Crush syndrome encompasses the systemic manifestations that result from a crush (or traumatic compression Compression Blunt Chest Trauma) injury. Compartment syndrome Compartment Syndrome Compartment syndrome is a surgical emergency usually occurring secondary to trauma. The condition is marked by increased pressure within a compartment that compromises the circulation and function of the tissues within that space. Compartment Syndrome and/or rhabdomyolysis Rhabdomyolysis Rhabdomyolysis is characterized by muscle necrosis and the release of toxic intracellular contents, especially myoglobin, into the circulation. Rhabdomyolysis can also occur in crush syndrome. Systemic effects include the development of renal failure due to toxins released from damaged muscles, hypovolemia Hypovolemia Sepsis in Children, and acidosis Acidosis A pathologic condition of acid accumulation or depletion of base in the body. The two main types are respiratory acidosis and metabolic acidosis, due to metabolic acid build up. Respiratory Acidosis. Other features include arrhythmias from the electrolyte imbalances, ARDS from the inflammatory response, and disseminated intravascular coagulation Disseminated intravascular coagulation Disseminated intravascular coagulation (DIC) is a condition characterized by systemic bodywide activation of the coagulation cascade. This cascade results in both widespread microvascular thrombi contributing to multiple organ dysfunction and consumption of clotting factors and platelets, leading to hemorrhage. Disseminated Intravascular Coagulation from liberated thromboplastin. Field management with intravenous fluids Intravenous Fluids Intravenous fluids are one of the most common interventions administered in medicine to approximate physiologic bodily fluids. Intravenous fluids are divided into 2 categories: crystalloid and colloid solutions. Intravenous fluids have a wide variety of indications, including intravascular volume expansion, electrolyte manipulation, and maintenance fluids. Intravenous Fluids and extrication is crucial in reducing the risk of death. Inpatient care requires a multidisciplinary team focused on continued hydration, reducing complications or further injury, and determining the need for operative intervention.
Last updated: Jan 24, 2023
Crush syndrome is a condition of systemic manifestations (including shock Shock Shock is a life-threatening condition associated with impaired circulation that results in tissue hypoxia. The different types of shock are based on the underlying cause: distributive (↑ cardiac output (CO), ↓ systemic vascular resistance (SVR)), cardiogenic (↓ CO, ↑ SVR), hypovolemic (↓ CO, ↑ SVR), obstructive (↓ CO), and mixed. Types of Shock and renal failure) that develop from high-degree crush injury or traumatic compression Compression Blunt Chest Trauma of the torso, extremities, or other parts of the body.
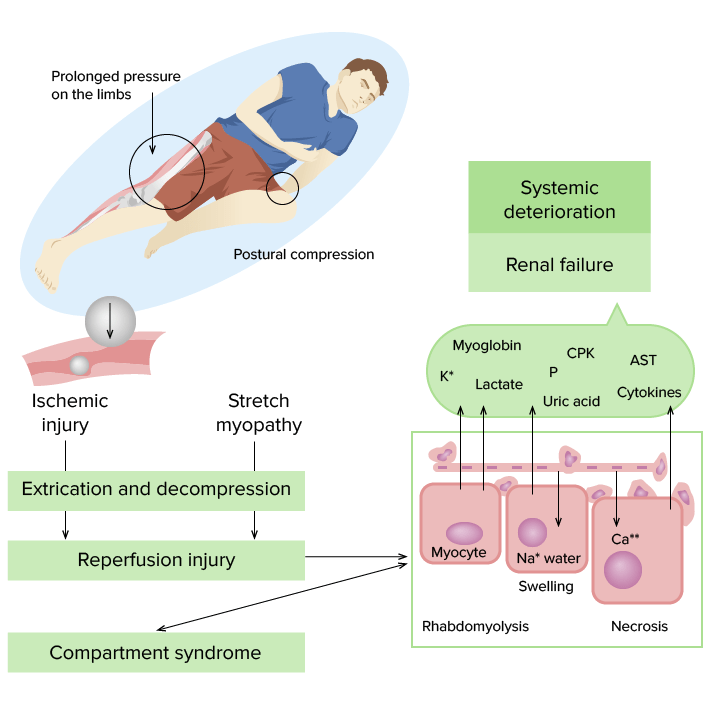
Pathogenesis of crush syndrome:
Prolonged pressure on the tissues results in vascular compression and tissue ischemia, particularly in the muscle. When the compression is relieved, a large release of cellular components occurs due to rhabdomyolysis, including electrolytes, lactic acid, uric acid, myoglobin, and creatine phosphokinase. These can lead to multiple systemic manifestations, including renal injury, hypovolemia, arrhythmias, and metabolic acidosis.
CPK: creatine phosphokinase
P: Phosphorus
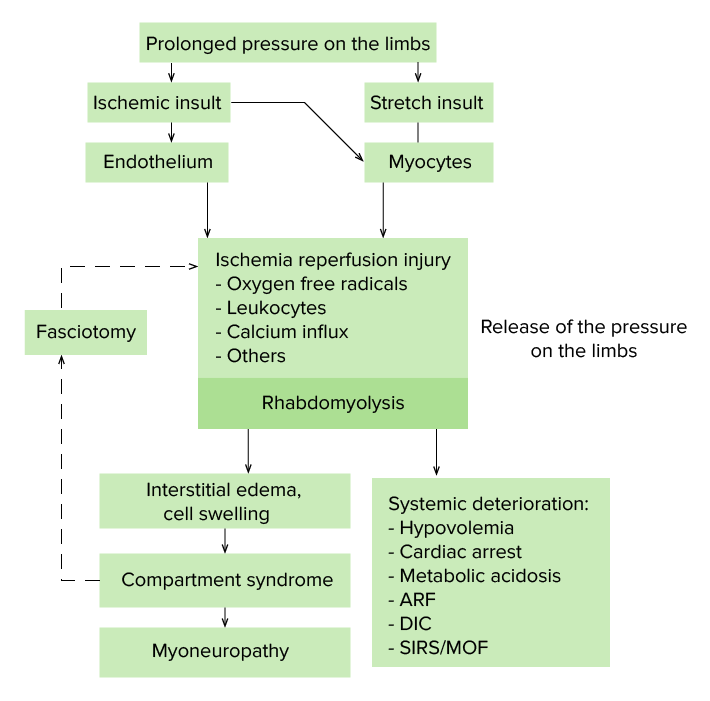
Pathogenesis of crush syndrome:
Ischemia reperfusion injury is the exacerbation of cellular injury and death due to the restoration of blood flow to ischemic tissues. There are many factors that play a role, including oxygen free radicals, calcium concentrations, endothelin, cytokines, and leukocytes. The resultant rhabdomyolysis can result in potential tissue swelling and compartment syndrome, as well as serious systemic effects.
ARF: acute renal failure
DIC: disseminated intravascular coagulation
SIRS: systemic inflammatory response syndrome
MOF: multiple organ failure

Chest blunt trauma: patient with crush injury with chest CT showing hemopneumothorax and bilateral pulmonary contusions (right more than the left)
Image: “Computed tomography scan” by ICU department, University Hospital of Alexandroupolis, Dragana, Alexandroupolis 68100, Greece. License: CC BY 2.0
Crushing injuries of foot and ankle: Image shows open fracture after initial debridement and fixation.
Image: “Open fracture of the ankle” by D.A. Edelstein and I. Florescu. License: CC BY 2.0