The menisci are fibrocartilaginous wedge-shaped structures between the distal femur and proximal tibia Tibia The second longest bone of the skeleton. It is located on the medial side of the lower leg, articulating with the fibula laterally, the talus distally, and the femur proximally. Knee Joint: Anatomy that stabilize and dissipate weight-bearing forces at the knee joint Knee joint The knee joint is made up of the articulations between the femur, tibia, and patella bones, and is one of the largest and most complex joints of the human body. The knee is classified as a synovial hinge joint, which primarily allows for flexion and extension with a more limited degree of translation and rotation. Knee Joint: Anatomy. A meniscus tear is an injury to the meniscus caused by rotational or shearing forces Shearing forces Vascular Resistance, Flow, and Mean Arterial Pressure across the tibiofemoral joint Tibiofemoral joint Knee Joint: Anatomy. Clinical presentation in a young patient with a traumatic tear includes a history of a twisting or rotational injury followed by pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways at the joint line with a small effusion. Clinical presentation in an older patient includes weight-bearing pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways at the joint line that mimics and accompanies progressive pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways due to the degenerative changes Degenerative Changes Spinal Stenosis of osteoarthritis Osteoarthritis Osteoarthritis (OA) is the most common form of arthritis, and is due to cartilage destruction and changes of the subchondral bone. The risk of developing this disorder increases with age, obesity, and repetitive joint use or trauma. Patients develop gradual joint pain, stiffness lasting < 30 minutes, and decreased range of motion. Osteoarthritis. Mechanical complaints (e.g., joint locking, catching, or clicking) are also common. Diagnosis can be challenging clinically and is often confirmed by diagnostic imaging or by direct visualization ( arthroscopy Arthroscopy Endoscopic examination, therapy and surgery of the joint. Knee Ligament Injuries). Management can be conservative or surgical, depending on the individual situation.
Last updated: Mar 29, 2023
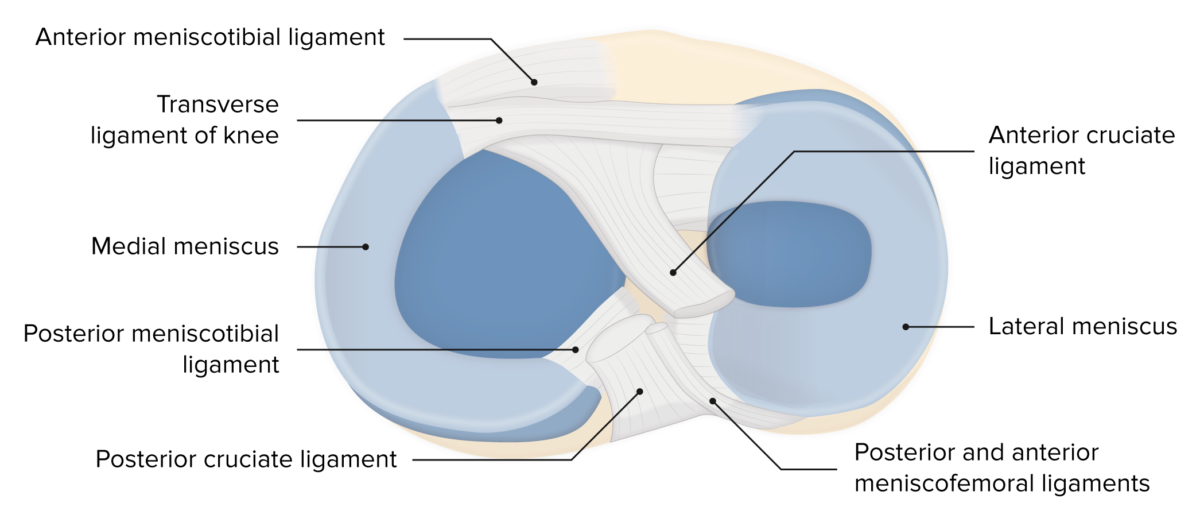
Menisci of the knee
Image by Lecturio. License: CC BY-NC-SA 4.0There are several types of tear patterns in meniscal tears:
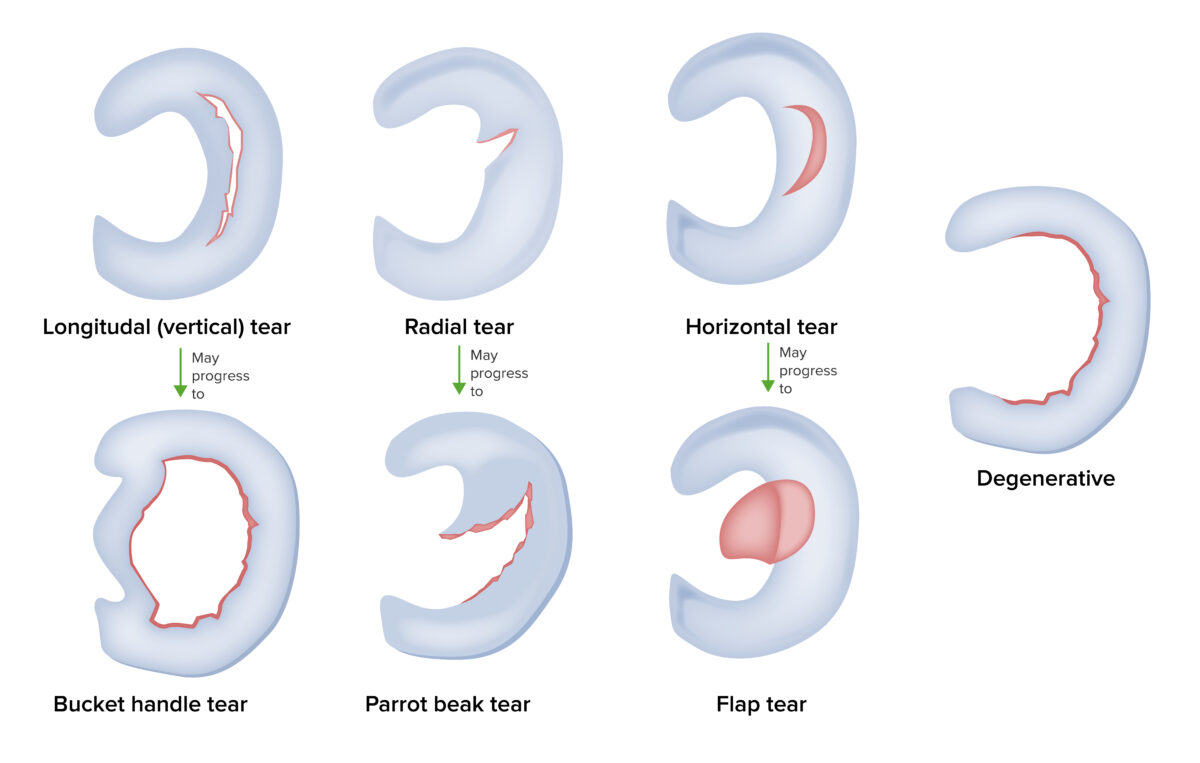
Types of meniscus tears
Image by Lecturio.Clinical anatomy:
Traumatic mechanisms for tears:

Thessaly test
Image by Lecturio.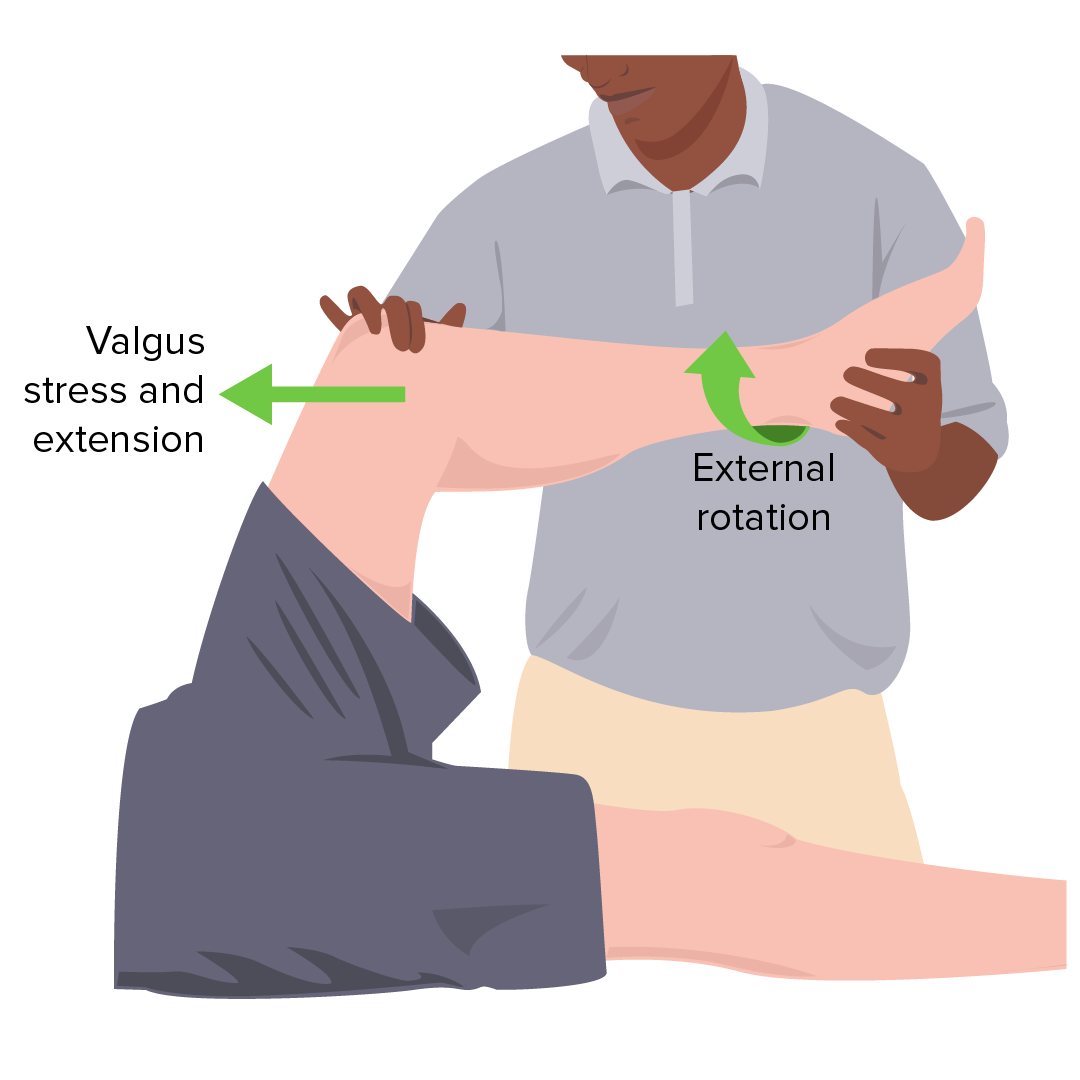
McMurray test
Image by Lecturio.Diagnosis is usually suspected with a thorough history and physical examination, and often confirmed with diagnostic imaging (e.g., MRI) or by direct visualization (e.g., arthroscopy Arthroscopy Endoscopic examination, therapy and surgery of the joint. Knee Ligament Injuries).
X-ray X-ray Penetrating electromagnetic radiation emitted when the inner orbital electrons of an atom are excited and release radiant energy. X-ray wavelengths range from 1 pm to 10 nm. Hard x-rays are the higher energy, shorter wavelength x-rays. Soft x-rays or grenz rays are less energetic and longer in wavelength. The short wavelength end of the x-ray spectrum overlaps the gamma rays wavelength range. The distinction between gamma rays and x-rays is based on their radiation source. Pulmonary Function Tests:
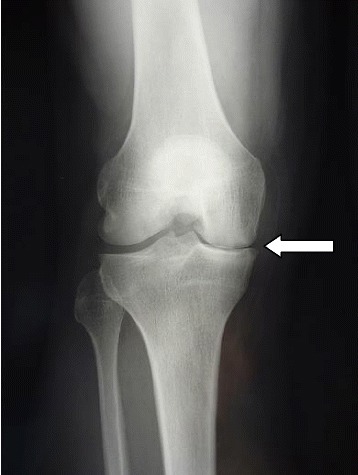
X-ray demonstrating medial joint space narrowing
Image: “Postoperative radiography at 3 month follow-up” by Steinmetz S, Bonnomet F, Rahme M, Adam P, Ehlinger M. License: CC BY 4.0Ultrasound:
MRI:

MRI of the right knee revealing intra-articular and bucket-handle medial meniscus tear with the displaced fragment located in the intercondylar notch
Image: “Coronal MRI of the right knee” by Ahmed Ali R, McKay S. License: CC BY 3.0
MRI of the knee showing horizontal tear (white arrow) at the posterior horn of medial meniscus
Image: “A sagittal T2-weighted MRI shows horizontal tear” by Journal of Orthopaedic Surgery and Research. License: CC BY 4.0Arthroscopy Arthroscopy Endoscopic examination, therapy and surgery of the joint. Knee Ligament Injuries:
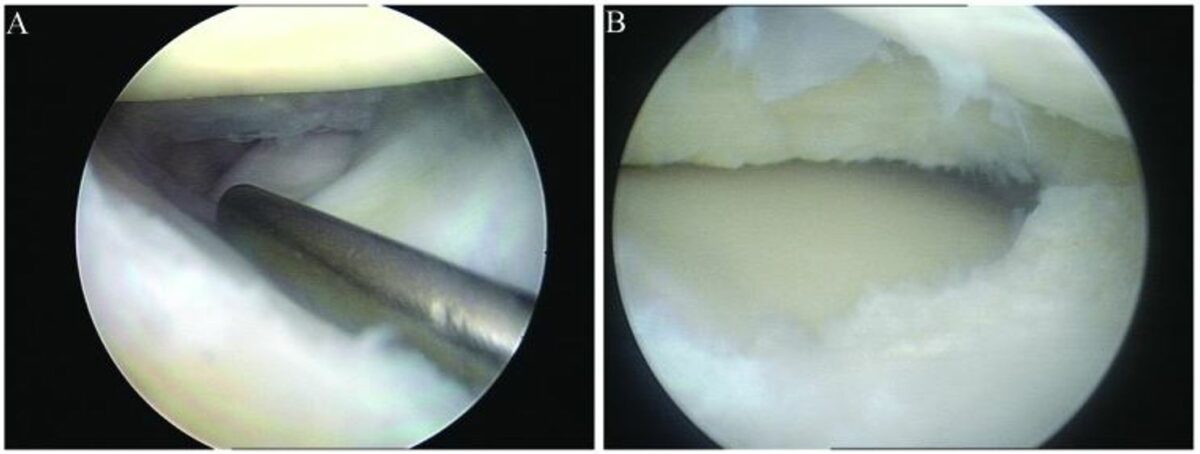
Arthroscopy with arthroscopic meniscus repair:
A: discoid lateral meniscus with longitudinal tear
B: discoid lateral meniscus following partial resection
Management of meniscal tears is dependent on the type of tear, age of the patient, occupation of the patient, associated mechanical symptoms, and other associated injuries (e.g., ACL tear ACL tear Knee Pain).
Conservative management indicated as initial treatment in degenerative tears in older patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship or prior to arthroscopy Arthroscopy Endoscopic examination, therapy and surgery of the joint. Knee Ligament Injuries in younger patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship:

Arthroscopy surgical positioning
Image: “The position for viewing the medial meniscus in right knee” by Gupta Y, Mahara DP, Lamichhane AP. License: CC BY 4.0
Medial meniscus fold as seen through anterolateral portal
Image: “Appearance of medial meniscus flounce” by Gupta Y, Mahara DP, Lamichhane AP. License: CC BY 4.0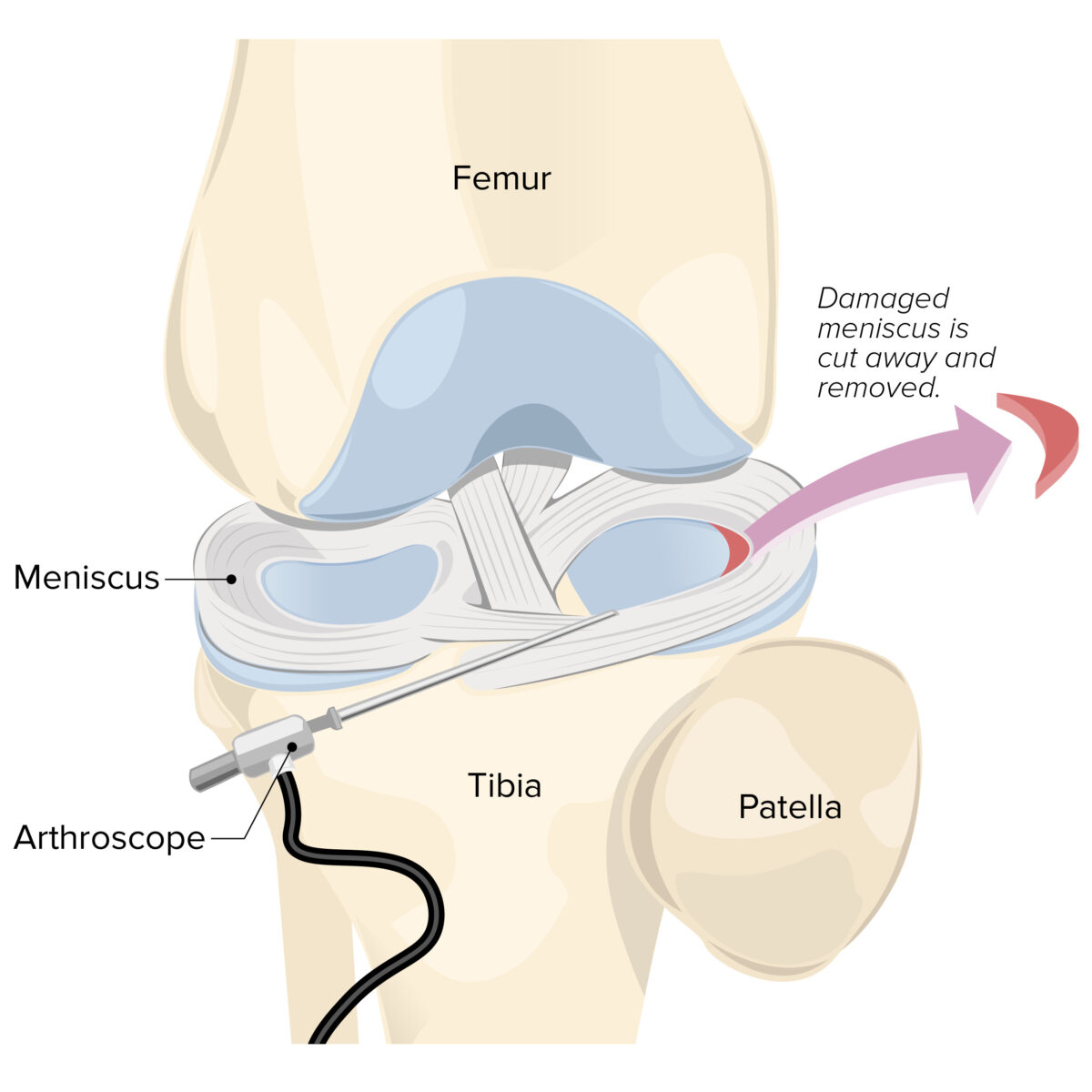
Knee arthroscopy with meniscectomy
Image by Lecturio.Long-term outcomes depend on: