Advertisement
Advertisement
Advertisement
Advertisement
Lyme disease is a tick-borne infection caused by the gram-negative spirochete Spirochete Treponema is a gram-negative, microaerophilic spirochete. Owing to its very thin structure, it is not easily seen on Gram stain, but can be visualized using dark-field microscopy. This spirochete contains endoflagella, which allow for a characteristic corkscrew movement. Treponema Borrelia burgdorferi Borrelia burgdorferi A specific species of bacteria, part of the borrelia burgdorferi group, whose common name is lyme disease spirochete. Borrelia. Lyme disease is transmitted by the black-legged Ixodes tick (commonly known as a deer tick Deer tick Borrelia), which is only found in specific geographic regions. Patient presentation can vary depending on the stage of the disease and may include a characteristic erythema Erythema Redness of the skin produced by congestion of the capillaries. This condition may result from a variety of disease processes. Chalazion migrans rash Rash Rocky Mountain Spotted Fever. Neurologic, cardiac, ocular, and joint manifestations are also common in later stages. Diagnosis relies on clinical findings and tick exposure, and is supported by serological testing. Antibiotics are used for treatment. Avoidance of tick exposure is key to prevention in endemic areas.
Last updated: Nov 7, 2022
Advertisement
Advertisement
Advertisement
Advertisement
Advertisement
Advertisement
Advertisement
Advertisement
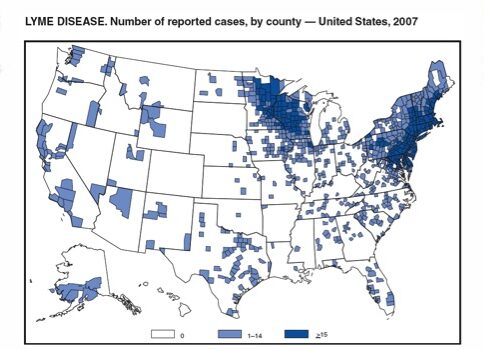
The majority of Lyme disease cases are reported in Northeastern and upper Midwestern regions in the United States, according to the Centers for Disease Control and Prevention (CDC) in 2017.
Image: “Lyme disease reported cases” by CDC. License: Public Domain
The black-legged tick (Ixodes scapularis) is the primary vector for Lyme disease.
Image: “The blacklegged tick” by Liza Gross. License: CC BY 2.5The incubation Incubation The amount time between exposure to an infectious agent and becoming symptomatic. Rabies Virus period for Lyme disease is 3–30 days (mean of 7 days). The clinical manifestations of Lyme disease are broken down into 3 stages: early localized disease, early disseminated disease, and late disease.
Symptoms appear in 1–5 weeks and resolve in approximately 30 days.
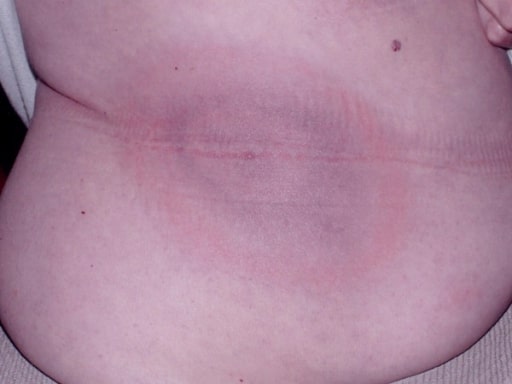
The classic “bull’s-eye” (erythema migrans) rash of Borrelia burgdorferi
Image: “Classic bull’s eye EM” by Department of Medicine, Johns Hopkins School of Medicine, Baltimore, Maryland, USA. License: CC BY 2.0
Erythema migrans
Image by James Gathany. License: Public DomainSymptoms develop in weeks to months in untreated patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship.
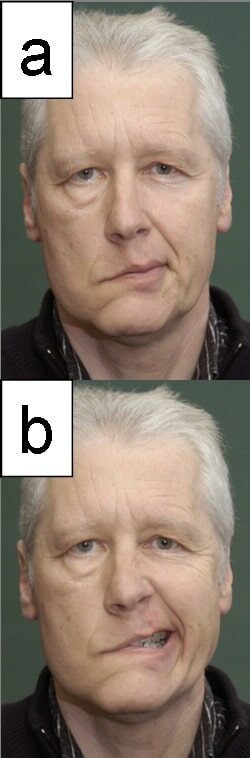
A patient with facial nerve palsy: This is the most common neurologic manifestation of Lyme disease.
Image: “Facial palsy” by Department of Otorhinolarnygology, University Jena, Lessingstrasse 2, Jena, Germany. License: CC BY 2.0
Lymphadenosis cutis benigna, also known as a lymphocytoma, of a patient’s ear: This is a rare cutaneous finding in early disseminated Lyme disease.
Image: “ Lymphocytoma” by Department of General and Visceral Surgery, Augusta Kranken Anstalt, Academic Teaching Hospital of the Ruhr-University Bochum, Germany. License: CC BY 2.0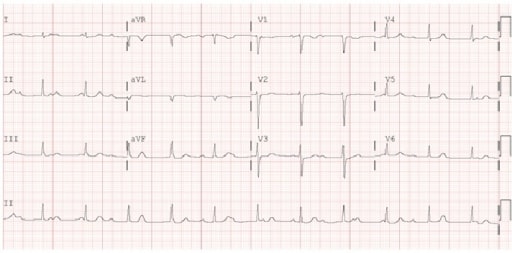
Electrocardiogram (ECG) demonstrating 3rd-degree atrioventricular block: This is 1 of the cardiac manifestations of early disseminated Lyme disease.
Image: “ Electrocardiogram” by Maxwell Eyram Afari et al. License: CC BY 4.0Symptoms develop in months to years in untreated patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship.

Bilateral knee swelling and arthritis in a pediatric patient with Lyme disease
Image: “Bilateral knee arthritis” by Krzysztof Orczyk et al. License: CC BY 4.0
Acrodermatitis chronica atrophicans
Image: “Acrodermatitis chronica atrophicans” by Giuseppe Stinco et al. License: CC BY 3.0Common symptoms of Lyme disease can be remembered by the mnemonic phrase “a key Lyme pie to the FACE.”
Laboratory tests are only significant in conjunction with the clinical history due to a high false-positive and false-negative rate.
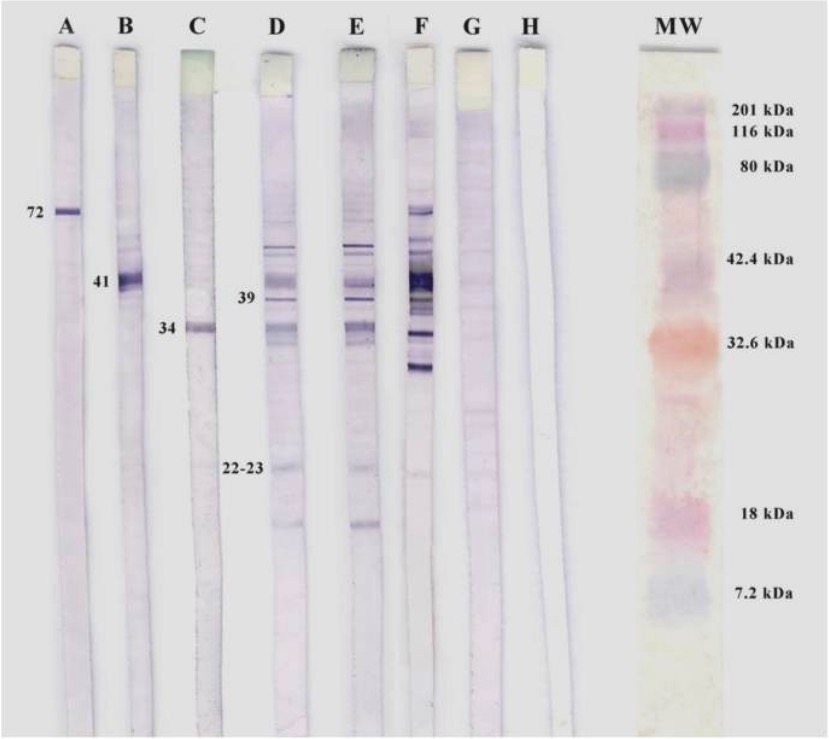
Western blotting of B. burgdorferi.
A, B, and C: positive controls for specific monoclonal antibodies
D and E: seropositive patients for IgM
F: positive control
G: negative control
H: white control
MW: molecular weight
Oral antibiotics:
Intravenous (IV) antibiotics:
Additional considerations:
| Clinical manifestations | Management |
|---|---|
Asymptomatic patient with a tick bite requires no prophylactic treatment unless:
|
If meets criteria, then must receive prophylactic doxycycline within 72 hours of bite |
| Erythema Erythema Redness of the skin produced by congestion of the capillaries. This condition may result from a variety of disease processes. Chalazion migrans (localized disease) |
|
| Early disseminated disease: |
|
|
|
| Cardiac and severe neurologic manifestations | Intravenous ceftriaxone Ceftriaxone A broad-spectrum cephalosporin antibiotic and cefotaxime derivative with a very long half-life and high penetrability to meninges, eyes and inner ears. Cephalosporins |
Late disease:
|
|
| Reinfection | Same antibiotic as recommended for a primary infection Primary infection Herpes Simplex Virus 1 and 2 |
Doxycycline prophylaxis Prophylaxis Cephalosporins is indicated if all the following criteria are met MET Preoperative Care: