Fibromyalgia is a chronic pain Chronic pain Aching sensation that persists for more than a few months. It may or may not be associated with trauma or disease, and may persist after the initial injury has healed. Its localization, character, and timing are more vague than with acute pain. Pain Management syndrome characterized by widespread body pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways, chronic fatigue, mood disturbance, and cognitive disturbance. It also presents with other comorbid symptoms such as migraine Migraine Migraine headache is a primary headache disorder and is among the most prevalent disorders in the world. Migraine is characterized by episodic, moderate to severe headaches that may be associated with increased sensitivity to light and sound, as well as nausea and/or vomiting. Migraine Headache headaches, depression, sleep Sleep A readily reversible suspension of sensorimotor interaction with the environment, usually associated with recumbency and immobility. Physiology of Sleep disturbance, and irritable bowel syndrome Irritable bowel syndrome Irritable bowel syndrome (IBS) is a functional bowel disease characterized by chronic abdominal pain and altered bowel habits without an identifiable organic cause. The etiology and pathophysiology of this disease are not well understood, and there are many factors that may contribute. Irritable Bowel Syndrome. Diagnosis is clinical with laboratory exams and imaging reserved to rule out other causes for the spectrum of symptoms. Management is centered around education and lifestyle modification, with both pharmacotherapy (e.g., antidepressants, anticonvulsants) and non-pharmacotherapy (e.g., low-impact exercise, sleep Sleep A readily reversible suspension of sensorimotor interaction with the environment, usually associated with recumbency and immobility. Physiology of Sleep optimization, cognitive behavioral therapy Cognitive behavioral therapy A directive form of psychotherapy based on the interpretation of situations (cognitive structure of experiences) that determine how an individual feels and behaves. It is based on the premise that cognition, the process of acquiring knowledge and forming beliefs, is a primary determinant of mood and behavior. The therapy uses behavioral and verbal techniques to identify and correct negative thinking that is at the root of the aberrant behavior. Psychotherapy) showing efficacy.
Last updated: May 16, 2024
While the cause is unknown, the following environmental triggers have been associated with the onset of fibromyalgia.
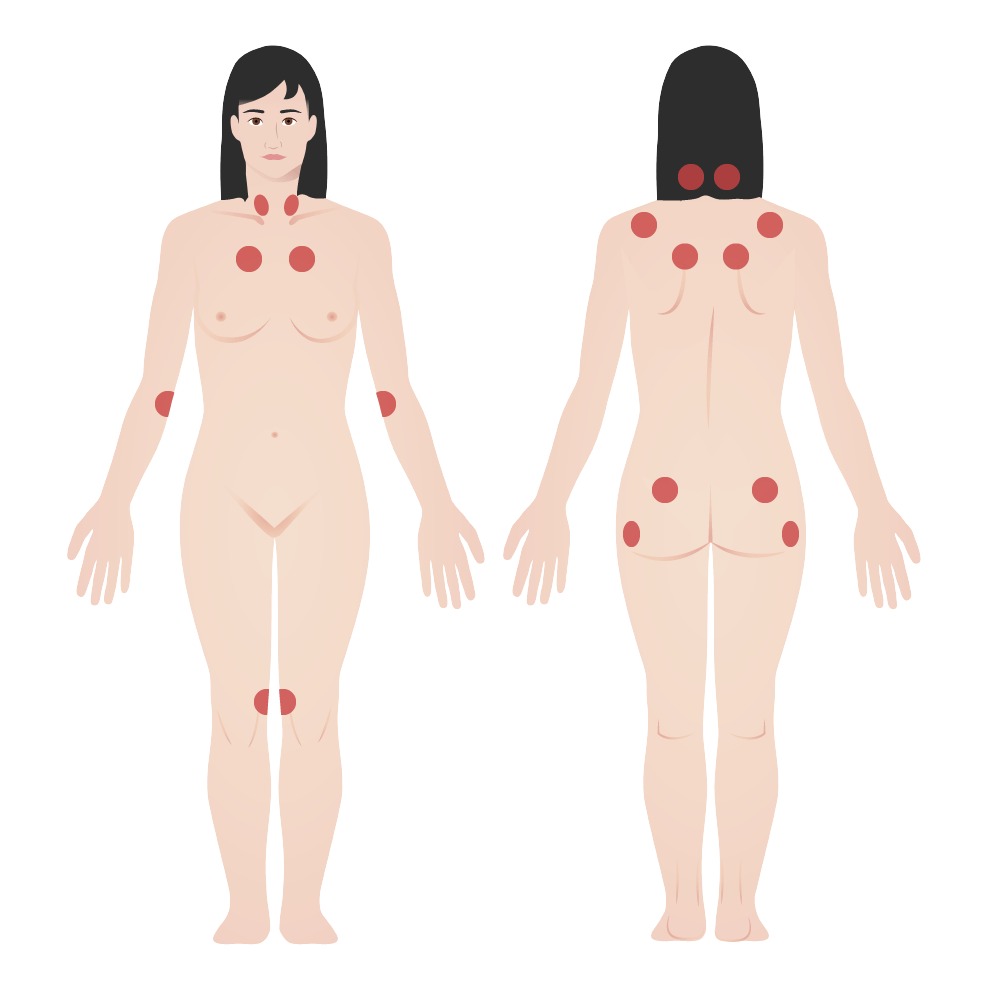
Fibromyalgia tender points:
The American College of Rheumatology diagnostic criteria for fibromyalgia was historically based on the presence of tender points.
Fibromyalgia is a chronic syndrome; therefore, diagnosis determination is recommended over multiple visits after sequential Sequential Computed Tomography (CT) observation and physical exams.
A history evaluation should include:
A physical examination should include:
An individual satisfies diagnostic criteria for fibromyalgia if the following 3 conditions are met MET Preoperative Care:
Widespread pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways index (each area is worth 1 point): score will be between 0 and 19.
Symptom severity scale Scale Dermatologic Examination score:
The SS SS Scleroderma (systemic sclerosis) is an autoimmune condition characterized by diffuse collagen deposition and fibrosis. The clinical presentation varies from limited skin involvement to diffuse involvement of internal organs. Scleroderma scale Scale Dermatologic Examination score is the sum of the severity of the 3 symptoms (fatigue, waking unrefreshed, cognitive symptoms) plus the extent (severity) of somatic symptoms Somatic symptoms Major Depressive Disorder in general. The final score is between 0 and 12. For each of the 3 symptoms, indicate the level of severity over the past week using the following scale Scale Dermatologic Examination:
Considering somatic symptoms Somatic symptoms Major Depressive Disorder in general, indicate whether the individual has:
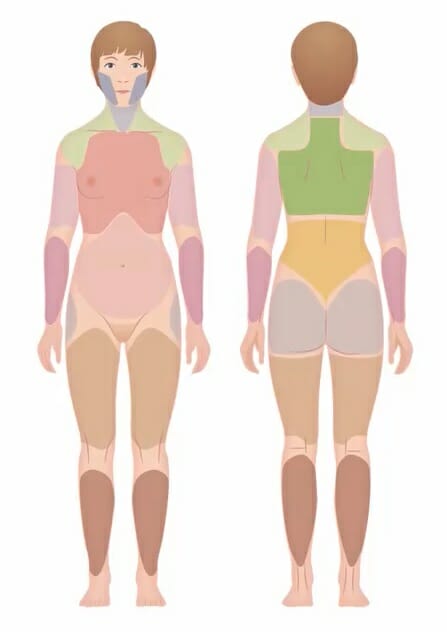
Widespread pain index:
A self-report assessment that identifies painful locations and the extent of symptoms, which has largely replaced the tender (trigger) point examination.