Glycogen storage disorders (GSDs) are genetic defects leading to disorders of carbohydrate metabolism. The disorders are caused by pathogenic variants in genes Genes A category of nucleic acid sequences that function as units of heredity and which code for the basic instructions for the development, reproduction, and maintenance of organisms. DNA Types and Structure that affect enzymes Enzymes Enzymes are complex protein biocatalysts that accelerate chemical reactions without being consumed by them. Due to the body's constant metabolic needs, the absence of enzymes would make life unsustainable, as reactions would occur too slowly without these molecules. Basics of Enzymes involved in glycogen breakdown. Deficiency of 1 of these enzymes Enzymes Enzymes are complex protein biocatalysts that accelerate chemical reactions without being consumed by them. Due to the body's constant metabolic needs, the absence of enzymes would make life unsustainable, as reactions would occur too slowly without these molecules. Basics of Enzymes may occur in the liver Liver The liver is the largest gland in the human body. The liver is found in the superior right quadrant of the abdomen and weighs approximately 1.5 kilograms. Its main functions are detoxification, metabolism, nutrient storage (e.g., iron and vitamins), synthesis of coagulation factors, formation of bile, filtration, and storage of blood. Liver: Anatomy or muscles and can cause hypoglycemia Hypoglycemia Hypoglycemia is an emergency condition defined as a serum glucose level ≤ 70 mg/dL (≤ 3.9 mmol/L) in diabetic patients. In nondiabetic patients, there is no specific or defined limit for normal serum glucose levels, and hypoglycemia is defined mainly by its clinical features. Hypoglycemia and/or abnormal glycogen deposition in tissues. Presentations vary from being fatal in the neonatal period to having their initial presentation with symptoms in adulthood. There are at least 14 types of GSDs, and the 4 most common and significant are von Gierke disease, Pompe disease, Cori disease, and McArdle disease. Diagnosis is clinical; detection of glycogen in tissues is by biopsy Biopsy Removal and pathologic examination of specimens from the living body. Ewing Sarcoma and confirmed by DNA analysis DNA analysis Biochemical identification of mutational changes in a nucleotide sequence. Hyper-IgM Syndrome. Management aims to treat or avoid hypoglycemia Hypoglycemia Hypoglycemia is an emergency condition defined as a serum glucose level ≤ 70 mg/dL (≤ 3.9 mmol/L) in diabetic patients. In nondiabetic patients, there is no specific or defined limit for normal serum glucose levels, and hypoglycemia is defined mainly by its clinical features. Hypoglycemia, hyperuricemia Hyperuricemia Excessive uric acid or urate in blood as defined by its solubility in plasma at 37 degrees c; greater than 0. 42 mmol per liter (7. 0 mg/dl) in men or 0. 36 mmol per liter (6. 0 mg/dl) in women. Gout, hyperlipidemia (HLD), and lactic acidosis Lactic Acidosis Oxazolidinones. No cure is currently available, but genetic therapies are being tested.
Last updated: Sep 12, 2022
Glycogen storage disorders (GSDs) are genetic defects causing enzyme deficiencies that result in liver Liver The liver is the largest gland in the human body. The liver is found in the superior right quadrant of the abdomen and weighs approximately 1.5 kilograms. Its main functions are detoxification, metabolism, nutrient storage (e.g., iron and vitamins), synthesis of coagulation factors, formation of bile, filtration, and storage of blood. Liver: Anatomy, muscle, or heart disease from abnormal glycogen deposition in tissues and episodic hypoglycemia Hypoglycemia Hypoglycemia is an emergency condition defined as a serum glucose level ≤ 70 mg/dL (≤ 3.9 mmol/L) in diabetic patients. In nondiabetic patients, there is no specific or defined limit for normal serum glucose levels, and hypoglycemia is defined mainly by its clinical features. Hypoglycemia (in most disorders), as the body cannot use glycogen as a source of energy.
Glycogen storage disorder I (von Gierke disease) is caused by mutations that lead to enzyme deficiencies; these result in excess glycogen and fat accumulation in tissues and hypoglycemia Hypoglycemia Hypoglycemia is an emergency condition defined as a serum glucose level ≤ 70 mg/dL (≤ 3.9 mmol/L) in diabetic patients. In nondiabetic patients, there is no specific or defined limit for normal serum glucose levels, and hypoglycemia is defined mainly by its clinical features. Hypoglycemia.
Glycogen storage disorder II (Pompe disease) is an autosomal recessive Autosomal recessive Autosomal inheritance, both dominant and recessive, refers to the transmission of genes from the 22 autosomal chromosomes. Autosomal recessive diseases are only expressed when 2 copies of the recessive allele are inherited. Autosomal Recessive and Autosomal Dominant Inheritance lysosomal storage disorder caused by a pathogenic variant in GAA. The defect results in an enzyme deficiency of alpha-glucosidase, with subsequent glycogen accumulation Glycogen Accumulation Cellular Accumulations in cardiac and skeletal muscle.
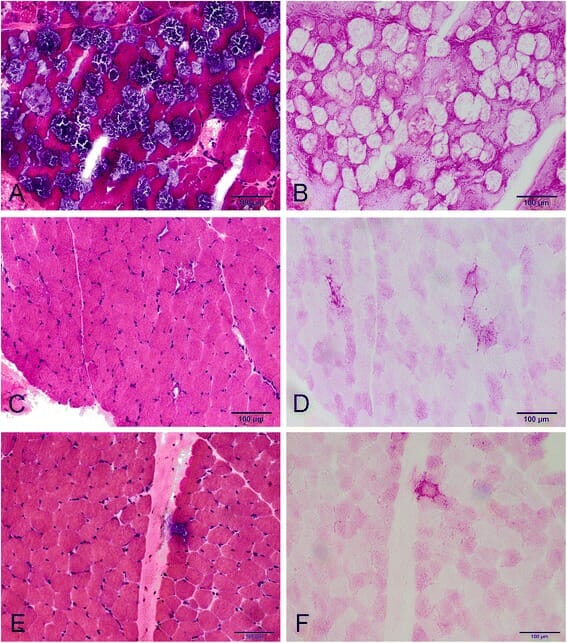
Myopathic changes with late-onset Pompe disease:
A: H&E staining—extensive vacuolation in many fibers.
C and E: H&E staining—vacuolation in only a few fibers in a different patient.
B, D, and F: PAS staining—vacuolar fibers stained positive for glycogen.
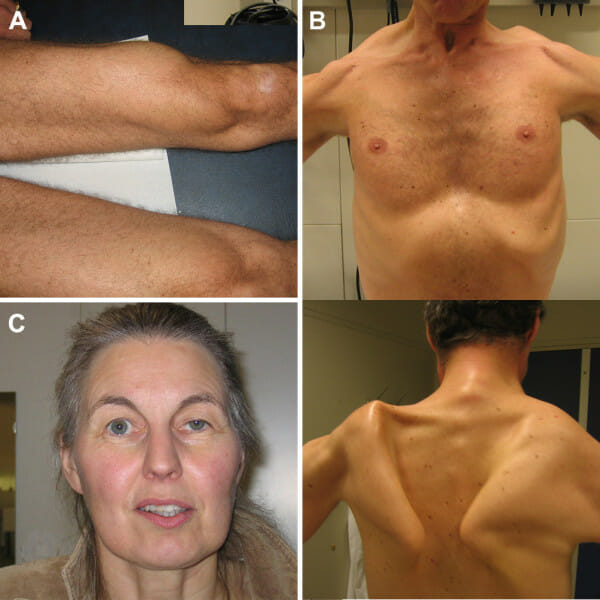
Clinical features in Pompe disease:
Atrophy of the quadriceps muscle (A), scapular winging (B), and ptosis (C) as notable clinical features in adults with Pompe disease. Photographs are printed with permission of the patients.
Glycogen storage disorder III (Cori disease) is caused by a deficiency in glycogen debranching enzymes Enzymes Enzymes are complex protein biocatalysts that accelerate chemical reactions without being consumed by them. Due to the body’s constant metabolic needs, the absence of enzymes would make life unsustainable, as reactions would occur too slowly without these molecules. Basics of Enzymes and leads to glycogen deposition in the liver Liver The liver is the largest gland in the human body. The liver is found in the superior right quadrant of the abdomen and weighs approximately 1.5 kilograms. Its main functions are detoxification, metabolism, nutrient storage (e.g., iron and vitamins), synthesis of coagulation factors, formation of bile, filtration, and storage of blood. Liver: Anatomy, muscle, and heart.
Glycogen storage disease Glycogen storage disease A group of inherited metabolic disorders involving the enzymes responsible for the synthesis and degradation of glycogen. In some patients, prominent liver involvement is presented. In others, more generalized storage of glycogen occurs, sometimes with prominent cardiac involvement. Benign Liver Tumors V (McArdle disease), also known as myophosphorylase deficiency, is an autosomal-recessive disorder caused by mutations in the muscle isoform of phosphorylase ( muscle glycogen Muscle glycogen Glycogen Metabolism phosphorylase, or PYGM) located at 11q13.
| von Gierke (GSD I) | Pompe (GSD II) | Cori (GSD III) | McArdle (GSD V) | |
|---|---|---|---|---|
| Presentation |
|
|
|
|
| Diagnosis |
|
|
|
|
| Management |
|
|
|
|