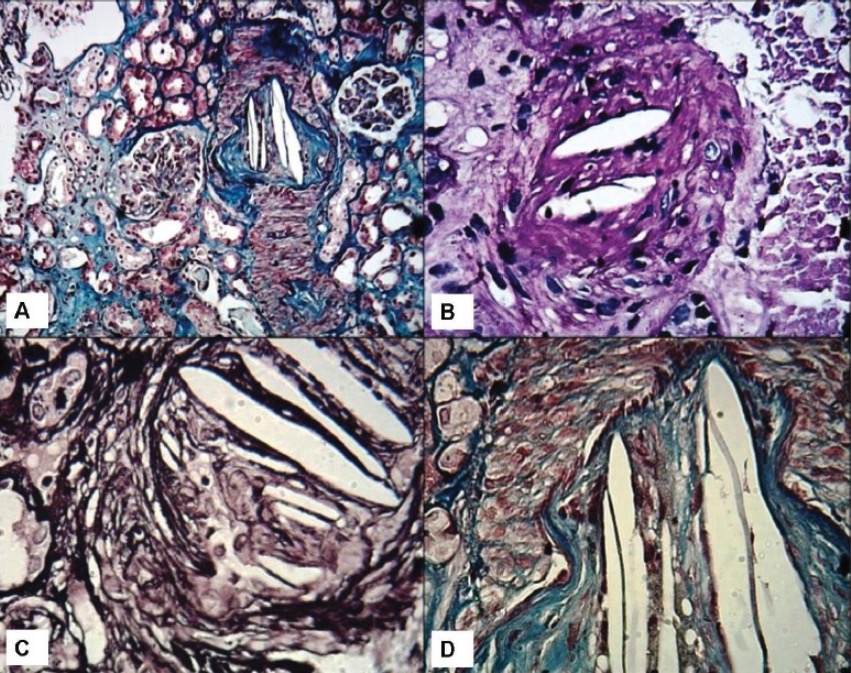
Kidney biopsies showing cholesterol clefts:
A: Low-power view showing an interlobular artery with luminal occlusion and needle-like crystals in the lumina. Two glomeruli are seen in the vicinity with minor changes on light microscopy. Mild patchy tubular atrophy is seen (Masson’s trichrome stain, ×100).
B: Medium-power view showing a small artery with luminal cholesterol clefts causing luminal occlusion (Periodic acid-Schiff stain, ×200).
C: High-power view showing typical empty-looking and needle-like cholesterol clefts in the lumina (Jones methenamine silver stain, ×400).
D: High-power view showing luminal cholesterol clefts and intimal fibrosis. Media appears red on this stain (Masson’s trichrome stain, ×400).
Pathogenesis may be by 1 or both of the following mechanisms:
Signs and symptoms typically develop 24–72 hours after the inciting event.
Fat embolism is usually a clinical diagnosis after excluding other possibilities.
An air embolism occurs when gas bubbles enter the circulation Circulation The movement of the blood as it is pumped through the cardiovascular system. ABCDE Assessment and block blood flow Blood flow Blood flow refers to the movement of a certain volume of blood through the vasculature over a given unit of time (e.g., mL per minute). Vascular Resistance, Flow, and Mean Arterial Pressure.
| Etiology | Examples |
|---|---|
| Surgical procedures |
|
| IV catheterization |
|
| Trauma |
|
| Pulmonary barotrauma Barotrauma Injury following pressure changes; includes injury to the eustachian tube, ear drum, lung and stomach. Invasive Mechanical Ventilation |
|
Presentation depends on the site and size of the embolism.
Venous air embolism → air travels to the right ventricle → pulmonary circulation Circulation The movement of the blood as it is pumped through the cardiovascular system. ABCDE Assessment:
Arterial air embolism → air travels to end organs → ischemia Ischemia A hypoperfusion of the blood through an organ or tissue caused by a pathologic constriction or obstruction of its blood vessels, or an absence of blood circulation. Ischemic Cell Damage:
Diagnosis is made by determining air in the intravascular space or organs of a patient with known risk factors. However, air is often rapidly reabsorbed and no longer present by the time the patient undergoes diagnostic testing; thus, the diagnosis is often made clinically.
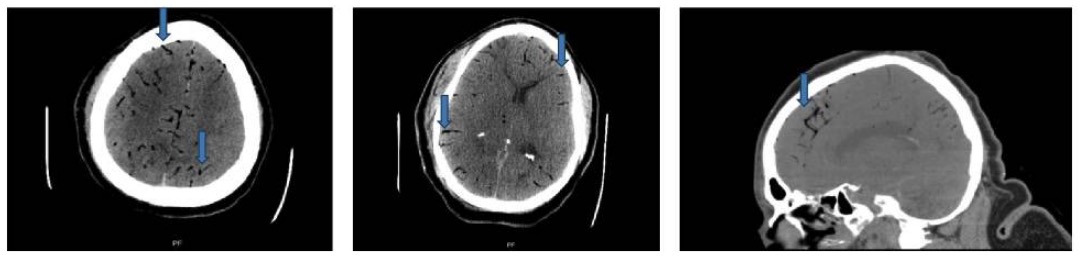
CT scan of head: axial and sagittal cuts showing foci of gas in bilateral cerebral arteries (blue arrows)
Image: “Case 2 CT scan of head” by Rashmi Mishra et al. License: CC BY 4.0Stabilize the patient:
Repositioning:
Definitive therapies:

Hyperbaric oxygen therapy chamber
Image: “Hyperbaric oxygen therapy chamber” by Mark Murphy. License: Public DomainAmniotic fluid embolism Amniotic Fluid Embolism Blocking of maternal circulation by amniotic fluid that is forced into uterine veins by strong uterine contraction near the end of pregnancy. It is characterized by the sudden onset of severe respiratory distress and hypotension that can lead to maternal death. Complications during Childbirth ( AFE AFE Blocking of maternal circulation by amniotic fluid that is forced into uterine veins by strong uterine contraction near the end of pregnancy. It is characterized by the sudden onset of severe respiratory distress and hypotension that can lead to maternal death. Complications during Childbirth) is a complication during labor and the immediate postpartum period Postpartum period In females, the period that is shortly after giving birth (parturition). Postpartum Complications.
AFE AFE Blocking of maternal circulation by amniotic fluid that is forced into uterine veins by strong uterine contraction near the end of pregnancy. It is characterized by the sudden onset of severe respiratory distress and hypotension that can lead to maternal death. Complications during Childbirth typically presents dramatically, as sudden-onset cardiopulmonary collapse occurring during labor or within 30 minutes after delivery.
AFE AFE Blocking of maternal circulation by amniotic fluid that is forced into uterine veins by strong uterine contraction near the end of pregnancy. It is characterized by the sudden onset of severe respiratory distress and hypotension that can lead to maternal death. Complications during Childbirth is a clinical diagnosis based on presentation.

Chest X-ray of a patient with amniotic fluid embolism:
Diffuse infiltration is observed throughout the lungs.
Survival depends on prompt diagnosis and effective resuscitation Resuscitation The restoration to life or consciousness of one apparently dead. . Neonatal Respiratory Distress Syndrome.
| Type of embolism | Most common clinical presentations | Management |
|---|---|---|
| Cholesterol Cholesterol The principal sterol of all higher animals, distributed in body tissues, especially the brain and spinal cord, and in animal fats and oils. Cholesterol Metabolism embolism | From thoracic sources:
|
Focus on risk reduction in atherosclerotic disease:
|
| Fat embolism | From orthopedic trauma:
|
Supportive care |
| Air embolism | From:
|
|
| Amniotic fluid embolism Amniotic Fluid Embolism Blocking of maternal circulation by amniotic fluid that is forced into uterine veins by strong uterine contraction near the end of pregnancy. It is characterized by the sudden onset of severe respiratory distress and hypotension that can lead to maternal death. Complications during Childbirth | During labor or within 30 minutes of delivery:
|
|
| Tumor Tumor Inflammation embolism | From any end-stage malignancy Malignancy Hemothorax: |
|